Peer support is more than the employment of people with lived experience in paid support roles; it is the employment of people who share some of the experiences of people using services (peers) specifically to draw on these shared experiences and ways they have found to live well (their experiential knowledge) – to provide support based on shared understandings, mutual problem solving, a belief in the possibility of recovery, and time together to find hope, solutions and connections.
17 ImROC Preparing Organisations PSW Briefing Paper outlines how organisations can enable PSWs to work to their full potential, to give careful consideration to the role: why are they PSWs? Who are they seeking to employ and how will recruitment and selection ensure that this is achieved? What is the role of PSWs? Where are they going to be employed to enable them to fulfil this role? How will they be supported, supervised and developed within the organisation? What structures are needed to enable them to have a collective voice so that they can influence improvements in the quality and effectiveness of services?
This guidance draws on research and guidance papers as well as the experience of PSWs and employers from NHS, Local Authority, third sector and voluntary sector organisations. It begins with the reasons why organisations might employ PSWs and why organisational preparation is so important, and goes on to provide guidance for organisations including: managers, team members/colleagues, Human Resources and Occupational Health, Learning and Development provision (for all staff), peer
supervision and support.
ImROC offers a range of peer support training and consultancy. We support organisations to employ peers within their workforce and train Peer Support Workers for their new role.
17. Preparing Organisations for Peer Support: Creating a Culture and Context in which peer support workers thrive
Julie Repper, Liz Walker, Syena Skinner, Mel Ball
Acknowledgements
We would like to thank Heath Education England (HEE) for funding the coproduction and writing of this paper. ImROC has previously written on this subject in our earlier Briefing Papers: Briefing Paper 5 Peer Support Workers Theory and Practice and Briefing Paper 7 Peer Support Workers: A Practical Guide to Implementation
1. INTRODUCTION
This paper provides information and guidance for organisations that employ, or are considering employing, peer support workers (PSWs). Peer support is a new role within many mental health services. It is not merely the employment of people with lived experience in paid support roles; it is the employment of people who share some of the experiences of people using services (peers) specifically to draw on these shared experiences and ways they have found to live well (their experiential knowledge) – to provide support based on shared understandings, mutual problem solving, a belief in the possibility of recovery, and time together to find hope, solutions and connections.
If organisations are to enable PSWs to work to their full potential, they need to give careful consideration to the role: why are they employing PSWs? Who are they seeking to employ and how will recruitment and selection ensure that this is achieved? What is the role of PSWs? Where are they going to be employed to enable them to fulfil this role? How will they be supported, supervised and developed within the organisation? What structures are needed to enable them to have a collective voice so that they can influence improvements in the quality and effectiveness of services?
This guidance draws on research and guidance papers as well as the experience of PSWs and employers from NHS, Local Authority, third sector and voluntary sector organisations. It begins with the reasons why organisations might employ PSWs and why organisational preparation is so important, and goes on to provide guidance for organisations including: managers, team members/colleagues, Human Resources and Occupational Health, Learning and Development provision (for all staff), peer supervision and support.
2. Why employ peer support workers?
There is increasing evidence that, where peer support workers are employed in a supportive environment with appropriate supervision and support, they contribute to improvements in the experience and outcomes of the people they support; they report benefits for their own recovery, and they can help to drive forwards a more recovery focused culture.
2.1 Benefits for people supported by peer support workers
In a recent review of the evidence about Recovery, Slade and his colleagues concluded that there is “substantially more randomised controlled trial evidence supporting the value of peer support workers than exists for any other mental health professional group, or service model”1. They summarised this research evidence as follows:
In no study has the employment of peer support workers been found to result in worse health outcomes compared with those not receiving the service. Most commonly the inclusion of peers in the workforce produces the same or better results across a range of outcomes.
The inclusion of peer support workers tends to produce specific improvements in service users’ feelings of empowerment, self-esteem and confidence. This is usually associated with increased service satisfaction.
In both cross-sectional and longitudinal studies, patients receiving peer support have shown improvements in community integration and social functioning. In some studies, they also bring about improvements in self-reported quality of life measures, although here the findings are mixed.
When patients are in frequent contact with peer support workers, their stability in employment, education and training has also been shown to increase.
NESTA and National Voices2 undertook a meta-analysis of a much broader range of over 1000 peer support studies and found that peer support is a term that includes many different approaches, contexts, components and beneficiaries. Nevertheless, the overall picture is one of benefit. They found that peer support:
- has the potential to improve experience, psycho-social outcomes, behaviour, health outcomes and service use among people with long-term physical and mental health conditions
- can improve experience and emotional aspects for carers, people from certain age and ethnic groups and those at risk, though the impact on health outcomes and service use is unclear for these groups
- is most effective for improving health outcomes when facilitated by trained peers
- is most effective for improving health outcomes when delivered one-to-one or in groups of more than 10 people
- works well when delivered face-to-face, by telephone or online
- is most effective for improving health outcomes when it is based around specific activities (such as exercise or choirs) and focus on education, social support and physical support
- works well in a range of venues, including people’s own homes, community venues, hospitals and health services in the community.
2.2 Benefits for peer support workers
While these findings indicate clear benefits for people who receive peer support, there is also evidence that peer support can benefit the peer support workers themselves. It brings all of the benefits of employment (pay, structure, social contact, self esteem), for some it is helpful to be able to ‘give back’ to services that have helped them or to contribute to the improvement of services; for others it is helpful to be able to contribute to others’ recovery, and for many becoming a PSW allows them to turn an often difficult experience into positive skills.
2.3 Benefits for Organisational Culture
At an organisational level, PSWs can drive forward a change in culture. They bring a different perspective into the workforce, they have not been trained or socialised into traditional practices, rituals, routines and beliefs but operate from their own experience.
This is invaluable in delivering services that are acceptable, accessible and effective for people using services: PSWs have been in this situation, they know what it feels like and given support, encouragement and appreciation of their perspective, they can contribute to the development of more sensitive, person centred and recovery focused practices, language, documentation and relationships.
Finally, the inclusion of peer workers in the workforce can be a powerful way of the addressing negative staff attitudes that still exist in places3. The most effective approaches to reducing stigma are those that include direct contact to allow both groups to identify and share their common humanity. Employing peer workers has been shown to work in this way, contributing towards more positive attitudes with higher expectations and greater hope for Recovery among staff4. Thus, peer workers can contribute towards creating an organisational culture that is more recovery focused.
3. Why Prepare the Organisation?
3.1 Creating a safe environment for PSWs
There are many reasons why organisational preparation for PSWs is essential. Of primary importance is the emotional and physical of safety of the peer workers themselves and the people with whom they work.
PSWs, by definition, draw on their own experience to support others. In order to do this, they are open about aspects of their life in ways that other staff rarely are. This places them in a vulnerable, potentially stigmatising position. Athough attitudes towards people with mental health problems have improved over the past decade5 too often assumptions are made about peer support workers based on ill-informed and negative beliefs about people who experience mental health conditions.
Research demonstrates that within the workplace context, people with mental health problems are perceived as less competent, dangerous, and unpredictable and that work itself is not good for these people6 and this is mirrored among healthcare providers who tend to hold pessimistic views about the reality and likelihood of recovery7,8.
This is particularly the case among those professional staff working on inpatient settings who rarely see people who use services other than when they are at their most distressed9. It is in these teams that attitudes show most improvement once peer workers are employed10, perhaps not surprising given working alongside PSWs gives them the positive contact that is known to improve attitudes. However, the potential for discrimination and the evidence that many existing staff with mental health problems do not disclose their condition for fear of repercussions clearly demonstrates the need for careful preparation before employing PSWs11.
Organisational preparation needs to ensure that all staff are aware of why PSWs are being employed, how they will be recruited and prepared, what employment conditions and sickness absence arrangements are for PSWs.
3.2 Gaining shared understanding of the meaning and purpose of peer support
Organisational understanding of peer support must go beyond practical considerations to recognise political and philosophical debates about what peer support means, how decisions about what PSWs do are integral to their identity, effectiveness and ‘fit’ in the organisation, and how the introduction of PSWs is not merely the introduction of a new role in the workforce.
Rather, it heralds new discussions and developments in organisational culture and practices. Peer support is underpinned by principles such as mutuality, equality, freedom, safety…. which cannot be implemented in settings where PSWs are expected to implement coercive, compliance-focused and restrictive practices.
This places PSWs in an impossible ethical predicament “either follow the organisational line and fail your own heart, or leave …”. Organisations need to consider how they can employ PSWs who are genuinely in a position to offer ethical and effective alternatives, otherwise there is a risk of organisations “using peer workers to create the appearance of recovery orientation, human rights compliance or community integration12” when this is far from the reality.
The employment of PSWs is only one way of working towards the development and delivery of recovery-focused, rights-based, person-centred, community-integrated services. If they are seen as the only way of changing services they run the risk of becoming crushed by the responsibility.
3.3 Ensuring shared understanding about the role of PSWs
The most common difficulty reported by both peer support workers and their non-peer colleagues is lack of clarity about their role. Both peer workers themselves and the staff with whom they work express confusion about what PSWs are employed to do and whether this should differ from the role of other support workers.
PSWs are not employed to deliver therapies or treatments based on professional training, nor are they employed to undertake all of the duties of non-peer care/support workers. They are employed to offer time, care, support, active listening, problem solving, ideas, suggestions and practical help within trusting, mutual, unconditional relationships with people using services – based on their experiential knowledge rather than on the traditional psychiatric knowledge taught to other professional groups.
While training for PSWs should provide clarity over how PSWs work (the values underpinning their approach), it is the organisation or team in which they are employed which needs to define precisely what is expected of them in that setting. In order to both create appropriate job descriptions, and to ensure that the whole team/organisation understands the nature of peer support, it is essential to provide all team members with information, preparation and time to discuss possibilities and opportunities for the team to define and understand everyone’s roles: the values and tasks that are shared as well as their distinct contributions. To date, most evidence of the impact of PSWs has been generated in settings where peer workers support transitions into and out of services, such as facilitating discharge or movement into community groups or employment, or into other services (such as transitions between Children and Adolescents’ services and adult mental health services).
However PSWs are increasingly working across the whole spectrum of services – forensic, substance misuse, intensive care, assertive outreach, crisis teams ….13 Wherever they work, it is essential for them and the team to respect their peer values and to support them to offer their distinct knowledge and skills to complement other members of the team.
3.4 Learning from peer led groups and VHSE organisations
The vast majority of peer roles exist within third sector and voluntary community groups, user led groups, self-help groups, housing services and organisations for homeless people. Much has been written about the risks incurred in ignoring the wealth of experience about peer support that has accumulated in these settings14.
Many of these groups have their roots in civil rights, in developing alternatives to psychiatric services, protesting against current practices and treatments, in believing in one another and finding ways forward through mutual support and solidarity.
They often have a closer understanding of the issues that are most important to people who experience mental health problems: issues like social justice, human rights, understanding diversity and appreciating the implications of traumatic life events, that are too easily overlooked in professionally led statutory services where greatest emphasis is often placed upon treating symptoms.
When organisations are preparing to employ PSWs, they are well advised to work in partnership with (other) user led and third sector groups within their locality, this can help to ground developments in first-hand experience and to resource and inform training, supervision and recruitment.
3.5 Enabling teams to understand and support PSWs role and contribution
Wherever PSWs are employed, team members need time to think through the implications of changing the relationship to a collegial relationship of equals. Often there is genuine concern for the wellbeing of PSWs, how they will cope with the demands of the work and exposure to others’ distress; how they will demonstrate/embody recovery and hope if they relapse at work; there is also concern about their ability to maintain professional boundaries and respect confidentiality when they are supporting people who are their peers – indeed they may be friends, or have shared time on an inpatient ward.
Team members need to be clear about how PSWs have been trained, recruited, selected and how they will be supervised. This cannot be achieved simply through giving information, it will only be understood through discussion and freedom to share personal views in a safe space.
Staff may also have concerns that PSWs won’t understand ‘why we do the things we do’: having first-hand experience of using services means that PSWs are likely to be sensitive to non-recovery focused practices and documentation, negative language, assumptions and ‘gallows humour’.
When employed in a context that welcomes feedback they can have a significant positive influence on team culture15. However, without preparation, team members may find feedback from PSWs difficult to hear and may become defensive. With preparation of the whole team, with time for reflection, discussion and development of a whole team approach to welcome and facilitate peer support workers to contribute to team development, team members can be supported to recognise the ideas and suggestions from peer workers as helpful and constructive.
Peer workers are trained to work within different relational boundaries from other staff. Since they will, by definition share more of their own stories, they are likely to hear more about the experiences of those whom they support. The team needs to prepare for this, consider what it means for the way they work, how they can value the lived and life experience of the whole team, how to share information and where confidentiality is critical.
Members of the team who bring lived experience of mental health problems may wish to undertake additional training on how to use their own experience appropriately and effectively in their relationships (although their role, power, code of conduct and professional source of reference means that they can never substitute for PSWs). Conversely, without careful preparation, organisations and teams can create a context in which PSWs comply with current practices, adopt the values and principles of other workers and lose their distinct identity, role and capacity to improve the culture.
3.6 Creating supportive, accessible and effective recruitment processes
Some people applying for PSW roles will have been out of paid work for some time – often many years. This can make the process of applying for a job, filling in application forms, completing DBS applications (police checks) and preparing for interviews stressful and off-putting. Care needs to be taken to recruit PSWs with a range of experiences and cultural backgrounds, recruiting from grassroots community groups, third sector organisations and services for groups that find services difficult to access – it is with these groups that peer support can be most effective16.
Personal support and information, feedback about the process as well as appropriate adjustments will help to make application less daunting and more accessible. Although this, once again, reflects good practice with all staff, it is often not available for any potential applicants and by improving HR and Occupational Health processes for peers, lessons can be learnt to improve the experience for everyone.
Once in post, support, supervision and development opportunities are essential. Training for PSWs is frequently quite brief and, as with many professions, learning really begins once they are in post. Accessible support on a day to day basis is helpful to reduce anxiety and answer questions as they arise, but peer specific supervision is essential to facilitate development and ensure that they maintain their ‘peerness’. Organisations need to make decisions in advance about who will provide managerial and peer supervision and how critical issues will feed back into organisational development, training available and specification of peer support roles.
4. Preparing the Organisational Context
4.1 Making Peer Support everybody’s business
Any organisation considering the employment of PSWs, needs to ensure that this is not a ‘niche’ discussion happening in one team; something that is slipped ‘under the radar’ in order to make it happen without the potential for barriers, or something that is considered insubstantial and a tick box activity to gain funding or achieve CQC approval.
The employment of PSWs does not happen as a separate, one-off event. It will trigger wide spreading ripples across the whole organisation, raising questions with far reaching implications. For example, an organisation cannot employ people specifically to use their own lived experience (PSWs) if it does not explicitly value the contribution of all staff who bring personal lived experience.
It is not enough to simply state that these staff members are valued, this has to be demonstrated in recruitment, selection and employment policies practices; managers need to be able to access training so that they can provide appropriate employment support; training must be available to clarify how these staff can use their personal experience safely, appropriately and effectively.
If implemented carefully, the employment of people with lived experience explicitly to draw on their own experiences in order to support others has the potential to significantly change the experience of people using services and shift the culture of the organisation.
If implemented without care and attention it has the potential to harm the PSWs employed, reduce the readiness of all staff to disclose their own lived experience, damage staff attitudes and belief in recovery, reduce the likelihood of recovery focused cultural change and ultimately it is people who use services who will suffer. It is preferable not to do it at all than to do it badly.
This means that the first step is to set up a peer support advisory group with membership from all levels of the organisation (for example, senior service manager, executive sponsor, HR/OH representatives, learning and development representative, user and carer involvement lead, service user representatives and where possible Recovery lead), and from any userled or peer support organisations working within the geographical system of services who can offer experience of employing PSWs.
This advisory group needs to make itself aware of what PSW means, the potential benefits and pitfalls, organisational requirements (eg for development of new training courses) and implications (eg for funding of project lead, funding for new posts, review of employment support for staff with mental health challenges).
At an early stage, the decision can then be made about whether the organisation is ready to embark on this process or not, and if they are, who else needs to be invited to join the advisory group (eg local voluntary and third sector peers; experts from other organisations with prior experience, team leaders where peers may be employed …) and who will take on the role of project manager.
4.2 Board level support for peer support workers
Even at this early stage, there are potential action points for all members of the steering group. Since the employment of PSWs is a significant decision with wide ranging ramifications, the Executive Sponsor for PSW (or a designated link person with the board) will need to present a proposal to the Board and both ask and answer questions from the Board.
Of primary significance is Board level recognition that the employment of PSWs signifies that the organisation recognises the benefits and value of experiential knowledge. At Board level, it is essential to consider what this means for organisational strategy and whether changes are required to ensure that this message is clear and consistent in all aspects of the organisational vision and strategy.
The employment of PSWs is a necessary but in itself insufficient element of overarching transformation towards services in which relationships between service providers and service users become more equal as they work more collaboratively in shared decision making, coproduction, collaborative care planning, joint safety planning and cultural shift towards valuing the preferences and wishes of people who use services.
If there is no organisational commitment to this overarching shift then the opportunities for PSWs to work in distinct person focused, experientially informed ways is likely to be limited to a role in which all that is shared between peers and those they support is their mutual powerlessness. Alternatively, if the organisation is prepared to value the perspective of PSWs and people using services, opening itself to new ideas and willing to try innovative coproduced practices, then the pool of resources available is expanded to include all those using services17; practices become more recovery focused and the experience and outcomes of people using services are likely to improve18.
4.3 Funding
An important element of organisational commitment to PSWs is allocation of adequate funding. PSWs employed within an organisation must have the opportunity to apply for paid posts, banded according to job descriptions. They are not a cheap alternative to professional staff, they are an effective complement to multidisciplinary teams. As with any professional group the PSW budget needs to cover costs of developing PSW training, preparing teams, providing supervision, and professional leadership.
4.4 Leadership
It will take time for numbers of PSWs to reach a critical mass – able to present a case or provide effective support – within a single organisation. This makes the appointment of a peer support leader essential. It cannot be assumed that PSWs will be appropriately led by other professional leads.
Peer Support arose in a totally different philosophical and practical tradition; one which largely developed as a response to poor treatment and neglect within services19,20. It may be helpful for an existing user and carer engagement lead, or a Recovery lead to be appointed to lead the development of peer support but thought needs to be given to the experience and capabilities of the appointee. A peer support lead must bring their own lived experience and demonstrate appropriate and effective disclosure of this, ideally with working experience as a peer support worker themselves. More information on this can be found in the Thought Piece on Career Pathways for peer support workers.
They need to understand the politics and practice of peer support and have strong links with networks of peers locally and nationally.
But they also need to understand how organisations and traditional professions work. They need to have excellent communication skills to gain the respect of other professions and above all strong leadership skills to take forward new peer roles and enhance their influence across organisational culture (see Case Study 3).
This is a demanding and potentially isolating position as a central aspect of the role is to provide challenge at all levels (including the Board) from a lived experience perspective. There are organisations that recruit service user/peer leadership from external organisations, this has the advantages of proving a more independent voice when challenging the system; however the person may feel of a lone voice if they operate from within a separate organisation; they can discuss, test and develop a service user perspective within a collective of peers (see Case Study 1).
Case Study 1: Trust wide Lived Experience Practitioner & Peer Support Lead role within Central and North and West London NHS Foundation Trust (CNWL)
My role as Trustwide Lived Experience Practitioner & Peer Support Lead for a large NHS Trust in London is nothing if not large and varied. I hold responsibility for the strategic development of our workforce, which includes developing infrastructure, and advocating for the creation of new roles.
I also supervise a large (and growing!) team of senior peer support workers and advanced lived experience practitioners, and co-deliver our Level 4 accredited ‘Developing Expertise in Peer Support’ training at London South Bank University. I frequently present our services both internally and externally, and liaise with stakeholders, such as colleagues within other professional groups, HR, recruitment, volunteering, service user and carer involvement, our employment services, and the Recovery and Wellbeing College. Much of my work, therefore, is about building relationships and communicating vision.
I am amazed at how critical my previous experiences of working within a variety of peer roles serve me day to day. Prior to my current role, I have worked across both inpatient and community settings, in both statutory and User Led Organisations and the third sector. This varied experience of peer roles across my career feels absolutely integral in being able to provide credible, and experientially informed leadership to my colleagues.
Furthermore, I often speak about holding a caseload of one – my organisation.
At CNWL we define recovery as “the purposeful pursuit of a good life, irrespective of the absence or presence of symptoms, organised around the pillars of hope, opportunity and control, with social inclusion and self management at the heart.”
Much like many of us who have experienced mental health difficulties, my organisation has come a long way and done well in working towards developing a focus on recovery. However, it is on an ongoing journey of recovery, which we all know is a non-linear journey by nature. From having skills honed in ‘front facing’ work, I am able to think about how to use myself, a relational way of thinking and some smatterings of self disclosure to support the system to consider another way of considering its contemporary circumstances.
Using a similar approach to staff supervision, I work by focusing on sharing a relationship where we can both learn from each other, neither of us is positioned wholly as the expert, though we have different useful perspectives to communicate and tasks to achieve in our respective roles. This allows an ongoing development of this perspective and keeps alive my skills as a lived experience practitioner. I am always keen to learn from my colleagues, and I usually find that my grounding in approaching people I work with as keepers of their own wisdom fosters a mutually curious and open way of us both relating to each other.
5. Organisational Preparation: A checklist of questions to address
Any organisation planning to employ PSWs will need to consider a number of key questions. These are summarised below and more information to inform responses is provided in the following sections.
What do you want to achieve by employing PSWs? (see Section 3) As an organisation are you committing to working in partnership with people who use services in every way possible? Are you employing PSWs to demonstrate your belief in people who have experience of mental health challenges? To improve the experience of people using services? How are you going to make this commitment understood, shared and ‘real’?
How will PSWs be employed? (see Section 6.1) There are various different models for employing PSWs and no conclusive evidence about which works most successfully. Have you considered whether you will work in partnership with an external organisation to train, supervise and/or employ PSWs, or whether you are going to employ them in house? (see section 6 for more details about different options).
Where will PSWs be employed? Are you working towards employing peer workers across the whole service, one part of the service, or one team…? Where are you going to start and what is the goal? This may be informed by where funding is available, where new services are being developed, where quality improvement initiatives are being implemented.
However, decisions made by managers about where, how and how many PSWs will be employed are unlikely to be as successful as engagement with teams about what peer support is, what it can achieve, whether they are interested in employing PSWs on their team. It is essential to include members of teams where PSWs will be employed in the planning process, ideally as members of the advisory group. The employment of two or more PSWs in each team is strongly advised so that they are not isolated and have some mutual support from other peers whilst they are carving out a role and a distinct identity for PSWs in the team.
How many posts will be developed? Whilst it is advisable to start with a small group of PSWs so that sufficient care can be given to refining processes and support mechanisms, the PSWs will feel less isolated and alone if the first group includes around 12-18 peers.
This allows mutual peer to peer support, meaningful experiential learning, sufficient numbers to have a collective voice and a sense of solidarity – and it thoroughly tests processes and practices from the start. Some PSWs do not feel ready for full time posts from the start of their employment so, as a rough guide, it is likely to be necessary to train up to 18 PSWs to fill 6 FTE posts.
How will PSWs be recruited, selected and supported during and following the application process (see Section 7) Decisions need to be made about HR leadership for the safe and effective recruitment, selection and employment (support) for PSWs, including occupational health support.
How will PSWs be trained? (see Section 9) Provision needs to be made about the training of the first cohort of PSWs and then for ongoing learning and development of this cohort as well as new recruits.
How PSWs will be supervised (see Section 10) Since peers are much more likely to retain their peer identity and role if practice supervision is offered by an experienced PSW, arrangements need to be made for this to be offered whether in-house (possibly with support or through an external organisation), or by an external organisation from the start.
How will development opportunities be created for PSWs? (see Section 10) Consideration needs to be given to the ongoing career pathways for PSWs, opportunities need to be developed within the organisation for PSWs to progress into (eg senior peer roles, team leader roles, lived experience practitioners, peer specialists). In addition, PSWs bring lived experience to the whole organisation and some of their time might be set aside for coproduction activities alongside the user and carer involvement service or for developing coproduced learning opportunities either in the Recovery College or in staff learning and development courses.
How will existing staff with lived experience be supported? (see Section 9) The employment support provided for PSWs should not be exclusive to these members of the workforce but must be extended to all staff members so that everyone can work to their full potential and stay well in work21. Additionally, although PSWs are employed specifically to draw on their experiential knowledge, many other members of the workforce will have experience that could be used in their practice to enhance the support that they provide. This has implications for Human Resources, Occupational Health, Learning and Development and managerial roles.
How will observations, perspectives and suggestions of peer workers be responded to? (see Section 11). PSWs are employed not only to support people using services, they also bring a different but equally valued perspective to services and service development. Whilst individual peers working in teams might find it difficult to make their voices heard, a forum where PSWs can join together to share experiences, develop their views and suggestions and take them forwards for consideration by relevant forums is an important indicator of the real value that is afforded lived experience.
Who will employ, train and/or supervise the PSWs working in your organisation? Peer support has its roots in peer run organisations and where there are local peer run organisations it is essential to work in partnership with them to ensure that the original values and principles of peer support continue to inform PSW practice. Without this, PSWs too often become no more than ‘peer staff’ who end up complying with traditional psychiatric practices rather than bringing their distinct and unique peer contribution.
The experience and solidarity of peer led groups not only support the integrity of peer practice, they can also provide a safe place for PSWs to share their experiences, discuss challenges and develop responses. However, employment in paid roles within large, often statutory organisations does bring different challenges, expectations and limitations. The governance, bureaucracy, hierarchies and power relationships within these organisations can make the employment of PSWs a tightrope act – trying to retain peer principles within settings in which many people using the services are highly distressed, may be on involuntary sections of the MHA, where (professionally defined) safety is the priority.
While partnership between peer-led organisations and statutory organisations is always preferable, decisions have to be made about where and how PSWs will be employed.
6. Who will employ, train and/or supervise the PSWs working in your organisation?
6.1 Employment of PSWs by an external peer support organisation.
The training, role, employment and supervision is all undertaken by an external (peer-led or experienced in peer support) organisation and PSWs are placed in posts in a mental health service. This requires close collaboration between the two organisations so that expectations are consistent. Communication needs to be clear to anticipate and prevent problems arising, pathways for conflict resolution need to be set up in advance. (see Case Study 2)
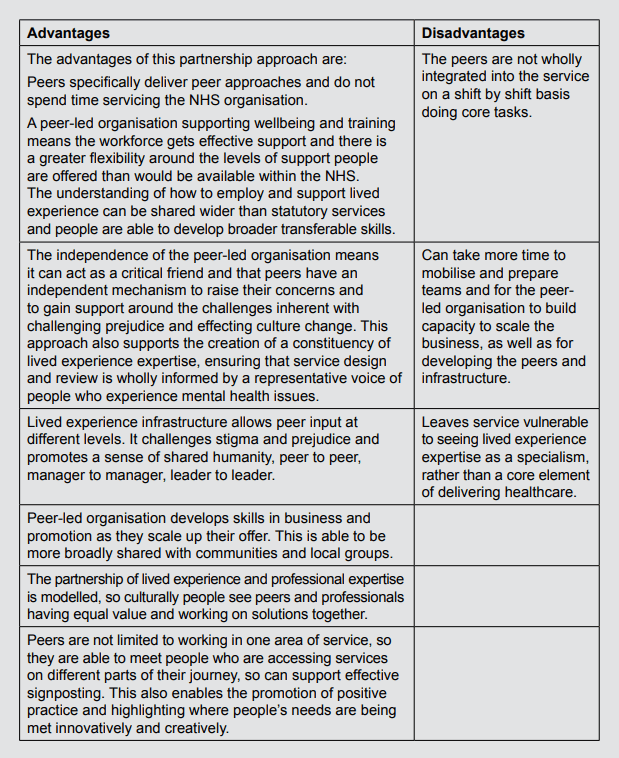
Case Study 2: Dorset Wellbeing and Recovery Partnership
Dorset Healthcare University NHS Foundation Trust and Dorset Mental Health Forum have been working in partnership, as the Dorset Wellbeing and Recovery Partnership (WaRP), for the past 10 years. At the heart of this Partnership has been the exploration of lived experience and clinical expertise co-existing to provide a range of perspectives.
Dorset Mental Health Forum is a local peerled organisation, employing approximately 80 people all of whom have their own lived experience of mental health challenges, or that of supporting partners or close family members. The aims of the Partnership are to change the culture of mental health services and promote wellbeing across the whole of Dorset. Through this work, the Partnership promotes and models shared humanity and the belief that Recovery as a philosophy is common to us all.
In Dorset, peer specialists are independently recruited, employed and supported by the Dorset Mental Health Forum and they then work into Dorset HealthCare. Peers work at different levels into inpatient settings, CMHTs, CAMHS, specialist services (such as Forensic, Perinatal), the Retreats (open access crisis service), Learning and Development, and the Recovery Education Centre. The Forum do not just provide peers to deliver services, but also work strategically on the Mental Health Integrated Programme Board and at team leader level to support service development, as well as influencing at Board level and as system leaders within the local Integrated System (ICS).
The Forum has developed a career structure, referred to as a lived experience infrastructure with peer specialists, peer coordinators and lived experience lead posts. Over the past 10 years, the Partnership has been able to test and demonstrate that this independent way of working adds value and also provides an additional mechanism for peer support within the organisation itself. Much of the work independent peers do, includes compassionate challenge and building a sense of collective community informed from a range of perspectives.
The work is underpinned by a codeveloped partnership agreement, which acknowledges both organisations as stakeholders and partners in decision making and planning. This enables explicit conversations to happen around power and the direction of services. The partnership agreement also covers how risk is managed, data sharing and confidentiality.
Before peers work into a new area of service, the Dorset Wellbeing and Recovery Partnership leadership team (with a representative from the Forum and a representative from the Trust) engage in some team preparation and culture focused work. This also provides an opportunity to provide assurance of how peers are supported to do their work. Wellbeing at Work plans and Advanced planning documents are discussed, as well as details and descriptions of ongoing training, supervision and support mechanisms that are in place.
It is often important to teams that they are able to explore how they can build capacity from within their own services, so we discuss how we might engage with people who have previously accessed their service and how a pathway may be developed.
6.2 An external organisation provides the whole service
The whole service is commissioned from a peer run organisation which runs independently. (see Case Studies in HEE thought pieces on a) Crisis Services where the Cellar Trust is commissioned to provide peer led services, and b) VCSEs and Peer Support).
6.3 The organisation recruits, trains and employs its own PSWs
The organisation that wishes to offer peer support develops systems and processes for recruiting, training, employing and supervising peer support workers. PSWs are employed either in selected multidisciplinary teams or from a central peer support team. Wherever peers work, staff are given preparation so that all members are clear about the role and employment conditions of PSWs. Practice supervision is provided by peer supervisors (who may come from external organisations) whilst their team leader provides managerial supervision as with other members of staff. (See case study 4)
Case study 3: Central & North West London NHS Foundation Trust
In 2009, as an ImROC Pilot Site, CNWL began its journey to transform our workforce through establishing peer support activities in a statutory service at a time when such an endeavour was considered innovative. As an organisation, with executive support, we aligned the development of our Recovery College and peer support to work closely together. Subsequently the staffing resource for both was strongly linked; peers were trained together via an in-house provided training programme, and initially some staff worked across both workstreams – as both peer trainers and peer support workers.
As time has gone on, we are glad to have initially ventured forward with the model of in-house employment. The influence of peer support workers being embedded within the organisation has paid dividends in terms of our organisational culture shifting towards a recovery focus.
Though there is still work to be done, one of the huge benefits of all peer support workers being employed directly by CNWL, is the way in which ownership and pride for these roles is rooted in many colleagues at all levels of our organisation. It is hard to say whether we would have quite the same level of support for the work we are doing to improve, upscale and innovate, if our efforts were all located within an external partnership organisation.
We have found that what follows embedding peer support organisationally, is broad support for the recovery focused agenda. Issues that peers advocate for, such as coproduction, informed and shared decision making, reducing restrictive practice and trauma informed care for e.g; are increasingly being considered ‘everyone’s business’.
Additionally, the feeling of ‘us and them’ between peer workers and other colleagues is reduced as our staff feel the benefits of working alongside their peer colleagues. As ‘mentally healthy’ workplace cultures are required for our peer workers to thrive, our working practices and policies continue to evolve with benefits of improved workplace wellbeing and job satisfaction for all staff.
Some NHS Trusts have successfully achieved a similar level of embedded presence via strong partnership working with local VCSE’s. For us at CNWL however, considering the sprawling geography and size of our Trust, we feel our peer workforce, located within the organisation, allows us to effectively work collaboratively across the whole organisation. In such a large organisation it is critical that our peer colleagues are not forgotten or undervalued. By developing an in-house workforce; we work alongside each other, ensuring delivery of services that reflect our Trust’s values.
7. Human Resources and Occupational Health issues
7.1 Developing the job description – what will PSWs do?
It is advisable for the whole PSW advisory group to be involved in determining the role of PSWs by contributing to the development of their job description. There are critical decisions to be made about what will be expected of PSWs. It is helpful to start by reaching agreement about how your organisation wants to define peer support, what you want to achieve by employing PSWs and how their job description can be crafted to stay true to your goals.
The literature suggests that peer support workers make at least three distinct contributions that differ from other staff22. The first is the development of a relationship characterised by mutual understanding, acceptance, trust and a genuine belief in the person’s ability to recover. The second is the inspiration of hope through self-disclosure; demonstrating that it is possible to gain control over mental health challenges, from being defeated and disabled by the condition to understanding it and believing that it is possible to live well in spite of, or even because of the condition.
The third lies in sharing experiences within this trusting and more equal relationship, exploring ways of coping and managing the condition and life more generally. This might include identifying life goals and working out steps to achieving them, it might mean problem solving together, developing a personal recovery plan, or practical help to address barriers – both within services and the social situations that stand in the way of living well – things like debt, poor housing, relationship problems.
While PSWs might not have the answers to these problems, their job description needs to allow them to spend time with people, help them gain understanding, work out what their experiences mean to them, work with them to think about what they want, find out what is available, what might help them, and then to take action together.
Having agreed on the purpose of PSWs in the organisation, it can be useful to look at a range of job descriptions developed by other organisations and then to consider key questions about the role of PSWs in relation to certain tasks and whether they will they be included in the ‘numbers’ on a shift.
Will PSWs be expected to undertake the routine duties of other support workers (like making beds, serving meals…) or will their role be confined to supporting Recovery through one to one support, running groups, coaching, recovery planning, goal setting, action planning….?
There are different ways of addressing these questions. Whilst the question of whether PSWs will be included in the ‘numbers’ is largely informed by finances, questions about the nature of their role are largely addressed by considering the values underpinning the role. PSWs are not employed to carry out tasks and duties defined by other professionals but to engage with people in a mutual and reciprocal manner. They may be able to achieve valued relationships whilst undertaking such tasks as making beds together, attending meetings together, taking a walk together or planning action together, but these tasks must not take precedence over relationship building and peer support.
More contentious questions must be addressed in relation to the role of PSW in coercive practices: the values and principles of peer support mean that PSWs should not take part in restraint or in giving medication – or other treatment – against a person’s wishes.
However, there are ambiguous situations in which a PSW may be involved in preventing a person from harming themselves or someone else; they could have a role to play in reducing a person’s distress, de-escalating a crisis, taking them for treatment that they have agreed to but may well be frightened about…. It is essential that a wide range of stakeholders are involved in discussions about the role of PSWs in your organisation so that a deep understanding is achieved and well justified decisions are made.
7.2 Person specification – what do you mean by ‘peer’?
One further crucial question to be considered relates to the person specification: what do you mean by ‘peer’? Whilst PSWs working in mental health services might be expected to have personal experience of mental health problems, it is important to think about how this will be defined. Will people define themselves as having this experience or will they be expected to have used services? if so, will they need to show they have used primary or secondary services? Will you consider people who have sought personal therapy to have the shared experience necessary to provide peer support?
Given that so many people using mental health services have experienced trauma, homelessness, poverty, unemployment … will these factors be taken into consideration when recruiting PSWs? Will your definition of ‘peerness’ depend on the service that you are recruiting to? For example, when recruiting PSWs for forensic services, will PSWs be expected to have used forensic services? When recruiting PSWs for homeless services will they be expected to have experienced homelessness and/or mental health problems?
An advisory group which includes people with a range of experiences, perspectives and a deep understanding of peer support will be helpful in reaching well justified answers to these questions.
7.3 Recruitment
However many peer support workers will be employed and in whatever part of the services, consideration needs to be given to the recruitment and employment process. Since PSWs bring added benefit for the engagement and recovery of people who find services difficult to engage with, it is advisable to recruit some PSWs from groups who themselves have difficulty accessing and engaging with services.
Recruitment needs to reach people who have experience of adverse life circumstances and mental health problems who are no longer using services, so advertisement of posts needs to go beyond NHS Jobs to provide relevant and accessible information to local voluntary sector, local authority and primary care groups and services.
For recruitment processes to be accessible, it is helpful for clear and welcoming advertisements to give the name and phone number of someone to call if they are interested in finding out more about the post. Calls must be returned quickly and supportive – and honest – responses given to inquiries. Peer support is not an easy job, it is not well paid and it does require people to talk about their own experiences.
However, if you want to use your experiences to help others, if you have found ways of managing your own condition and living well, then it might be for you.
The application process for large organisations can be a deterrent in itself. It requires access to a computer and the internet, a high level of literacy – and it asks questions about past employment and experience. All of these might be particularly difficult for people who could make very good PSWs.
It can therefore be helpful to offer individual support to people interested in applying to become a PSW, enabling them to access the right form and giving them the confidence to respond to questions appropriately. This might be undertaken by a member of the HR team or the employment support team, or once there are PSWs in post, it might be possible for a member of the PSW team to provide this support.
7.4 Selection
Just as applicants for PSW posts have often had little experience of applying for work, they may also find the prospect of an interview very anxiety provoking. It can be helpful to arrange a selection process that allows applicants to demonstrate their skills, values and behaviours in different scenarios.
An assessment centre approach in which all shortlisted applicants are given the opportunity to meet, ask questions, take part in a large group discussion, answer selected challenges in a small group and take final questions in a brief individual interview can be a more effective approach to selection. It is essential for the selection team to include at least one person with lived experience, ideally already in post as a PSW, and for an HR representative to sit on the panel to answer questions about process and expectations, as well as a service manager/team leader from the service the successful applicant will work in.
As with all recruitment, it is necessary for the panel to agree set questions and criteria beforehand. In order to work well as a PSW, applicants do NOT need to be symptom free, but they do need to demonstrate an understanding of their condition, what they do to keep themselves well, how they know when they are not so well and what they do when they need additional support.
Indeed, it is the learning that has occurred through their own experience that will be most helpful in their role as a PSW, so selection does need to assess what they have learnt and how this might enable them to support another person. Since peer support is built on strong values, it is helpful to observe group discussions and problem solving for evidence of applicants’ values in action.
All applicants, whether they are offered a post or not, should be given feedback so that they are clear why they were successful or unsuccessful and for those not offered a post, support should be offered to enable them to develop their skillset (for example an introduction to Recovery College to learn more about personal recovery planning, an introduction to the Volunteer team for opportunities to gain more experience in supporting others).
7.5 DBS checks
For people who have been involved in the criminal justice system during difficult periods in their life, the prospect of completing a police check form is yet another barrier to negotiate. Personal support and information can help them to see this as just one part of the process of applying for a job. However, at an organisational level, the employment of PSWs may well trigger a review of the DBS checking process.
7.6 Employment support
The introduction of peer support workers in the workforce provides an opportunity to consider and develop new strategies, policies and procedures for the benefit of all staff. Line managers and leaders should be supported to adopt a zero tolerance towards discrimination. Policies as part of a wider plan to implement and communicate the importance of wellbeing could be introduced.
- Occupational Health assessments are a routine part of NHS and larger organisations usual recruitment processes. While they are designed to assess the health needs of a new employee and offer support to fufill the duties of their new role, they can be particularly anxiety provoking for peers who may have been denied employment because of their health condition or been “retired” from previous employment due to their health condition.
The success of these assessments depends on the level of understanding of the person carrying out the assessment ie do they understand the role? Do they understand the duties expected? Do they appreciate/ understand why the person may not have been in work previously. It is Occupational Health who will make recommendations about reasonable adjustments, again the nature of the adjustment recommended will depend on the OH professional truly appreciating the role and context in which the person will be working.
- Reasonable adjustments. Employers have a duty of care under the Equality 2010 and Reasonable Adjustments DWP 2017 give some guidance on employing people with mental health conditions. DWP suggest flexible work patterns, changing the work environment where possible, creating action plans to help manage their condition and allowing leave to attend appointments and so on as helpful strategies but these do not go far enough. Reasonable adjustments can and should be made throughout the recruitment process as suggested in 7.3 and 7.4 of this paper to ensure peers are supported appropriately to successfully apply for roles and survive and thrive in work.
- ‘Wellness at Work’ plans. Peer support workers benefit from understanding how ‘Wellness at Work’ can help them in their employment, so this should be an integral part of their training as well as part of a more general approach to having open and honest conversations about mental health in the workplace (something which all staff would benefit from). A wellbeing plan helps to build a picture of why a person may react in unexpected ways to situations and enables support to be provided based on shared understanding, regularly reviewing the plan is important and can be done as part of ongoing supervision.
- Occupational Health Support. Ongoing support from OH may be necessary for the peer support worker to remain in work. OH may be best placed to recommend and signpost PSWs (and others) to additional support Eg Employee Assistance Programmes, and initiatives like the “Green Hour” implemented at CPSL MIND that encourages all staff to have an hour a week in “work time” to play sport go far a walk, read a book etc.
7.7 Financial considerations for peer support workers
Due to the complexities and individual nature of our current benefits system we would recommend that ALL peers applying for peer support worker role should seek individual benefit advice.
Many peers work part time or on “bank” arrangements which further complicates how peers can be paid and employed. Some peers choose to begin their employment under permitted work and assume that they will be able to work for 16 hours and earn under a set amount per week that is usually 16 hours times the national minimum wage.
For entry level Agenda for Change band 3 PSWs this isn’t the case. The hourly rate of pay for a band 3 PSW is higher than the national minimum wage which means currently peers are only able to work about 12 hours / week to meet the requirements of permitted work.
Again, we would advise seeking the advice of an employment advisor if you have access to one or the Disability Engagement Officers at DWP. NHS Trusts will have access to pensions advice to support peer support workers to think about their future pension and to understand the importance of national insurance contributions in safe guarding their future financial security and we recommend that PSWs are encouraged to meet with their advisor as part of their induction programme.
Trusts are used to employing staff who are managing long-term conditions or have a disability, and, therefore, it will be helpful when employing PSWs for the first time to apply similar “rules”.
8. Team Preparation
The success of PSWs is largely attributable to the teams in which they work. Where the team understands why PSWs are being employed, how they will contribute and what additional specific support they are able to offer to people using the service PSWs can settle in without confusion, negative judgements or blame. Where team members actively seek out PSWs to provide mutual support to people who are isolated, disengaged, inactive or experiencing distressing experiences, then peers use their skills in a targeted way, they feel valued and appreciated by staff and people using services and given support and supervision they will enrich the team, improve the experience of people using the service and develop their own skills and confidence.
8.1 Team Preparation workshops
Once decisions have been made about where PSWs will be employed, then each team needs some careful and bespoke preparation. Where possible the whole team (including all professions and non-clinical staff) needs to spend at least half a day sharing, learning and planning together.
The session needs to be facilitated by the peer support lead, a senior service manager and a peer support worker. It is helpful to cover the following areas in an experiential, non-judgmental, and developmental manner and to create a safe space for all participants to contribute openly23:
- Peer support: What is meant by peer support, what is a PSW, what do they do, what difference do they make (input by PSW lead).
- What are the hopes and fears of team members about a PSW joining their team (generation of ideas to be done confidentially so that participants can be honest) (exercise facilitated by PSW trainer)
- Which of these fears can be addressed here and now? What further information is required to address all the concerns raised? (Manager to lead discussion of feedback)
- How can the team ensure that all their hopes about PS are realised? (Manager)
- What is the role of PSWs in a team like this (PSW lead drawing on examples from literature and practice)
- How will this work in your team? How could a PSW enhance the support that you offer? (exercise facilitated by PSW trainer) Collect a team specific list of PSW tasks/duties
- How can you, as a team set up processes and support to enable your PSWs to work to their full potential (eg how to refer/ engage PSWs in specific work with people using the service; identifying a mentor for PSWs…) (exercise facilitated by PSW lead)
- Making an Action Plan, identifying who is responsible for what and when.
8.2 Can PSWs work in any mental health team?
Since PSWs bring experience of using the whole range of mental health services (some have used acute inpatient services, some community, some substance misuse services, others child and adolescent or forensic services; some have avoided using services but have sought different types of support , therapy and/or treatment …. ), in theory they can be employed to work in any of these services so long as they potentially share some of the experiences of people currently using those services.
However, it is particularly challenging for PSWs to be employed in very traditional, hierarchical or coercive teams where there are no plans or attempts to introduce more Recovery focused practices. If a PSW is employed in a team where there is frequent restraint, where the emphasis is on giving medication and treatment against the will of people using the service and where there is little attempt to share decision making or facilitate personal Recovery planning, then PSWs will not be able to work in a manner consistent with their role.
Too often, PSWs employed in contexts such as this become disillusioned, frustrated, burnt out; it is not fair or ethical to place them in contexts which will either be bad for their wellbeing – or require them to adapt and adopt accepted practice.
This is why the introduction of PSWs cannot be a standalone initiative: the only intervention implemented to challenge current practice. This places huge responsibility on individual PSWs and essentially sets them up to fail in their role. Organisations introducing PSWs need to consider how other initiatives might support and strengthen the influence of PSWs in changing the culture of the organisation.
8.3 Team Recovery Implementation Planning (TRIP)
One approach that complements the introduction of PSWs in teams is Recoveryfocused quality improvement using the TRIP as a set of benchmarks for the team to assess themselves against, identify 3-5 priorities for action, and agree a comprehensive team recovery action plan that can be reviewed regularly.
The introduction of TRIPs to improve the Recovery focus of teams has been a CQINN target in a number of areas (including high secure services) and used in outcomes-based commissioning. It is worth considering the use of TRIPs in organisations where teams are not actively working towards Recovery before employing peer support workers24.
8.4 Ongoing support for teams employing PSWs
A single workshop to prepare a team for PSWs is unlikely to provide sufficient understanding of what will be required, nor will it facilitate the ongoing development of structures to support and develop PSWs in practice.
Where PSWs are employed, team leaders need to have access to support, problem solving, coaching and development to enable them to continue to develop a supportive context for PSWs and to manage any challenges that occur in an appropriate Recovery focused manner (see also Section 9).
9. Learning and Development Opportunities to support the employment of PSWs
9.1 Training in peer support
It is essential for all PSWs in paid roles in organisations to undertake high quality training in peer support that enables them to understand the values and principles of peer support, implement these in developing relationships and to work safely, appropriately and effectively. Organisations may wish to access PSW training provided by respected organisations, and they may wish to work with these organisations to develop their own PSW training course.
HEE is currently working with UCL partners and the NCCMH to develop and approve a competency framework for PSWs which clearly outlines the areas to be covered by training. Once this has been ratified, trainers will have a shared consistent and agreed framework to inform the development of training. (Contact HEE for information about training providers.)
A number of different organisations offer PSW training at different levels, some accredited, some not. (See ImROC Training Prospectus and ImROC Peer Support Brochure).
Case Study 4: PSW Training provided by ImROC
ImROC coproduced the first training course for PSWs working in NHS services in 2008 working with local peer led NGOs and drawing on an extensive review of the literature. This course has developed over the past 12 years and is now offered as organisational development support rather than simply a training course.
A team of experienced peer and professional trainers (from statutory NHS, LA, and Voluntary Sector services) work with organisations interested in employing PSWs to ensure that they have a full understanding of what this means, why they are embarking on it, and whether they have the funding, structures and culture necessary.
Support is offered at organisational level, with teams where PSWs will be employed, with Learning and Development Departments and with HR departments to develop a training and development plan fit for their organisational context.
This includes support with selection and recruitment of trainees, organisation of pastoral support during training, preparation of placement mentors and delivery of a ten day training course with additional specialist modules for PSWs working in specialist placements; assessment of competency of PSWs and advice on employment support.
ImROC offers an accreditation system which examines the organisational context including training and is renewed annually following annual peer review.
9.2 Training before or after employment?
Organisations need to decide whether PSWs will be employed and then offered training, or recruited to training which enables assessment of their competency and readiness to work before they are recruited to a post.
The advantage of offering training prior to employment is that it enables the student to fully understand the nature of the role and gain experience of working as a peer support worker during a student placement; it ensures that they have the skills and understanding to keep themselves and those whom they support safe; and it offers the organisation greater confidence in the ability of the recruit to undertake the work.
Since other professional groups undertake training prior to employment it seems to make sense.
9.3 Ongoing development of PSWs
PSW training only provides the basic knowledge and skills for peer working. As with any job, most development takes place with practical experience over time, and further training is necessary to gain more advanced and/or specialist skills.
PSWs may wish to learn more about Recovery and Wellness Planning, Coaching Skills, Problem Solving, Co-Reflection, Community Development, Peer-to Peer supervision, Supporting family members, Training to be a trainer, Survivor research skills, and more.
These training needs may be identified in their personal development plan, supervision or appraisal system – (importantly all primarily based on and informed by their own experience). Whilst some of these courses will be relevant and available to all staff, others will be specific to PSWs. Organisations need to plan ways of enabling PSWs to access appropriate ongoing education – either through inhouse courses or in the Recovery College (if there is one locally) or by accessing external trainers.
There is often a period of time when organisations are building their capability in peer support and investing in the development of staff who will become peer supervisors, peer trainers, peer researchers and senior PSWs as the peer workforce expands (see HEE paper on career pathways).
9.4 Offering relevant courses to all staff
The employment of PSWs is only one way of shifting the culture of services. Organisations that employ PSWs need to ensure that all staff have access to courses that enable them to play a part in delivering more Recovery focused services. Personal Recovery and Wellness planning, shared decision making, coaching approaches, solution focused approaches, shared crisis planning, joint safety planning, collaborative care planning …. are all fundamental aspects of practice in Recovery focused services so training needs to be available for all staff to understand and implement these approaches.
Similarly, team leaders and managers need to adopt a strength based, facilitative and supportive style of management to enable all staff to work to their full potential, to build on their strengths and cope with external stressors. Everyone has the right to employment support and reasonable adjustments to their role. Training must be available for managers to learn these skills – not just when working with PSWs, but for the benefit of everyone in their service.
9.5 Non-peer staff with lived experience
As previously referenced, between 30 and 60% of staff working in mental health services have been found to have personal experience of mental health problems. Traditionally, they have been advised not to disclose their own stories.
However, Recovery focused services are all about breaking down barriers between ‘them’ and ‘us’, sharing more about ourselves, demonstrating our shared humanity.
Staff are already beginning to feel more confident about disclosing their own experiences to their colleagues and people who they support; this appears to be even more the case where PSWs are employed.
Although PSWs have received training in how, why, when and how much to share of their own stories, other staff have not. Training departments need to lead the way in ensuring that organisations have clear policies and expectations about whether, how and when all staff can safely, appropriately and effectively disclose aspects of their own life and lived experiences.
10. Supervision for peer support workers
Regular supervision is absolutely essential for all practitioners including peer support workers. The CQC defines supervision as “a safe and confidential environment for staff to reflect on and discuss their work and their personal and professional responses to their work. The focus is on supporting staff in their personal and professional development and in reflecting on their own practice” (CQC 2013)
The challenge for organisations employing PSWs is to consider what supervision means for a profession that is based on personal experiential knowledge and experience rather than a recognised theoretical and professional knowledge base.
Leaders in the field of peer support in the US have defined peer supervision in some detail. Sherry Mead (the author of Intentional Peer Support (IPS) draws on the principles of peer support in describing supervision as a process of co reflection where the supervisor and supervisee help each other to reflect on their practice, where expertise is created together through a process of learning, practicing and reflecting.
She describes this co reflection approach as “referring to reciprocal arrangements in which peers work together for mutual benefit where development feedback is emphasised and self directed learning and evaluation is encouraged” (Mead 2012)
Lori Ashcraft, the originator of peer specialists in Recovery Innovations Arizona, describes peer support supervision as “a strengthsbased process that supports the role of peer specialist. Feedback is important, promotes trust in the relationship, and supports professional development. All supervision must occur within the framework of existing human resource standards and procedures” (Ashcraft, L 2015)
10.1 Why focus on supervision for peer workers?
Peer roles are unique. There is no other occupation in the NHS that requires postholders to share aspects of their personal experiences and it is this that makes supervision both essential and distinct in the following ways:
- Working with people who disclose personal experiences of trauma and mental health challenge is demanding for everyone. For people with their own lived experience it can trigger distress, lead to reliving traumatic events and even lead to vicarious trauma.
- Recalling and referring to personal experience of trauma, mental health problems and Recovery in itself is demanding emotional labour
- Open acknowledgement of personal experience of mental health challenges has the potential to render PSWs vulnerable to discrimination by other staff
- Reference to personal experience is a huge strength and asset in relationships with people using services and can lead to closer connections, greater trust, more disclosure and higher/different expectations from clients.
This brings with it continual questions for each peer about relational boundaries with the individual (e.g. what is the difference between peer support and friendship?) and with the team (what parts of the story I have been told should be shared with the team?); about their own role (I feel more connected to the views of this individual than with other staff … what do I do about this?; I do not feel comfortable with the language used to describe this behaviour…).
Skilful supervision can support PSWs to maintain quality, integrity and safety of peer practice; provide coaching/problem solving to address challenges in practice, develop personal practice and repertoire; enable safe and appropriate sharing of emotional burden of the role; help them to integrate within their workplace, and provide a forum to raise concerns about organisational policies and practice and share decisions about next steps.
10.2 What sort of supervision do PSWs require?
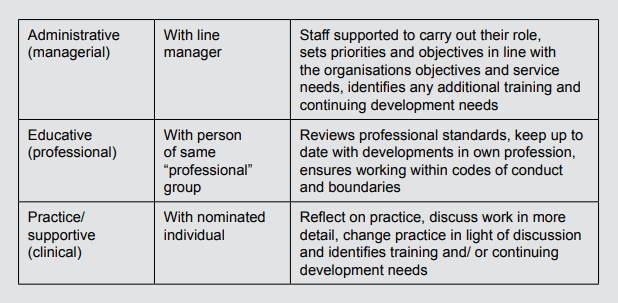
Much of the literature that describes supervision required in the NHS describes three types: managerial, professional and clinical. Within the context of peer working these headings could translate into administrative, educative and practice or supportive supervision. Arguably these headings are better as they describe the “type” of supervision they can expect.
Traditionally supervision models fall into three categories: developmental, integrated and orientation specific. All of these have relevance for the supervision of PSWs, but PSW supervision requires consideration of an additional category which defines whether the supervisor has their own lived experience and expertise in peer support.
Developmental supervision refers to the different stages of a supervisee’s development from “novice to expert”. Each stage consists of discrete characteristics and skills; the key is for the supervisor to accurately identify the supervisee’s current stage, and offer feedback and support appropriate to that level alongside facilitating the supervisee’s progression.
The model uses a process of “scaffolding” to encourage the supervisee to use prior knowledge to produce new learning which fosters the development of critical thinking skills. The Integrated Development Model is by far the most researched development model. For more detail please see Stoltenburg (1981), Stoltenburg & Delworth (1987) and finally Stoltenburg, McNeil & Delworth (1998).
Integrated Supervision relies on more than one theory or technique in much the same way as clinicians describe their practice as eclectic; that is, integrating several theories into consistent practice. One well-recognised model is Bernard’s Discrimination Model originally published 1979.
This model comprises three areas of focus (intervention, conceptualisation and personalisation) and three supervisory roles (teacher, counsellor and consultant). What this means in practice is that the supervisor can respond in one of nine ways. For example, the supervisor can respond as teacher, while focussing on specific intervention; or respond as counsellor whilst focussing on intervention and so on.
Orientation specific supervision model adopts a “brand” of therapy that is selected based on an analysis of the supervisee’s role (for example, CBT informed supervision for a CBT practitioner). Within peer support, Mead’s co-reflection based on principles of mutual support and reciprocity is closest to a brand specific type of supervision for peer support.
Peer to Peer Supervision refers to supervision for PSWs provided by a supervisor with their own lived experience and expertise in peer support. Kopache (1995) describes the difference in impact that supervisors who have lived experience can have in relation to role modelling, support, trust and the building of knowledge based on their experiences. She goes on to emphasise the importance of both planning and developing peer roles and believes they should be embedded in job descriptions and training for supervisors (see HEE thought piece on Peer Development Pathway).
Two commonly used models in peer to peer supervision are Proctor (1991) and Sherry Mead (2005) Proctor’s model describes 3 aspects of the tasks and responsibilities of the supervisor and supervisee. Formative / educative which has a focus on development of knowledge and skills, an opportunity to become increasingly reflective upon practice and is all about learning and growth. Normative / managerial which essentially monitors and evaluates the quality control aspects of supervision.
And finally Restorative/ support which explores elements of psychological support for the supervisee. That is, it explores work life balance, feelings and concerns, it challenges ideas and encourages and enhances good working relationships.
Sherry Mead’s co-reflection guide for supervising in Intentional Peer Support describes the process of creating expertise together through a cycle of learning, reflecting and practising. The model is designed to reflect the principles of peer support and to enhance personal development of PSWs.
10.3 In summary…
Given the role of PSWs, it is essential a) for PSWs to receive regular supervision, and b) for this to be provided by someone with clear understanding of the provenance, role, purpose and potential challenges of peer support, preferably someone who has lived experience themselves.
Beyond this, decisions about supervision will depend on the addressed:
- Who will provide supervision for PSWs?
- How will supervision be provided?
The following tables summarise the advantages and disadvantages of different decisions as suggested by the HEE peer support implementation group which includes employers, trainers and practitioners of PSW as well as user led organisations.
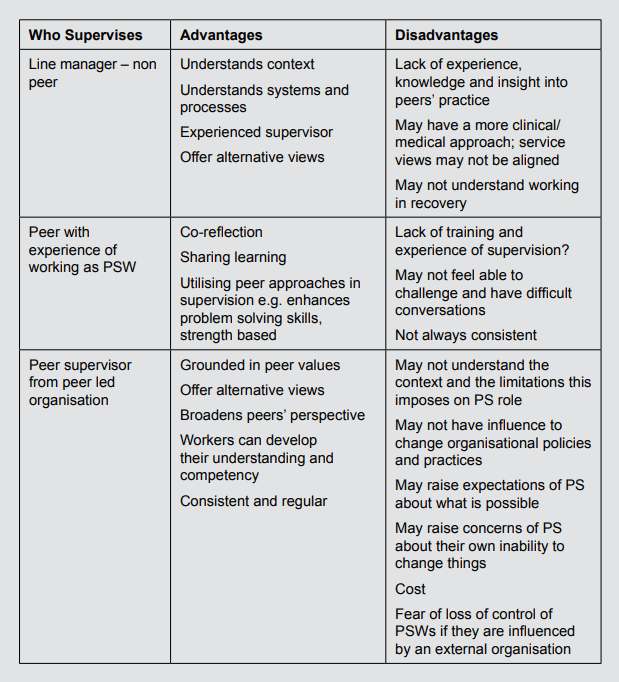
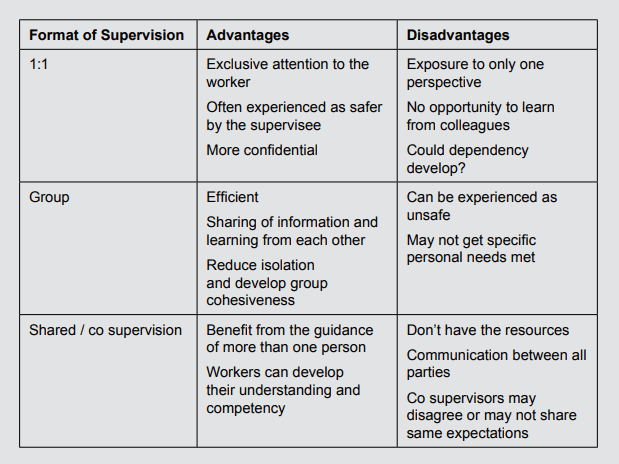
11. Creating a context for PSWs to develop a collective voice
- While individual peer support workers might have an influence on the culture of the team that they work within, this is a huge expectation to place upon them. They have limited positional power and whilst they may have the confidence and skills to influence language, practice and attitudes within a receptive team, this cannot be assumed or expected.
However, if all the PSWs working in an organisation are provided with opportunities to come together at regular intervals, to learn together, generate ideas, solutions and plans, then they have a more powerful collective voice. This forum can also become a space to debate contentious issues, invite external speakers and meet organisational managers and leads to discuss the case for changing particular practices.
- Nottinghamshire Healthcare NHS Foundation Trust has been running PSW Development Days for more than ten years. These run quarterly and membership not only includes all of the peers working within the Trust but is open to PSWs working in local VCSE and user led groups. Issues nominated by the group are placed on the agenda for the following meeting and addressed in detail with expert speakers invited where appropriate.
The group is facilitated by the Trust Peer Development Lead who facilitates open debate and discussion and where agreed, issues will be taken forward to relevant forums to become part of relevant agendas for change (eg PSW role in care planning, note writing, reducing the use of restraint will be taken to relevant decision making groups; PSW led cases to change policies and procedures will be taken to relevant managers).
- In effect, this sort of forum not only amplifies the voice and influence of PSWs within the organisation, increasing their influence on cultural change, it also provides learning opportunities and facilitates personal development of PSWs.
The system wide membership ensures awareness of wider agendas and keeps members of the group informed of relevant events and opportunities for PSWs. Importantly it also provides a space to raise concerns and risks to the integrity of peer support within the organisation.
ImROC’s Vision
For systems, services and cultures to support Recovery and wellbeing for all locally, nationally and internationally.
ImROC’s Mission
ImROC works in partnership with communities to develop systems, services and cultures that support recovery and wellbeing for all. ImROC has been leading the way in recoveryoriented service and practice improvement since 2011.
Originally established on behalf of the Department of Health to champion its ‘Supporting Recovery’ initiative, through a collaboration between the Centre for Mental Health and the NHS Confederation’s Mental Health Network, ImROC is now hosted through Nottinghamshire Healthcare NHS Foundation Trust. This innovative new partnership allows us to cement our close working relationship with frontline providers of care, ensuring that our work remains relevant and useful to practitioners, managers, system leaders, local communities and ultimately, the people who access services.
Our role is about enabling people (who use services, work in services and live in communities) to unlock and pool the strengths and talents they take for granted, explore new ways to make use of them, share knowledge and learning, and facilitate recovery-oriented improvement in the outcomes and experience of health and social care. We rely on and embrace the expertise, experience and collective wisdom of everyone we work with, and encourage communities to develop as a result. Our job is about using our expert knowledge to inspire others to believe that change is possible; pursue their dreams, and most importantly to act: changing attitudes and behaviours. This ethos of working in co-production is at the heart of our organisational work, and role models what we seek to achieve at a practice level too.
1 Slade, M.; McDaid, D., Shepherd, G., Williams, S., Repper, J. (2018) Recovery: The Business Case. ImROC Briefing Paper 14.(imroc.org)
2 NESTA and National Voices (2015) Peer Support: What is it and does it work? London: NESTA and National Voices
3 Thornicroft G. Shunned: Discrimination against People with Mental Illness. Oxford: Oxford University Press 2005.
4 Dixon L, Hackman, A., Lehman,A. Consumers as Staff in Assertive Community Treatment Programs. Administration and Policy in Mental Health and Mental Health Services Research 1997;25:199-208.
5 National Attitudes to Mental Illness Survey (2020) London, Institute of Psychiatry.
6 Krupa, T, Kirsh, B, Cockburn, L, Gewurtz, R. Understanding the stigma of mental illness in employment. Work. 2009;33(4):413–425.
7 Henderson, C, Noblett, J, Parke, Ha. Mental health-related stigma in healthcare and mental health–care settings. Lancet Psychiatry. 2014;1(6):467–482.
8 Schulze, B . Stigma and mental health professionals: a review of the evidence on an intricate relationship. Int Rev Psychiatry. 2007;19(2):137–155.
9 Hansson L., Jormfeldt H., Svedberg P., etal. (2013) Mental health professionals’ attitudes towards people with mental illness: do they differ from attitudes held by people with mental illness? The International Journal of Social Psychiatry 59, 48– 54.
10 Solomon, P. (2004). Peer Support/Peer Provided Services Underlying Processes, Benefits, and Critical Ingredients. Psychiatric Rehabilitation Journal, 27(4), 392–401.
11 Devon Partnership NHS Trust (2009b), Recovery Coordination: Policy Implementation Guide and Practitioners Handbook, Devon Partnership NHS Trust, Exeter.
12 Penney, D and Stastny, P. (2018) Peer specialists in the mental health workforce: A critical reassessment. Mad in America. October 16, 2018.
13 Watson, E. (2019) What is peer support? History, evidence and values. Chapter 2 in Watson,E and Meddings, S. (Eds) Peer Support in Mental Health, London: Red Globe Press.
14 Penney,D. and Prescott, L. (2016) The co-optation of survivor knowledge: the danger of substituted values and voice. In J Russo and A Sweeney (Eds) Searching for a rose garden: challenging Psychiatry, fostering mad studies (p.35-45) PCCS Books.
15 Solomon, P. (2004). Peer Support/Peer Provided Services Underlying Processes, Benefits, and Critical Ingredients. Psychiatric Rehabilitation Journal, 27(4), 392–401.
16 Faulkner,A. and Kalathil, J. (2012) The freedom to be, The chance to dream. Preserving user-led peer support. London: Together
17 Many reports describe the net gain of working in collaboration with people who use services, PSWs, family members and community groups. A good example of innovative partnerships with people who use services Slay, J. and Robinson, B. (2013) In this together: Building knowledge about co-production. London: New Economics Foundation.
18 Slade et al (2018) The business case for recovery. Nottinghamshire Foundation Healthcare Trust: ImROC Briefing paper 14.
19 Chamberlain,Mead
20
21 Morgan,P. and Lawson, J. (2015). Developing guidelines for sharing lived experience of staff in health and social care, Mental Health and Social Inclusion, Vol. 19 Iss 2 pp. 78 – 86 A survey was undertaken in the Mental Health Directorate of DHC, with a response rate of 31 per cent; 53 per cent of staff self-identified as having lived experience of mental health problems. A similar survey in Devon Partnership Trust had similar results. Of a 23 per cent response rate, 43 per cent identified as having lived experience of mental health problems. One third of respondents with lived experience felt unable to be open with their managers and colleagues with the most frequent reason being fear of stigma, misunderstanding and rejection
22 Davidson
23 Repper, J & Perkins, R (2013) The Team Recovery Implementation Plan: a framework for creating recovery-focused services. ImROC.
24 Repper, J & Perkins, R (2013) The Team Recovery Implementation Plan: a framework for creating recovery-focused services. ImROC.
How can ImROC help?
ImROC has previously commented on the media exposure of appalling practice in inpatient units (Response to Dispatches – ImROC – Implementing Recovery through Organisational Change); coverage that vindicated the personal reports and cries for help from people in those services, patients, their families and staff. The Independent Inquiry into events at Edenfield that were exposed by Panoram in February 2023 digs deeper and finds little to reassure any of us that we can feel confident that if we reach a point of crisis we can look forward to a safe, therapeutic or compassionate response. Whilst the report focuses specifically on one Trust, the experiences that we hear daily from ImROC’s staff and students who have themselves spent time in inpatient settings closely and alarmingly echo the findings.
What is clear is the extent to which staff members who are committed to developing respectful and empowering relationships, creating safe spaces for those in distress to make sense of their experiences and find ways forward in a supportive and understanding environment have little opportunity to do so. More worrying is their powerlessness in making their concerns heard, their inability to positively influence culture and practice when there is systemic resistance to hearing ‘bad news’ and responding appropriately.
Even worse is the finding that people from black and minority ethnic groups and those with protected characteristics (both patients and staff) appear to fare worst; not merely in not being heard but in being treated coercively and disrespectfully with no understanding of their experience, their culture or what drives their behaviour.
It is somewhat reassuring to see NHSE commitment to shifting the culture of practice in inpatient settings through significant investment in values based, lived experience led training, coaching, leadership development, supervision and quality improvement. (Culture of Care Programme (rcpsych.ac.uk). But this will inevitably be slow to implement, time limited and cannot possibly address the widespread systemic problems relating to lack of funding, workforce shortages, inadequate social care and support and worsening inequalities in all domains of life. Indeed no single intervention or approach will provide all the answers.
So what can ImROC offer that might support current endeavours to improve the experience of people in crisis?
1. A briefing paper
We have coproduced our own response to inform the recovery of acute inpatient care. This carefully cocreated paper builds on the experience of people who have a range of different experiences in acute care – people who have spent time in wards and family members, people from different minority and ethnic groups, people with different professional roles. The result is lengthy but that is because it is not a set of directions, guidelines and checklists. It goes back to basics and focuses on the importance of human connections: the relationships that underpin safe and supportive care. It discusses ways of offering trauma informed and neuro-inclusive environments and conversations; and emphasises the need for appreciative and collaborative decision making whether developing collaborative care plans, joint safety plans or preparing to move on.
This paper is available to view here (24. Recovering Adult Acute Psychiatric Inpatient Wards – ImROC – Implementing Recovery through Organisational Change) and we will be running a webinar to offer a visual/verbal and accessible summary of the paper. This will be followed by a series of lived experience led podcasts that focus on different elements of the paper. Follow us on Linked in to find out when these will be happening
2. Companion Guides
Alongside this briefing paper, we have coproduced two companion guides . The first (Thinking about Recovery Together – ImROC – Implementing Recovery through Organisational Change) is a conversational tool loosely based on a personal recovery plan – adapted for use in acute care settings. We heard from people who have been in acute wards that it can be hard to focus on completing a full recovery plan in times of acute distress. There are so many immediate fears, worries and priorities. However, some people, staff and patients find it helpful to have a structure to work with, some key questions to focus on, questions that validate a persons strengths, resources, experience and emphasise possibility, hope and aspirations.
The second is a benchmarking tool: Team Recovery Implementation Plan for Acute Inpatient Wards
Designed for whole teams, including those using their support and family members, to use to assess their strengths and achievements, the gaps and potential areas that need improvement against evidence based good practice benchmarks. This is specifically adapted for inpatient settings and provides a tried and tested basis for self assessment, priority setting and quality improvement. ImROC has long experience of working with teams utilising this tool to identify bespoke goals, supporting action planning and implementation.
3. Co-facilitated learning spaces for inpatient staff
We offer co-facilitated learning spaces for inpatient staff which are developed with organisations/teams to meet their particular needs. These take the form of action learning sets for key members of staff to learn, reflect and share in a safe group away from their place of work.
4. Culture of Care
We have already written a paper that focuses on the culture of care (19. Creating a Recovery Focused Culture: changing the nature of conversations from the bottom up – ImROC – Implementing Recovery through Organisational Change). As always we start with people using services and the staff who work with them. Both groups are frequently disempowered with minimal influence, receiving little appreciation and little support. This paper offers examples, ideas and approaches to change the nature of conversations at every level of organisations.
5. Coproduced recovery focused learning spaces
It is interesting to see that the Independent Inquiry found that the Recovery Academy was a beacon of light for those using the Edenfield Unit. ImROC developed the first Recovery College in England in 2009 and has supported their development ever since. All research demonstrates the benefit of coproduced recovery focused learning spaces where people learn alongside others who share their experiences and their stories of hope and achievement. ImROC continues to offer support for any service wishing to develop their Recovery College offer into inpatient areas, this can be offered to individual teams or services, or through membership of our Learning Set. International Recovery College Learning Set – ImROC – Implementing Recovery through Organisational Change
6. Peer Support Workers
There is no mention of peer support workers in the Edenfield inquiry, yet research demonstrates that the employment of peer workers in acute care correlates with an improvement in staff attitudes and a reduction in the use of restraint and coercion. We believe that peer support is an essential and complementary role in any multidisciplinary care team. Research suggests that peer workers offer hope, validation, time, practical and emotional support that is not bound up with treatment and regulation. In addition peer support workers can offer advocacy and bring alternative perspectives in team practices and decisions. Whilst imROC offers a whole pathway of accredited training and development for peer support workers ( Training Courses – ImROC – Implementing Recovery through Organisational Change) , we do not recommend their employment in teams without careful training and preparation of the team. We offer workshops with mental health teams to prepare them for peer support workers (Team Recovery Implementation Plan for Acute Inpatient Wards – ImROC – Implementing Recovery through Organisational Change) and these are a helpful way of identifying strengths and challenges existing in the team.
Get in touch
If you are interested in finding out how we could support you, your team or your organisation to improve the experience of inpatient care, please do get in touch. We always start where you are at, working with you to provide coproduced and cofacilitated support to meet your needs.
Across UK mental health services, most NHS Trusts and voluntary sector services are actively recruiting people with personal experience of mental health challenges to newly created ‘Peer Support Worker’ positions. A national competency framework for peer workers has been agreed (Health Education England, 2020) and accompanying training programmes have been established (see for example, Bradstreet, 2006; Repper et al, 2013 a & b). The value that such employees can bring has been widely documented (see, for example, Repper et al 2013a, Davidson et al, 2012; Watson and Meddings, 2019). The benefits for people supported by peer workers can include increased self-esteem, confidence, problem-solving skills, hope, positive feelings about the future and a sense of empowerment. Peer workers have also been found to bring benefits to the teams and services in which they work by providing inspiration, challenging negative attitudes and facilitating a better understanding of the challenges people using the service face. There are also benefits for the Peer Support Workers themselves including increased confidence and self-esteem, a positive sense of identity and value, feeling less stigmatised and empowered in their own recovery journey.
20. The Value and Use of Personal Experience in Mental Health Practice
Rachel Perkins and Julie Repper
The advent of Peer Support Workers who explicitly draw on and share their personal experience of mental health challenges in their work has highlighted two key issues.
1. Peer Support Workers are not the only employees with experience of mental health challenges.
There are many nurses, doctors, psychologists, occupational therapists, social workers and other mental health professionals who have themselves experienced mental health challenges. Indeed, workforce surveys of staff in three mental health Trusts have revealed that up to 62% of staff have experience of mental health challenges and/or of caring for someone in the family with mental health conditions (Morgan and Lawson, 2015). Are these people also ‘Peer Workers’?
We would argue that, while their personal experience of mental health challenges can undoubtedly enhance the work of trained mental health professionals, they are primarily employed for their expertise in their chosen profession and in this professional role, their primary source of reference is their professional knowledge. Peer support workers bring a different kind of expertise: experiential knowledge drawn from their personal experience of recovery with mental health challenges. They also offer a different kind of relationship: one based on mutuality (by definition, as peers they share experiences), reciprocity (learning together rather than one being the expert and the other being recipient of that expertise) and cocreation (with the person they are supporting) of understandings, ideas and ways forward. Peer workers are not employed to deliver in any type of intervention or therapies; they work outside traditional power hierarchies and claims to special, professional, knowledge.
This peer to peer relationship is quite different to the relationship between a mental health professional who also has personal experience of mental health challenges: Such a professional is very much part of traditional hierarchies and has claims to the special knowledge of their professional training. This does not mean that professionals should not use their personal experience of mental health challenges in their work, rather that these do not make them a ‘Peer Worker’. Indeed, if we only employ people with personal experience of mental health challenges in designated ‘peer’ roles, we risk reinforcing the destructive ‘them’ and ‘us’ barriers that remain within mental health services.
Breaking down barriers, reducing ‘othering’, improving staff expectations of people using services and challenging stigma and discrimination more generally, can only be achieved if personal experience of mental health challenges among all mental health professionals is valued at organisational, team and interpersonal levels. Peer Support Worker roles are important, but it is also critical that people with personal experience of mental health challenges can a) access training for all of the roles within mental health services, b) are explicitly welcomed to apply for these roles in organisations, c) are supported to use these experiences appropriately, effectively and safely in their practice, d) receive the employment support that they require to work to their full potential.
2. Lived experience of mental health challenges is not the only sort of personal experience that may be relevant and useful in work within mental health services.
People working in mental health services may bring personal experience of many life challenges in common with the adversities faced by people using services: bereavement, physical health challenges and impairments (themselves or in someone close to them), relationship difficulties, loneliness, redundancy, being a refugee, racism, sexism, heterosexism and other types of discrimination and disadvantage. We know that mental health challenges do not occur in a vacuum, they occur in the context of a family, a relationship, a community, a culture and a place … All of these are important in understanding the meaning of mental health challenges for someone using services and the possibilities and opportunities that are available to them. Again, mental health workers may have personal experiences in common with the person/people who they support. These experiences may be a cause or consequence of mental health challenges, or they may seem to be unrelated. It is the fact that professionals working in services and people using services have experiences in common that is key to building different kinds of relationships that draw on shared human experience and insights rather than relying purely on particular professional skills and strictly professional roles, that is the key here.
Recovery is about rebuilding a life – discovering and pursuing the things you value, your interests and possibilities. The experience that staff have of different activities, interests and possibilities may be equally important in assisting people in rebuilding their lives as their professional skills. We need to extend our vision of ‘lived experience’ beyond that of mental health challenges to encompass the full range of personal experience that may be valuable and useful in mental health work. Every professional brings to their work, not only their professional expertise, but also their:
- Personal life experiences.
- Interests, hobbies, skills, likes, dislikes and activities outside work.
- Culture, community knowledge and contacts.
- Past struggles, difficulties and disappointments in life. Some may also bring their experience of the mental health challenges of their relatives friends and people who are close to them, and, of course, their own experience of mental distress.
Why share personal experience?
“Contrary to previous research on patients’ experiences, the themes that predominated related to the emotional not physical environment in which they stayed … relationships form the core of service users’ experiences of psychiatric hospital admission …” (Gilburt, et al, 2008)
Relationships are central to the experience of mental health services and central to recovery. Many people with mental health challenges feel cut off from families, friends and communities.
“Social relationships and social integration are as (if not more) important as smoking, drinking, exercise and obesity in determining health and wellbeing.” (Holt-Lunstad et al 2010)
One of the key aims of services must be to assist people to rekindle those ordinary relationships on which all of us rely. However, relationships with mental health professionals can be particularly powerful … for good or ill. If the mental health professionals who provide your treatment and support do not seem to respect you, trust you, believe what you say, believe in your possibilities, how can you hold on to hope and believe in yourself and your own possibilities? We know that trusting, empowering and hope-inspiring relationships are central to recovery and recovery-focussed services:
“Meaningful relationships, peers, and role models increased participants’ motivation to change especially when shared experiences facilitate identification with these significant others” (Price-Robertson et al, 2016)
Yet in relationships between mental health professionals and the people they support there are many barriers:
• One person talks about their thoughts and feelings, the other does not
• One is in the role of helper and the other is in the role of being helped
• One is there because they need help (or someone else thinks they need help) the other is paid to be there • Differences of culture, ethnicity, age, gender, class, faith …
• One person is ‘the expert’ who defines what is wrong and prescribes what they should do (and, at the bottom line, can force them to accept their views) … and if the person using services does not agree with the ‘expert’ then they may be defined as ‘lacking insight’ or ‘non compliant’ and their perspective discounted.
These are all barriers that divide ‘them’ from ‘us’ and they are maintained by, often unwritten, traditional rules that govern relationships within mental health services: the ‘expert’ knows best, and ‘experts’ must give nothing of themselves, maintain ‘professional boundaries’. It may be beyond the power of any individual professional to dismantle traditional heirarchies and power relationships. However, if we are really to respect and promote the recovery of people using services then we must reach across that divide between ‘them’ (the people using ‘our’ services) and ‘us’ (those of us who are employed to ‘fix’ them); erode the barriers that exist within services – and the communities they provide for. First we must recognise the expertise of lived experience as well as professional expertise and bring these together in a process of ‘co-production’ (see Lewis et al, 2017) where equal value is placed on experiential knowledge as upon specialist professional knowledge. Second, we must foster relationships that recognise and demonstrate our shared humanity. As Wyder et al (2013) found “those who felt they were treated as somebody who could be counted on, as a fellow human being … felt respected and the experience allowed them to gain self-confidence.”
Barriers and risks
In some services there exist physical barriers between people using services and those working in them (separate cups, separate toilets, signs declaring that staff do not tolerate aggression or violence) but boundaries also exist in relationships between professionals and people using services – and in how we have defined what ‘being professional’ means. Too often this includes the routinisation of ‘non-disclosure’. The sharing of personal experience by mental health professionals has often been perceived as violating professional boundaries and codes of conduct (Lovell et al, 2020; Dunlop et al, 2021). Organisational cultures typically discourage ‘disclosure’ on the part of professionals and professionals feel that doing so might result in disciplinary action (Lovell et al, 2020; Dunlop et al, 2021). Whilst such beliefs may be widespread, as Lovell et all (2020) and Dunlop et al (2021) point out, across the main codes of practice, standards and ethics for professionals, the sharing of personal experience is not forbidden. Indeed, there is much to be lost if mental health practitioners do not use and share their personal experience in their work
“self-disclosure can help foster a trusting relationship between service user and practitioner through similarity, credibility and shared understanding.” (Dunlop et al, 2021)
Traditionally, the sharing of personal experience has been referred to as ‘disclosure’ or ‘selfdisclosure’. We prefer not to use this term because it has negative connotations of ‘disclosing some shameful secret’. We prefer the term ‘sharing personal experience’ to indicate the positive value of such experience. Just as there are risks associated with the inappropriate use of professional expertise (e.g. based on our professional judgements we might encourage people to ‘be realistic’ about their limitations, thereby eroding their hope and life chances – ‘You will never be able to cope with the stress of a job’) there are also risks associated with the inappropriate use of personal experience. The sharing of personal experience may be considered inappropriate if, for example, it:
• Removes the focus from the person being supported to the person employed to provide support.
• Burdens the person being supported with too much information leaving them worrying about the professional and the difficulties they are facing.
• Makes the person reluctant to ask for help because the professional already has so many problems of their own with which to deal.
• Creates a competitive situation between the professional and the person about whose challenges are greatest (e.g. ‘Don’t worry about taking that medication – I have taken far more than that for years.”)
• Creates confusion about the nature of the relationship (moving beyond a work relationship to friendship or even intimacy).
• Becomes prescriptive if the professional implies that the way they dealt with difficulties is the ‘correct’ or only way (‘ I know what you mean, you should do what I did …’).
• Invokes envy in the person being supported (if they see the professional coping far better with similar problems than they are).
• Creates difficulties for the mental health practitioner when they share experiences they are not ready to share or opens up subjects they are not comfortable discussing leaving them feeling exposed and vulnerable.
• Provides personal details that might cause confusion about the nature of our relationship or potentially put us or our family members at risk, for example our home address or details of the school our children attend. (see, for example, Henretty and Levitt, 2010; Audet and Everall, 2010; Ruddle and Dilks, 2015; Dunlop et al, 2021).
The value of sharing personal experience with people using the service
In many walks of life, sharing personal experience is an important feature of trusting and respectful relationships. Within mental health services, sharing personal experience helps us to reach across the ‘them’ and ‘us’ divide and foster those human to human relationships that can be critical in helping the person to feel valued and more than ‘just a patient’. Trust is a twoway street: if mental health professionals expect people using services to trust them with the intimate details of their lives, they must give something of themselves as well. It is noteworthy that the one of the core interventions developed by the widespread ‘Safe Wards’ initiative (which resulted in 15% decrease in the rate of conflict and a 24% decrease in the rate of containment) was the ‘know each other’ exercise1 . This involved staff providing some information about themselves to residents on the ward – their likes, dislikes, hobbies, interests, favourite TV programme, film, book, music etc. – and encouraging people using the service to provide similar information, thus fostering interactions based on shared humanity and similarity – beyond their previously fixed identities as ‘nurse’ and ‘patient’.
The sharing of personal experience can: • Foster authentic, human to human interaction. • Promote an alliance and build trust. • Normalise experience: enabling people to feel less alone and that much of what they are experiencing (like hopelessness, despair and anger) are common reactions to what has happened (see Deegan, 1988). • Build self-esteem. • Challenge myths and misconceptions. • Facilitate self-exploration and encourage people to talk more openly about their challenges. • Show similarities that can provide reassurance and alternative ways of understanding experiences and approaching challenges. (See, for example, Henretty and Levitt, 2010; Audet and Everall, 2010; Dorset Mental Health Forum, 2013; Morgan and Lawson, 2015; Ruddle and Dilks, 2015; Meddings, Morgan and Roberts, 2019; Lovell et al, 2020; Dunlop et al 2021).
The value of sharing personal experience within the team or service
The sharing of personal experience can also be a valuable resource for the team/service in which staff work. The benefits include:
• Providing access to a greater range of talents that may be of use to people using the teams’ services. This might include, for example, language competencies, music and sport. The interests and skills of staff can be used to provide pointers to helping clients to access different activities and community opportunities.
• Providing the team with greater range of expertise. This might include the experience of different kinds of challenges and knowledge of different cultures and communities. For example, an understanding of how mental health challenges are construed in different cultures and communities can provide insight into the experience of people using the service: the challenges and possibilities facing people from different cultures and communities and greater understanding of their feelings and behaviour.
• Making the team a more supportive place to work. If team members feel that they can talk about the challenges they are facing then this can help colleagues to feel more supported and enhance staff well-being.
“Within the team I have referenced some of my difficulties. It is an open environment from that point of view … I do think that one being open can bring more openness in others. It almost gives ‘permission’ for people to feel they have the opportunity to be open about difficulties they face.” (cited in Perkins, 2021)
• Contributing to the breaking down barriers and reducing ‘othering’. If everyone feels able to talk about the challenges they are facing then this can lead to a recognition that “…everyone has their own experience of recovery as a consequence of the wideranging vicissitudes of life that leave noone unscathed.” (Perkins, 2021)
If staff are encouraged to see their personal experiences as assets and resources in their practice, and the whole team values the range of different experiences that members bring, then it is far more likely that staff will be more open about themselves. What they previously felt compelled to hide – as vulnerabilities or weaknesses – can more confidently be shared. In a staff survey undertaken in Devon Partnership Trust, 43% of respondents identified as having lived experience of mental health problems, but one third of respondents with lived experience felt unable to be open with their managers and colleagues. The most frequent reason for not disclosing their mental health problems was fear of stigma, misunderstanding and rejection (cited in Morgan and Lawson, 2015). If people feel unable to share these experiences, they are also unable to discuss the sort of supports and adjustments that might enable them to stay well and work to their full potential.
There can be no absolute rules about using personal experience at work – we cannot replace the traditional ‘tell nothing of yourself’ with ‘tell everything’. Ultimately, we must be guided by the purpose of our relationship with people using services: to help them in their journey of recovery. Individuals and situations differ so all professionals need to make informed judgements about what we can usefully share, why, when, with whom, how and how much. It is noteworthy that Henretty and Levitt (2010) found that 90% of mental health professionals had shared personal experiences with people using services, yet this is rarely explored in supervision and clinical discussions, there are few guidelines about such matters about and professional guidelines have typically been silent on such issues. As Ruddle and Dilks (2015) say, “Everyone is doing it but no-one is talking about it. It is time we started.”
Starting to talk about sharing personal experience
The ‘Competence Framework for Mental Health Peer Support Workers’ (Health Education England, 2020) states that a core role of Peer Support Workers is to draw on and share their lived experience of mental health challenges and other life experiences in a way that is relevant to the person and their circumstances, helps them to know that they are not alone, empowers them and gives them hope and helps them to discover the recovery and self-care practices that work for them while maintaining appropriate boundaries. The training of Peer Support Workers explicitly addresses how they might do this and considers the risks as well as the benefits of sharing personal experience. However, the training of other mental health practitioners does not give such detailed consideration about using their personal experience to enhance their professional roles. Some guidelines have begun to emerge for those mental health professionals who have personal experience of mental health challenges that they are willing to share. For example, Meddings, Morgan and Roberts (2019) suggest that mental health professionals think about what facets of their personal experience of mental health challenges they are comfortable about sharing, when to share it and why – the reasons for sharing – and how to share it. They recommend that practitioners think about two key dimensions ‘Does it benefit the person you are sharing with?’ and ‘Is it okay with you?’. Scior (2017) developed ‘Honest, Open and Proud for Mental Health Professionals’ – a self-help intervention that supports mental health professionals with lived experience of mental health challenges to make decisions about ‘disclosure’. This helps practitioners to consider the pros and cons of sharing, contexts and levels of sharing and how to share their experiences in a meaningful and safe way.
More recently, guidelines for the sharing broader aspects of personal experience have begun to emerge. For example, Dorset Healthcare University NHS Foundation Trust (Morgan and Lawson, 2015) have developed guidelines for staff sharing their lived experience that moves beyond personal experience of mental health challenges to personal experience of overcoming health challenges and challenging life circumstances. This makes it clear that personal experience of challenges and adversity is an asset in mental health practice, and provides guidance to all mental health practitioners. The guidance takes the form of a set of principles that staff should consider and describes the benefits of sharing as being: to inspire hope, improve partnerships with people who use services and their families, reduce stigma and promote staff well-being by creating a culture of openness within teams. Based on work by Dunlop et al (2021), Leeds and York Partnership NHS Foundation Trust have developed a ‘Sharing Lived Experience Framework’. This takes a yet broader perspective on the sharing of personal experiences to include such things as hobbies, interests, sexuality, religion and culture. The Framework spans what it describes as ‘the disclosure process’
“… from pre-disclosure planning and reflection, to in-the-moment questions to consider internally and dialogically with the service user, and finally to post-disclosure reflection. Such reflection should consider the impact of disclosure on the service user, the practitioner and the relationship, and how the experience should inform future disclosure decisions.” (Dunlop et al, 2021)
The framework takes the form of a series of questions for guided self-reflection, clinical supervision and training. It also explicitly includes questions relating to the professionals ‘motivation for sharing’: ‘healthy motivations’ (such as normalising/ demystifying, offering hope and/or ideas for coping, being seen as human and strengthening the relationship) and ‘warning signs’ when “the motivation for disclosure is unhealthy”. This guidance focuses on sharing personal experience with individuals using the service – it does not consider the benefits of sharing personal information within the team/service. Building on the work of Morgan and Lawson (2015) and Dunlop et al (2021), an IPS Grow working group developed guidelines on using personal experience within ‘Individual Placement and Support’ evidence based supported employment programmes (Perkins, 2021). This included the value of sharing the full range of personal experience both in individual work and within teams and services.
The purpose of this ImROC briefing paper is to build on all of this existing work. It considers the use of all relevant personal experience and how this might appropriately and safely be used in individual work, and in increasing the expertise available to the team, to promote the recovery of people using services. We also explore how organisations might create a culture that both values the personal experience of all its employees and encourages them to use it in their work.
Guidelines for professionals in sharing personal experience
Following Dunlop et al (2021) and Perkins (2021), this might include 3 elements:
• Preparation: what life experience you bring that may be useful and what you feel able to share and with whom
• Making decisions in individual or team interactions: how, how much, what, why, when and with whom (a colleague, the team, a person you are supporting).
• Reflecting on the use of personal experience: lessons learned – what was effective, what was less useful
Preparation
Every practitioner needs to think, in advance, about what personal experience we feel able to share with people using the service, with their manager, with colleagues and other team members. This is important because:
• When we have shared something with someone we cannot ‘unsay’ it.
• Once you have shared an experience with one person, we need to be prepared for them to share this with others. We cannot ask or expect anyone to keep it to themselves, this creates confusion about the nature of our relationship.
• We need to be able to explain the reasons why we have shared any aspect of our personal experience if asked.
• We need to consider the possibility that sharing one aspect of our experience might lead to further questions, we must prepare ourselves by thinking about how we might answer these or how we can close these down in a supportive manner.
• Our mood and day to day stresses can influence our responses, if we prepare in advance we are more likely to respond in a mindful manner.
We may be prepared to share different things with different people and for different purposes. For example, if we are having difficulties at home we may share these with our supervisor or manager in order to gain support or adjustments in our work. This may well be something that is far too raw to share with colleagues or people we support and is very different from sharing personal experiences to help people we support or colleagues in their work.
It is reasonable to expect all mental health practitioners to bring something of their experience of life to benefit colleagues and people they are supporting but each of us needs to make decisions first, about what we feel able to share and second about how we present it. This will influence the way in which it is heard and the impact it has on ourselves and the people we share it with. For example, many people will have experienced the breakdown of a relationship, and this may be useful in understanding the experience of people we are supporting colleagues who face similar challenges and supporting them. However, we need to think about how much detail we present and how we frame it. Without prior planning and consideration, it is too easy to find ourselves sharing all the ‘gory details’. This risks leaving us feeling very exposed and embarrassed and burdening others with an excess of information. While we may need to acknowledge the gravity of what happened for us, if we present our experience without any information about how we tried to cope and move forward then we risk making others feel hopeless and negatively influence the way in which they perceive us: we are ‘vulnerable’, unable to cope, untrustworthy.
See Table 1 for questions that you might want to reflect on in deciding in advance what personal experience you may use in your work.
Table 1. Preparation: Some questions for reflection
• What personal experiences have I got that might be helpful in my work? For example: life history and family background; hobbies, skills, interests; culture; faith and spirituality; difficulties we have experienced in the past.
• Which of these am I comfortable about sharing: with colleagues to inform their work? with people I support to help them in their recovery? (n.b. if you share this with one person others are likely to find out. Are you comfortable for this information to be available more widely?)
• How might sharing this information be helpful to: colleagues to inform their work? people I support to help them in their recovery? (n.b. think about how you might explain sharing this information to a sceptical colleague or manager)
• How am I going to present this experience and how much detail am I willing to share: with colleagues to inform their work? with people I support to help them in their recovery? (n.b. how you present it will influence the impact it has on you and the people we share it with)
• What experiences and which details am I NOT prepared to share?
• What information do I put on social media? (n.b. this public information and potentially available to colleagues and people we are supporting)
Making decisions in individual interactions
In everyday life, when we meet people we show an interest in them, and give something of ourselves. This may be something as basic as saying ‘I love the colour of your jumper – green is my favourite colour’. Such interactions help develop our relationship with the person and are equally important in forming relationships with people we support or our colleagues: developing a rapport with the person, showing an interest in them, going beyond the strict requirements of gaining/giving information that enables us to fulfil our professional role. Indeed, the personto-person interaction that we have is an important foundation of the mutual trust that will be critical to the effectiveness of any professional intervention. Sharing personal information or experiences sets the groundwork for the relationship that we will have with colleagues or people we support. What it is useful to share, when and how has to be considered in the context of every individual interaction.
There will be individual differences. While there may be some colleagues and people we support who value practitioners sharing something of themselves and their experiences, others will prefer to keep this to a minimum. We need to be sensitive to this and it is probably sensible to start small, and in relatively non-threatening areas (e.g. ‘Were you OK getting here in the dark – I hate these short winter days) and see how the person responds.
Moving beyond relationship building, we need to give more attention to the experiences we share to support people with specific aspects of their own recovery. We need to think about what we select to share, how much detail will be helpful, and why we are sharing this experience: the possible benefits and risks attached, and warning signs that we may be tempted to share too much (see Table 2).
We also need to think about getting the timing right in terms of my relationship with the person, are they in the right place to hear this today, do I feel comfortable discussing it right now, is there space and time to cope with any possible conversation that might ensue – will we have to leave issues hanging?
Finally, it is generally wise to avoid saying ‘I know what you mean’. No two experiences are the same – individuals and circumstances differ. No-one can ever fully understand the impact of an event on another person. It is usually preferable to use a form of words like ‘I don’t know what it was like for you, but when X happened to me I felt ….”. Nor should we assume that our way of dealing with things is the only way or the right way, merely one in a range of options: ‘I did X but I know of other people who found Y or Z helpful.’
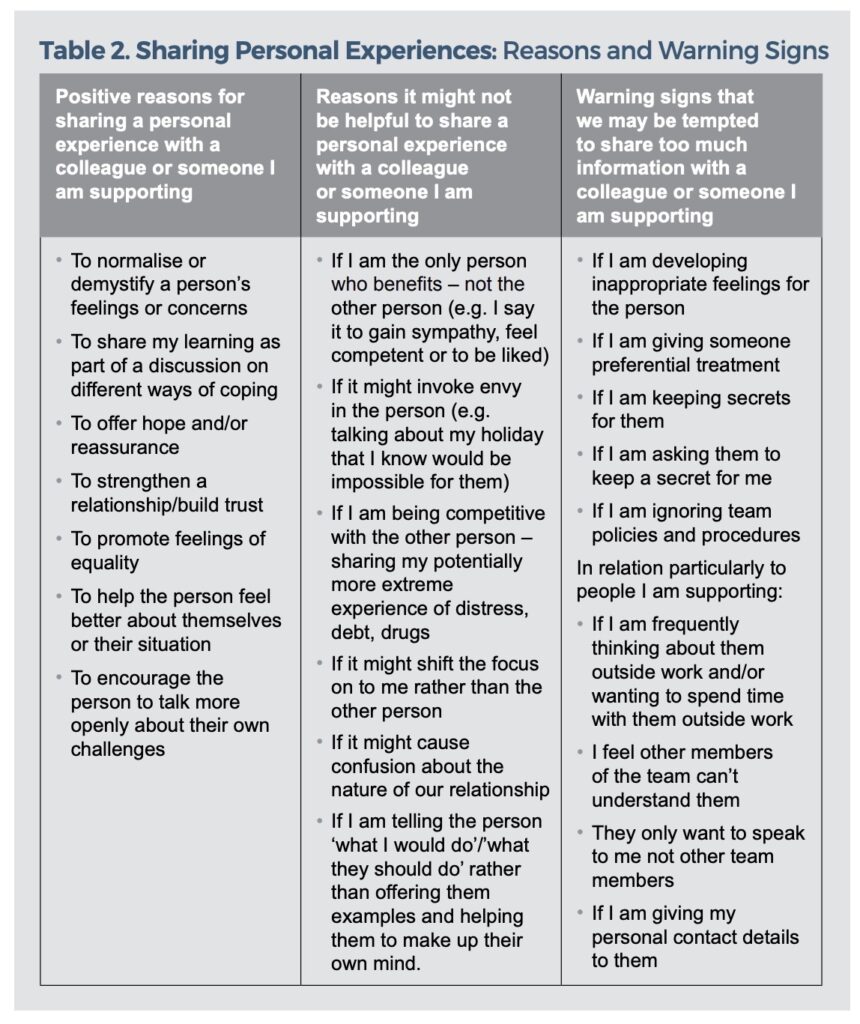
Reflections after sharing personal experience
Just as it is wise to reflect on professional judgements and interventions, it is important to reflect on our experience of sharing of personal experience. Whether such experience has been shared with colleagues or someone we support, reflection allows us to learn from or experience and can inform future decisions about sharing. Table 3 provides some questions that might assist such reflection. While personal reflection may be important, it can also be useful to use supervision or discussions with colleagues for this purpose.
Table 3. Learning from our experience of sharing: some questions for reflection
• How did my experience of sharing personal experience go – what impact did it have on The person with whom I shared? Our relationship? Me?
• How did it help someone I support in their recovery or a colleague in their work? What worked? What didn’t work? Why?
• How did sharing my personal experience feel at the time and how do I feel now?
• What did I learn from my experience of sharing?
• Do I want to, and would it be useful for me to, share my learning with the team?
Creating a culture in which personal experience is valued and used
If mental health practitioners are to bring both their professional expertise and their personal experience to their work then we need to create a culture – values, beliefs and behaviours – that explicitly and implicitly respects both of these. Leadership is critical in creating a culture where personal experience is valued and used alongside professional expertise. Leaders, at all levels of the organisation, need to commit to making this happen.
Directors, managers and team leaders all need to:
• Ensure that personal experience of all staff is explicitly valued in all documentation, policies, procedures and operational policies.
• Personally model the appropriate sharing of personal experience. This implicitly ‘gives permission’ for other members of staff to do likewise.
• Create expectations that every member of staff will use some of their personal experience in their work. This might usefully include a requirement that all staff prepare a brief biography of themselves which includes their professional experience, something about their interests and activities outside work and their reasons for working in this area. Together with photographs, these might then be shared on ‘meet the directors and managers’ pages of a web-site and a ‘meet the team’ information leaflets and noticeboards.
• Explicitly values personal experience within the recruitment process.
– Job descriptions and person specifications should indicate that personal experience of life challenges, including mental health conditions, is a desirable asset and that it is essential that the post-holder is willing to use some relevant personal experience in their role (e.g. life experience, interests and activities outside work, cultural and community knowledge, as well as difficulties and disappointments in life).
– Information provided to potential applications indicates that personal experience is valued alongside professional expertise and experience.
• Clinical/Practice Supervision models, values, explores and develops use of personal experience in practice.
– The supervisory relationship should be one in which both supervisor and supervisee share personal experience and foster mutual learning. It is important that supervisors initiate this process in order to model how the supervisee might do likewise.
– Supervisors can help supervisees to explore what personal experience they bring to their work, whether they feel able to use this experience in their work and how they might do so (see Table 1). This might include developing their own biography to be included in team materials.
– The process of supervision should be used to reflect on, and learn from, the sharing of personal experience, making it clear that none of us get it right first time and all of us are learning. It is vital that the supervisor gives examples of this from their own experience.
– In interviews candidates are asked to reflect on some aspect of their personal life experience and how this might enhance their practice.
– Supervision provides a context to reflect on relevant policies and procedures that relate to ‘boundaries’ in relationships (e.g. giving and receiving of gifts and ‘professional/patient’ relationships).
• Ensure that all employees have the opportunity to work to their full potential. A culture that values personal experience must also be one that BOTH enables people to talk about difficulties they are facing and supports them through these as far as is possible AND supports them to draw on the full range of personal experiences in their work. This might usefully include:
– Enabling each employee to use some of their personal experience and expertise as part of their work (e.g. someone who is keen on football organising a football team or helping anyone who wants to access local football opportunities). Work is more satisfying if you are able to do things that you like and are good at.
– Recognising that people have a lot going on in their lives and that if accommodations can be made in the work environment then well-being and performance are improved. This should include not only the ‘reasonable adjustments’ for disabled people required by the Equality Act, but also adjustments for people who may have child-care responsibilities, an appointment with a debt advisor or run/attend a yoga class.
In addition, team leaders might consider the use of ‘Team Recovery Implemetation Plans’ (Repper and Perkins, 2013). These encourage front line staff, people using services and those who are important them, to identify the full range of talents that exist within the team and share intelligence about community opportunities in order to develop plans to enhance recovery-focused practice within the team.
Training and development also have a key role to play in developing skills and understanding to enable staff to use their personal experiences safety, appropriately and effectively in their practice.
• All professional training courses should help trainees to think about what personal experience they bring, why this might be useful and what, how, when and where to share this information. Provider organisations can encourage the professional institutions from which they draw their staff to address these issues. Education providers are well placed to initiate research in this area and to consider the philosophical and ethical issues involved.
• Education departments within provider organisations need to establish inservice training courses and workshops to ensure that existing staff are equipped to confidently use their relevant personal experience in their work and training for team leaders in how to foster a culture that values such experience within their teams.
• Induction programmes provide an opportunity to convey a culture that values personal experience among new recruits. At the same time as introducing recruits to policies on ‘boundaries’ they also need to encourage recruits to value the full range of their experience and use this appropriately in their work. Introductions from Chief Executives and other senior leaders on such programmes can usefully model and encourage this.
• Individual teams and services can explore the range of personal skills, expertise and experience within their teams and reflective practice sessions about how these can be valued and used.
Conclusion
Everyone working in mental health services brings not only their professional training and experience but also a wealth of personal experience (life experiences, skills and interests outside work; culture and community knowledge; past struggles, difficulties and challenges – including mental health challenges). At present, exhortations to ‘be professional’ means that many feel that they must leave half of their experience at the door. This reduces the authenticity and humanity of relationships at work and much valuable experience and expertise is lost to those using services.
Recovery is about people growing within and beyond what has happened and discovering lives they find meaningful, valued and satisfying life. Our professional skills have only limited value in assisting people to do this, but when complemented by our collective wealth of personal experience we are in a far better place to support people to explore and realise their possibilities.
References
Audet, C. T., & Everall, R. D. (2010). Therapist self-disclosure and the therapeutic relationship: A phenomenological study from the client perspective. British Journal of Guidance & Counselling, 38(3), 327–342.
Bradstreet, S. (2006) Harnessing the ‘lived experience’. Formalising peer support approaches to promote recovery. Mental Health Review, 11, 2-6.
Davidson, L., Bellamy, C., Guy, K. & Miller, R. (2012) Peer support among persons with severe mental illnesses: a review of evidence and experience. World Psychiatry, 11, 123- 128.
Deegan, P.E. (1988) Recovery: The lived experience of rehabilitation. Psychosocial Rehabilitation Journal, 11(4), 11-19.
Dorset Wellbeing and Recovery Partnership (2013) Valuing the Lived Experience of Staff Working within Dorset Health Care. Dorchester: Dorset Mental Health Forum http:// www.dorsetmentalhealthforum.org. uk/ pdfs/other/hidden-talents.pdf.
Dunlop, B.J., Woods, B., O’Connell, A., Lovell, J., Rawcliffe-Foo, S. & Hinsby, K. (2021) Sharing Lived Experiences Framework (SLEF): a framework for mental health practitioners when making disclosure decisions. Journal of Social Work Practice https://doi.org/10.1080/0 2650533.2021.1922367.
Gilburt, H., Rose, D. & Slade, M. (2008) The importance of relationships in mental health care: A qualitative study of service users’ experiences of psychiatric hospital admission in the UK. BMC Health Services Research, 8:92, http://www. biomedcentral.com/1472- 6963/8/92.
Health Education England (2020) The Competence Framework for Mental Health Peer Support Workers. Part 2: Full listing of the competences. London: Health Education England.
Henretty, J. R., & Levitt, H. M. (2010).The role of therapist self-disclosure in psychotherapy: A qualitative review. Clinical Psychology Review, 30(1), 63–77.
Holt-Lunstad J, Smith TB, Layton JB (2010) Social Relationships and Mortality Risk: A Meta-analytic Review. PLoS Med 7(7): e1000316. doi:10.1371/journal. pmed.1000316.
Lewis, A., King, T., Herbert, L. & Repper, J. (2017) Co-production – Sharing Our Experiences, Reflecting On Our Learning. Implementing Recovery through Organisational Change (ImROC) Briefing Paper, Nottingham: ImROC.
Lovell, J., O’Connell, A., & Webber, M. (2020). Sharing Lived Experience in Mental Health Services. In L. B. Joubert, & M. Webber. (Eds), The Routledge Handbook of Social Work Practice Research (pp. 368–381). London: Routledge.
Meddings, S., Morgan, P., & Roberts, G. (2019). All mental health professionals using lived experience. In E. Watson & S. Meddings (Eds.), Peer Support in Mental Health, Chapter 9. London: Macmillan.
Morgan, P. & Lawson, J. (2015) Developing guidelines for sharing lived experience of staff in health and social care. Mental Health and Social Inclusion, 19(2), 78-86.
Perkins, R. (2021) Valuing and Using Personal Experience in IPS Practice. London: IPS Grow.
Price-Robertson, Rhys & Obradovic, Angela & Morgan, Brad. (2016). Relational recovery: Beyond individualism in the recovery approach. Advances in Mental Health. 15. 10.1080/18387357.2016.1243014.
Repper, J., Aldridge, B., Gilfoyle, S., Gillard, S., Perkins, R. & Rennison, J. (2013a) Peer Support Workers: Theory and Practice. Implementing Recovery through Organisational Change (ImROC) Briefing Paper, Nottingham: ImROC.
Repper, J., Aldridge, B., Gilfoyle, S., Gillard, S., Perkins, R. & Rennison, J. (2013b) Peer Support Workers: A Practical Guide to Implementation. Implementing Recovery through Organisational Change (ImROC) Briefing Paper, Nottingham: ImROC.
Repper, J. & Perkins, R. (2013) The Team Recovery Implementation Plan: A framework for creating recovery-focused services. Briefing Paper. Nottingham: ImROC.
Ruddle, A. & Dilks, S. (2015) Opening Up to Disclosure. The Psychologist, 28(6), 458-461.
Scior, K. (2017, November 3). Honest, open, proud. The British Psychological Society Blog. https:// www.bps.org.uk/blogs/drkatrina- scior/honest-open-proud.
Watson, E. & Meddings, S. (2019) Peer Support in Mental Health. London: MacMillan International Higher Education.
Wyder, M., Bland, R. & Compton, D. (2013) Personal recovery and involuntary mental health admissions: The importance of control, relationships and hope, Health, 5(3), 574-581.
In Nigeria ImROC is a current co-applicant in a HOPE study that will commence in 2022 This project is about developing peer workers to support homeless people in Nigeria in partnership with Kings College London.
In Kenya ImROC is a current co-applicant in a HOPE study that will commence in 2022. This project is about developing peer workers to support homeless people in Kenya in partnership with Kings College London.
In Ethiopia ImROC is a current co-applicant in a HOPE study that will commence in 2022 and continue through 2023/24. This project is about developing peer workers to support homeless people in Ethiopia in partnership with Kings College London.
If services are to become more recovery focused then recovery principles and values must permeate every facet of organisations (Shepherd et al 2009). Creating recovery focused services is not about adding a new intervention or service to our repertoire but about fundamental cultural change. This centrally involves a transformation in the individual interactions – between staff and people using services and those close to them, and between staff colleagues – and the attitudes and values that underpin them. “Culture can be defined as the whole character and experience of organisational life … existing in and reproduced through the social interaction of participants” (Scott et al, 2003, p111) Efforts to change the culture within services have typically taken a ‘top down’ approach. Many services develop a kind of ‘initiative fatigue’ in trying to implement the numerous national programmes that emerge from ‘on high’ (‘the productive ward’, ‘releasing time to care’, ‘the first 15 steps’, multiple service redesigns ….). When staff are subjected to a plethora of ‘top-down’ directives they often feel alienated, disempowered and unable to use their own initiative. It is too easy for the development of recovery focused practice to be seen as yet another top-down directive.
Empowering people who use services must mean empowering relationships at the front line: recognising the centrality of such relationships in changing culture and recognising the power of front-line staff to make a very real and important difference. The focus of many of these ‘top-down’ initiatives is ‘learning from mistakes’ and putting right that which has ‘gone wrong’. Many of the policies and procedures in services have emerged from inquiries into ‘critical incidents’ and ‘near misses’ and are designed to stop such things happening again. While this may be important, on the ground the effect is often to create defensive practice in which the main aim of staff is to avoid making mistakes. If we are to create recovery focused services then we must focus and build on the strengths, achievements and possibilities of everyone using and working in them. How different would our policies and procedures look if they had been based at least as much on learning from what had gone well rather than solely learning from mistakes? Too often, in trying to develop ‘recovery focused’ practice we make lists of things that staff do that is not ‘recovery focused’. If staff are to face this challenge of developing more recovery-oriented practice they must believe that they can do a good job, that their strengths are recognised and that their positive efforts are acknowledged and valued. Too often staff perceive that a ‘blame culture’ predominates. Achievements go unremarked and it is only things that go wrong which attract attention and censure. This focus is on ‘learning from mistakes’ with scant attention to learning from success can leave staff feeling punished for what they do wrong but rarely praised for what they do right. This can lead to a kind of ‘learned helplessness’ (“ what’s the point of trying, I’ll never get it right” see Seligman, 1972). A sense of control and self-determination are diminished and too often people report feeling unable to pursue the values and ideals that brought them into this work in the first place. The sense of passivity so often reported by people who use services is reflected in the staff who provide them. The fear of ‘getting it wrong’ stifles the ‘culture of innovation’ that is so important in the development of recovery focused services (Whitely et al, 2009). The challenge in creating recovery-oriented services is to enable all staff to recognise their role in transforming culture and practice. Even in a climate of ‘top down’ rules, front line staff have the power to change individual conversations. It is often the little things, not the grand initiatives, that make the biggest difference to the experience and development of both people who use services and the staff providing them. In creating change, it is easy to rely on staff training as ‘the answer’. Training is important in the development of recovery-oriented services, but this needs to go beyond basic ‘introduction to the principles of recovery’ to encompass, for example, coaching approaches, personal recovery planning, recovery focused approaches to risk and safety, self-management approaches, shared decision making …. Such training is not just about teaching a set of skills via traditional ‘chalk and talk’ methods. It must instead explore and build on participants’ ideas, skills and experience within a framework of recovery values. It must value and build on the expertise gained from both research and lived experience of front line staff from different backgrounds/professions, people living with mental health challenges, those who are close to them, people managing/ developing services and the expertise available within communities and community organisations. If all of these groups learn together then opportunities for shared exploration and learning that can lead to mutual understanding are enhanced.
However, education/training alone is not enough. Whitely et al (2009) found four factors worked together to facilitate a recovery focused service culture: recovery focused education, organisational commitment, recovery focused leadership and a culture of innovation. There has been considerable attention paid to the organisational commitment and leadership required in the ’10 key organisational challenges’ adopted by ImROC (Shepherd et al, 2010). It is probably true to say that the primary focus in many services has been on larger service changes (such as introducing peer workers, developing recovery colleges and establishing different approaches to risk and safety). The first key organisational challenge – changing the nature of day to day interactions – remains the most elusive, alongside creating a culture of innovation and the front line leadership that is required to achieve this. The purpose of this briefing paper is to explore ways in which recovery focused transformation of services can be reflected in, and driven by, changing the nature of conversations at the front line and empowering teams to create their own solutions.
19. Creating a Recovery Focused Culture: changing the nature of conversations from the bottom up
Rachel Perkins, Julie Repper and Kirsty Giles
What sort of conversations? From the ‘patient in our services’ to the ‘person in their life’
If we are to change the nature of our conversations, we must first ask, what is the purpose of our service and the conversations within it. Traditionally it has been assumed that the purpose of services is to reduce and eliminate problems, deficits and dysfunctions. In this context we have focused on ‘the patient in our services’ and their needs in terms of what we have to offer (inpatient care, a day service, psychological therapy etc.). Our primary goal has been diagnosis, treatment and symptom reduction so our conversations have focused on the nature and aetiology of their difficulties. We have then used our expertise to prescribe solutions for them. Their personal history, strengths, goals, social circumstances, activities, values, beliefs etc. have been considered only in so far as they inform decisions about diagnosis, treatment, support and prognosis. The purpose of a recovery focused service is to help people to rebuild their lives. As surgeon, Professor Atul Gawande, said in his 2014 Reith Lectures ‘The Future of Medicine’:
“We think our job is to ensure health and survival. But really it is larger than that. It is to enable well-being – and well-being is ultimately about sustaining the reasons one wishes to be alive… Medicine must shift from a focus on health and survival to a focus on wellbeing – on protecting, insofar as possible, people’s abilities to pursue their highest priorities in life.”
In order to do this we must understand what drives the person, the nature of their ‘highest life priorities’. This means that, in thinking about recovery we need to start in a different place, not with the ‘patient in our services’ but the ‘person in their life and community’ – where they have been, what has happened to them, who and what is important to them, what they have got going for them and what they value – the ‘reasons they wish to be alive’. Symptoms, diagnosis, prognosis, treatment, support and services must all be considered not just in terms of how much they reduce problems but how far they enable the person to do the things they want to do and live a satisfying, meaningful and valued life as part of their community. We cannot understand the person in their life and community through a ‘one size fits all’ checklist. If we are to begin to understand the person, and if they are to feel heard, they need a chance to tell their own story in their own words. Simple questions like ‘What has happened?’ (rather than ‘what is wrong?)’, enable people to tell their story; taking time to listen, believing their account, exploring their experiences … can be very powerful. Personal narratives form the basis of recovery. We can learn a great deal about the person, their culture and their life if we let them tell their story about what happened to bring them to services. There will be some information that we have to collect but much may be covered in the course of the person telling their story when we take the time to actively listen.
Over time we may want to explore a number of areas:
• What the person sees as their most pressing concerns/needs. This may not be their mental health problems it could be money, housing, safety, children, relationships … it is important not to jump to conclusions and people’s concerns usually change over time.
• What the person has done to try to cope with problems they are facing. Many people have tried lots of ways of dealing with difficulties, some of which may have been quite effective. Together we can build on these and avoid replicating things they have not found helpful. What help are they already receiving? Is there anything else that they think might help?
• Their situation and the meaning for them of what has happened. The way in which they understand what has happened and how it has affected their life, relationships and roles. The practicalities of their life including their living arrangements, employment/education, finances, general health, transport/getting around, relationships community, and how these may help or hinder their recovery.
• Hope and fears. Anything that the person is frightened of, anything that makes them feel unsafe (or frustrated, or angry, or hopeless …), anything that keeps them awake at night. What might alleviate their anxiety and help them to feel safe? Who might best provide this?
• Their courage and strengths. People often understandably focus on their shortcomings and perceived deficits, weaknesses, but amid these lie a great deal that is worthy of respect:
– the courage it takes to recognise problems and seek help
– the courage and ingenuity it has taken to keep going with such difficulties
– the creativity in working out ways of keeping going
Whilst acknowledging the magnitude of the challenges they face, we must spend time discussing their own strengths and resources – and those available to them within their family, friends and communities. Solutions do not lie exclusively in services. Services can help identify, support and develop a person’s resources rather than be the sole provider. Such discussions can help people to recognise that they have some agency:
- Their personal resources: coping strategies, sources of strengths, protective factors, experiences of coping with adversity, values and activities that are important to them, inner resources that the person draws on.
- Things that make the person ‘tick’: values and beliefs, things that are important to the person, give them a sense of purpose and a reason to get up in the morning.
- Their diverse range of strengths: skills and talents, personal virtues, educational qualifications, work and work experience, interpersonal skills and resources, overcoming adversity, spiritual/faith resources.
- Their social resources: family, friends, neighbours, colleagues, support networks, services, faith communities, other communities of which they are a part and the resources within these.
- Their sources of security and hope: people to whom the person turns when they need help or solace, sources of hope and strength, spirituality and philosophy.
We cannot help people in their journey of recovery by understanding their problems and resources alone. We cannot help someone to get somewhere in their life unless we know what is important to them and where they want to go. We need to understand and help the person to explore:
- Short term goals: not just ‘getting rid of symptoms’ – what would be different? What would you be able to do that you cannot do now?
- A vision for the future: hopes and dreams for the future – what do you want to do with your life? Have these changed? What did you want to do with your life before your problems started/when you were young? If you could wave a magic wand, what would be different/how would you know things were different?
We all know that the people who are close to us often understand a great deal about our strengths and resources, our hopes and dreams, and our most pressing concerns. Sometimes they can help us to articulate these when we are not able to do so ourselves. As mental health workers we always need to recognise that, while recovery may be a personal journey, it is not one travelled alone. It is one travelled in the context of friends, families and communities. Those who the person sees as important to them may have valuable information to impart and may be valuable allies in the person’s journey.
Little things make a big difference
Probably the most difficult aspect of working as a mental health practitioner is understanding how each little thing we say or do is received by the people we are there to support. When the ward is very busy, the telephone is ringing and the doctor wants to go through the drug charts and someone comes to the office door wanting to speak to you for the third time that morning it is very easy to wave them away or tell them that you are too busy at the moment. It is all too easy to expect them to be able to see how things look from your perspective – being harassed on all sides. However, there is another perspective. The person may have lost all their friends, no-one from their family visits, they are not allowed off the ward because they are a suicide risk, and have only the staff with whom to share their loneliness and distress. You are the only person who is there for them, and you are too busy. The sense of yet another rejection is immense. There is no easy answer. You have the unenviable task of deciding which is most important: to speak to the person, answer the phone or talk to the doctor? Your instinct tells you that the person’s needs are paramount, but the doctor tells you how busy they are and you have no idea how important the telephone call might be. Perhaps you can ask the doctor to wait for a moment while you speak to the person? Perhaps you can ask the doctor to answer the phone while you do so? Perhaps you can then apologise to the person for keeping them waiting … answer the telephone and tell the caller you will ring them back … It is difficult to think through the options and their implications in the split second you have to make the decision. But perhaps the essence of taking a recovery-oriented perspective is to change some of the traditional hierarchies.
How often do we, as a team, discuss such dilemmas together? Consider how to balance priorities. ‘People before paperwork’ may be a good maxim, but this does not make the paperwork go away. There have been numerous initiatives around ‘protected time’ for staff to spend with people, perhaps this is looking at things the wrong way round?
Perhaps we should be talking about ‘protected time’ for paperwork and assume that for the majority of our time we are available to people using the service? Would we wave away, or ignore the doctor when they want our time? Probably not, we may apologise and give an explanation, arrange another time to see them … treating the people that our service is there for with the same respect as we accord colleagues is the least we can offer, but we do need to discuss and agree this as a team?
Similar dilemmas arise in every part of the service. In a busy community team, how do we respond to the person who calls several times a day asking for help? Too often the traditional response is to ‘set limits’ (‘your care worker will come and see you next week’) in an attempt to discourage ‘inappropriate attention seeking’. But how does this feel for the person who is calling you? They feel at the end of their tether, they have no-one to talk to. They really do value your help. They really do feel that they will have to take drastic action if they do not get help, even though you do not believe their situation to be critical. It is not easy. We cannot talk to a single person all the time, but from where the person sits they are continually being rejected, they feel no-one recognises how difficult things are for them. Any one of us knows how important it is that our friends and colleagues acknowledge our distress. How often do we call them to check they are OK? If we reached out on a regular basis – proactively recognising their distress rather than passively rebuffing or ignoring their approaches – then we demonstrate that we care, that we are interested, that we are there for them … if we arrange to call them regularly (daily if necessary) rather than waiting for them to call us then distress ceases to be the only way they can get the attention that we all crave. If we call them we can talk about their achievements as well. But again, this requires us to discuss and agree this approach as a team. It requires all of us to think through the person’s situation, what our role is and the consequences of different courses of action. If we rebuff the person’s approaches, all too often they do escalate their calls for help until we are unable to ignore them. What are our values? What are our attitudes to the person?
In both of these examples, the challenge is to move beyond our perspective, appreciate how things look from the other person’s shoes and recognise our common humanity. Treat the person on the ward as we would treat the doctor and treat the person who calls us repeatedly as we would wish to be treated ourselves, or how we would treat our own family members.
This latter example also illustrates the importance of the language we use and the relationship between language and thought. If we label someone as ‘attention seeking’ this defines their behaviour as a ‘problem’ to be eliminated. If instead we label them as distressed or frightened these are emotions that all of us share. Every one of us needs acknowledgement, recognition, attention, someone with whom to share hard times as well as good times. Most of us have friends, family, colleagues to provide us with this. Too often the people who use services have no-one to turn to but services. Once we start to recognise our common humanity and label their behaviour differently our response changes.
The language we use to speak and write about people has a significant influence on the way in which we respond to them. Although many services aspire to a strengths based approach, the reality often falls short. A brief perusal of the records of anyone using services reveals that the number of words describing deficits, dysfunctions and problems far outweighs the space devoted to strengths, possibilities and personal aspirations. Given the pressure of work in mental health services it is hardly surprising that we develop shorthand language. Given the prevailing focus, this short hand invariably describes problems: ‘non-compliant’, ‘difficult’, ‘attention-seeking’, manipulative’, ‘lacking motivation’. This has two consequences.
First, it describes the person and their behaviour in negative terms. Someone who does not agree with what we think is best for them may be described as ‘non-compliant’, but they could equally be described as ‘knowing their own mind’. Someone who tries to get us to do what they think is best may be labelled ‘manipulative’ while a member of staff who tries to get the person to do what they think is best is more likely to be described as a good clinician.
Second, it robs the behaviour of its context and meaning. It tells us little about the person’s situation and how they see the world, both of which are critical if we are to help them. As the ‘Independent investigation into the care and treatment of Daniel Gonzales’ (2009) says “The recovery … philosophy requires the professional to be curious about what drives the service-user, what is meaningful to him, and why..” If we say that the person is ‘non-compliant’ this tells us nothing about why the person’s perspective differs from our own and what is important to them.
Although most services aspire to offering choice, the language we use frequently assumes that our way of looking at things is the correct one and that we have the answers about how to put things right.
Typically we use ‘you’ language: you have schizophrenia, you are suicidal, you are vulnerable. This implies that our construction of events is correct and too often leads to the polarised confrontations (‘you have schizophrenia’, ‘no I haven’t’, ‘yes you have’ …) that mitigate against the formation of collaborative, recovery focused relationships. If we instead use ‘I’ language (‘I think you might have schizophrenia’, ‘I am worried that you might hurt yourself/that about other people taking advantage of you’) then we introduce the possibility of discussion of different perspectives (‘I think this, what do you think?’) that allow us to understand each other’s perspective, even if we end up agreeing to disagree.
Often we tell people what to do to make progress (‘my advice to you is …’, ‘You need to …’ , ‘You should …’). This assumes that we know what is best for the person. Just as there is no single correct construction of events, there is no single correct road to recovery. Each person must find their own way, work out what helps them and develop their own ‘personal medicine’:
“When describing their use of psychiatric pharmaceuticals or “pill medicine”, research participants also described a variety of personal wellness strategies and activities that I have called “personal medicine”. Personal medicines were non-pharmaceutical activities and strategies that served to decrease symptoms and increase personal wellness” (Deegan, 2005, p.30)
If we are to assist people in doing this our role is not to tell people what to do but to help them explore different possibilities: from ‘my advice to you is …’ to ‘some people have found X helpful, some people have found Y helpful, have you had any thoughts about what might help you?’.
As well as exploring the language we use, we also need to examine some of our accepted ways of doing things. Often we have ‘one size fits all’ rules (‘no visitors in your room’, ‘you cannot have your mobile phone’) which often reflect a kind of ‘lowest common denominator’ approach to safety: if one person is ‘not safe in the kitchen’ then no-one can use the kitchen unsupervised. Alternatively, such rules may be reinforced by ideas about fairness: it is difficult to ask Jane to get up at 8 am so she can go to a therapy group if Fred is allowed to stay in bed until 11am. Whether through ideas about safety or fairness, blanket rules prevent us tailoring services to individual needs and preferences. For example, the general rule may be ‘no visitors between 12 noon and 2pm’. If a person’s relatives have to drive a long way to reach the ward, maybe this is the only time they can visit. Keeping in touch with family and friends may be more important that sticking to blanket rules.
It is important not only to think about what we do but the way in which it is done. The rule ‘no mobile telephones’ can be delivered in different ways. The person could simply be told to hand over their phone because they are not allowed on the ward. It would be equally possible to apologise for not being able to let them have their telephone, explain why the rule exists, and how they can make a call if they want to. Common courtesy is at least as important to people using services as it is to the staff who work in them!
It is also worth thinking about the messages that our services convey about how we value those whom we serve. How do we welcome people? What do our initial appointment letters say? What messages do our ‘zero tolerance of violence’ posters, or our separate ‘staff’ and ‘patient’ toilets, convey? How does it feel to have to speak to the receptionist through a hatch or holes drilled in Perspex? How different does it feel if you are offered a cup of tea when you arrive? If the letter you are sent offering you an assessment says something about what this might entail and what a ‘Community Mental Health Team’ is? While it is important to convey the message that violence cannot be tolerated, there are lots of ways of doing this. For example, in a ward in a state hospital in the USA, the notice read “We understand that you may feel frustrated and angry at times. If you feel like this, come and talk to a member of staff – we are here to help. Our job is to keep everyone safe. Violence will be prosecuted.”
Supporting mental health workers in developing their recovery focused talents
Individual supervision and appraisal
Teams need to empower staff to work in a more recovery-oriented way. It is important to create a context in which they can develop and grow – explore all facets of their practice and contribute to their full potential. In this context, supervision and appraisal that discuss, support and encourage recovery-oriented practice are central. How can we better develop relationships that reflect our common humanity and enable people to develop and grow? How can we think about the language we use and the way in which we understand people’s challenges? How can we explore different ways of understanding why someone behaves and feels the way they do – how might things look from their perspective? How can we explore the way we do things – from initial assessments to ongoing individual work – to better foster hope, enable people to do the things they value in life and become experts in looking after themselves?
“Contrary to previous research on patients’ experiences, the themes that predominated related to the emotional not physical environment in which they stayed … relationships form the core of service users’ experiences of psychiatric hospital admission …” (Gilburt, et al, 2008)
Such supervision and appraisal needs to involve both the celebration of success and addressing challenges. We must learn from success as well as from that which is not working well. It is as important to explore why some relationships are successful – and what has contributed to this success – as well as examining how challenges might be addressed. Indeed the former can inform the latter.
Some services have used the ’10 top tips for recovery focused practice’ as the basis for recovery focused supervision2 . This list provides clear guidance for recovery focused conversations and a useful structure for identifying approaches and techniques that the individual might want to develop or improve (see Figure 1).
Figure 1: Ten top tips for Recovery focused interactions
After each interaction, the mental health professional should ask her/himself/themself, did I…
- actively listen to help the person to make sense of their mental health problems?
- help the person identify and prioritise their personal goals for recovery – not professional goals?
- demonstrate a belief in the person’s existing strengths and resources in relation to the pursuit of these goals?
- identify examples from my own ‘lived experience’, or that of other service users, which inspires and validates their hopes?
- pay particular attention to the importance of goals which take the person out of the ‘sick role’ and
- enable them actively to contribute to the lives of others?
- identify non-mental health resources – friends, contacts, organisations – relevant to the achievement of their goals?
- encourage self-management of mental health problems (by providing information, reinforcing existing coping strategies, etc.)?
- discuss what the person wants in terms of therapeutic interventions, e.g. psychological treatments, alternative therapies, joint crisis planning, etc., respecting their wishes wherever possible?
- behave at all times so as to convey an attitude of respect for the person and a desire for an equal partnership in working together, indicating a willingness to ‘go the extra mile’?
- while accepting that the future is uncertain and setbacks will happen, continue to express support for the possibility of achieving these self defined goals – maintaining hope and positive expectations?
(cited in Shepherd, Boardman, & Slade, M., 2008, p.9)
The possibility of introducing 360 degree appraisal at team level might also be considered, including the experience and contribution of people who are using the service in this process. For example, feedback might be provided by using the INSPIRE assessment tool (Williams et al., 2011) which focuses on the relationship the person has with a mental health worker and the extent to which they feel this supports their recovery as part of a person’s appraisal. Alternatively, people who use services might be trained to provide clinical supervision with groups or teams of staff.
Recognising and rewarding individual expertise and effort
Recognition and reward for achievements is critical and cannot be left to supervision and appraisal alone.
In their ‘effort-reward’ model of job stress, Siegrist et al (1990) describes the problems that arise if effort and reward are out of balance; people are working very hard and receive little acknowledgement or reward for their efforts then well-being, morale and health are compromised. Reward in this context is not all about pay – it is also about status and recognition. Clearly pay and promotion are one way of recognising achievements, but alone they are a rather crude and infrequent mechanism that ensure that most people’s efforts, most of the time, go unacknowledged.
Some services have recognised this by instituting various forms of awards for teams. While these may be an important way of acknowledging success, they too are infrequent and leave the day to day initiatives and successes of most staff uncelebrated.
Little things make a big difference and are the building blocks of recovery-oriented culture and practice. These little things often take a great deal of effort and ingenuity that goes unacknowledged. If no-one recognises the effort you are making then you rapidly stop making the effort. What motivates most of us is the sense of having achieved something – made a difference. If the effort-reward imbalance is to be restored then it is critical to acknowledge these successes. We need to build in ways of recognising and celebrating these day to day successes and relationships as part of our routine work.
On a day to day basis, simply noticing what others in the team have done is critical. A simple ‘well done’ or ‘thank you’ from a colleague or team manager can go a long way. Reflective practice sessions, care plan review meetings, ward rounds and staff handovers offer a real opportunity to do this. Typically these are problem-focused: problems are identified and solutions sought. If the course of action decided is successful it is rarely noted, we simply move on to the next problem. This leaves everyone with a sense of failure ‘nothing we do works’. In order to recognise and celebrate success, some teams have started identifying a specific time in review meetings and ward rounds for discussing successes and exploring what can be learned from these. One ward decided to finish the handover at the end of each shift by going round and asking each staff member to describe something that they had achieved in the shift: a success, however small, or something of which they were proud. This not only recognised what staff had achieved but it left them going home after work on a positive note. Similarly, the manager of a community team instituted a ‘little miracles’ meeting at the end of each week. Towards the end of a Friday afternoon, all team members of the team who could make it were invited to come together for ‘tea and cakes’ and share the ‘little miracles’ that had happened during that week: these were written down on a sheet of paper and left on the wall as a reminder for the rest of the week. Tokenistic as such initiatives may sound, their impact on enabling people to recognise what they have achieved should not be underestimated.
As well as celebrating success within teams, it is important that these successes are recognised at a management level. Too often middle managers feel besieged from all sides – told from on high to make sure that cost and performance targets are achieved and from below that there are insufficient resources. Managers are more likely to recognise success if they know what individuals and teams have achieved. How often do individuals and teams feed-back their small but important success stories to offer a different narrative to that of performance targets? Providing feedback on the things that are important can do much to create a more recovery-oriented discourse within the service that can do much to change culture.
This might be achieved via newsletters that contain brief reports of progress and success in individual work with individual people using services. For example, one ‘snippet’ related how someone on an admission ward had refused to have a bath or wash: numerous confrontations and abuse followed when the person was repeatedly exhorted to bathe and relationships deteriorated. A member of staff spent time talking to the person and discovered that she thought it was unhygienic to bathe in facilities used by lots of strangers and ascertained that she would be happy to have a bath in her own home … so when the ward was quieter at a weekend the staff member took the person to her home to have a bath. One organisation started including narratives of success as a routine part of its Key Performance Indicator reporting systems. At the start, some cynics thought that these would go unnoticed – that ‘they’ would only be interested in the numbers, not the people. This proved wrong: the brief narratives brought the figures to life and reminded managers and commissioners what the service was really about.
As well as acknowledging achievements, recognising and using expertise of individual staff is also important both in making services more recovery oriented and improving job satisfaction. Staff often have a range of professional training and experience (for example, working with families, addictions, trauma informed care etc.) which they are not able to use in their day to day work. In many teams, people only work with their designated ‘caseload’, so the input available to people using the service depends on the skills of their designated care co-ordinator. This is both a waste of skills and limits the options available to people using services. We need first to have a register of the skills that are available within the team and second, ways of enabling people using the service to access the skills within the team that they need. The creation of ‘lead’ roles can go some way to addressing this. For example, someone with family work training might be the ‘family, friends and carer’ lead and offer family interventions offer this to people across the team, not just to those on ‘their own’ caseload. Staff also bring a range of other talents and expertise from outside their professional careers: interests, hobbies, community networks and contacts and a range of cultural competencies. Staff satisfaction, and the experience of people using the service, can be enhanced by recognising the talents and interests of staff and using these. For example, a nursing assistant had been a journalist in the country of her birth – once these skills had been recognised she worked with service users to produce accessible, ‘plain English’ leaflets about the ward and the activities/ supports available. A staff member who had qualifications as a personal trainer used these to help individual clients to develop their own, individual exercise regimes. Identifying staff interests and talents enables a matching of clients and staff with similar interests and backgrounds can create a ‘win-win’ situation by fostering improved relationships and improving job satisfaction.
Building on strengths at team level: Using Team Recovery Implementation Planning
While it is important that each mental health practitioner reflects on their own practice, we all work together in teams and the whole is more than the sum of its parts. To work together effectively to promote recovery, and support the endeavours of individual workers, the whole team needs to reflect on their purpose and approach.
A service cannot promote recovery unless recovery focused principles and practice are embedded and owned at the grass roots. We need to work together to create more recovery oriented services and bring together the collective expertise, creativity and ingenuity of those at the front line – both mental health workers and the people who use services – with that available among relatives friends and communities. The Team Recovery Implementation Plan (TRIP) offers a framework for doing this. Initially developed in Nottingham, it has been refined in use across the UK and beyond (see Repper and Perkins, 20133 ). It has proved a useful approach to the development of recovery focused practice in the full range of services (from high secure settings through acute inpatient wards and community teams to voluntary sector services) and has assisted in breaking down ‘them’ and ‘us’ barriers by changing the relationship between staff and people who use services.
The TRIP is founded on co-production. It involves recognising people as assets and building on the strengths within the team: the resources of both staff and people supported by the service. It is founded on the principles of mutuality and reciprocity – breaking down barriers and blurring roles: staff and people using the service share responsibility for both designs and delivery of the plans. It extends the resource base by including peer, personal, professional and community networks. The service becomes a catalyst for change rather than a creator of change by enabling people to lead their own recovery and the development of recoveryoriented services and empowering people to develop a range of resources in peer networks and communities to support them in their journeys. Not only does coproduction result in better services by harnessing additional capacity and expertise it also promotes the recovery of those involved by enabling them to move from passive recipient of services to active agent.
The TRIP involves four key components⁴ :
- Identifying assets: the resources that exist within the team among staff and people using the service: not just the experience of using/providing mental health services but a) ‘hidden talents’ (other skills, qualifications, interests, experiences) and b) contacts and networks within communities. For example, one Early Intervention Team had someone using the services who was interested in the development of ‘apps’. Using this talent, and the team manager’s knowledge of sources of funding, the team developed ‘My Mind Western Trust’ app⁵ to support people with mental health conditions and help them take back control as part of their TRIP. In a ward in a secure psychiatric service, a band was formed using the musical talents of a number of staff and inpatients as part of their TRIP.
- Benchmarking progress in recovery focused practice. Based on good practice statements drawn from the Recovery SelfAssessment – Provider Version (O’Connell et al, 2005) and ImROC’s 10 Key Organisational Challenges (SCMH, 2010), teams discuss and rate their progress. This is a collaborative process in which staff and people using the service recognise and celebrate what they have achieved and identify ways of moving forward and building on what they have done. For example, one voluntary sector service had already introduced people using services onto interview panels and decided they could build on this by coproducing job descriptions and person specifications with people using the service.
- At the end of the benchmarking process, front line staff and people using the service, alongside people who are close to them and community partners, come together to identify priorities and develop action plans. These might best balance impact and ease of implementation by including some ‘quick wins’ and some longer term projects. The challenge is not just about ‘doing more’ it is about ‘doing differently’. The range of targets identified by teams is extremely broad, from making waiting areas more recovery focused, to the collection of recovery stories, changing the format of review meetings, shared entries in notes, ‘trip advisor’ style ratings of community facilities, co-producing information booklets about the service; inviting external agencies to run activities on wards; changing the initial assessment letter to make it more friendly and give people information about what the assessment would entail and what questions would be asked … Whatever the priorities identified it is important that these are co-delivered. Each priority is co-led by a staff member and someone using the service, assisted by other staff, people using the service, relatives/friends and community partners/agencies as appropriate. Many teams have found that not everything has to be done by staff. Tapping the expertise of people using the service is equally important. For example, one community team have decided to provide an ‘information corner’ in their waiting room. Staff have not got the time to run this, but there are people using the service who are keen to help on a voluntary basis. The team has made available resources to collect information leaflets about a range of issues (from opportunities in the local community to self-help materials) and people using the service introduce people to these and help them to use them. There exist a wealth of talents among service users that can be tapped!
The TRIP has also been used by corporate services and non-clinical teams to help them focus on what coproduction means in their own area and how they can better support the development of recovery focused practice at the front line. For example, one Business Development Department set up a group of people who had used services to assist in tendering for new services; and one executive team decided to introduce ‘recovery impact assessments’ of all new policies and service developments; a Finance Department produced a ‘simple to understand budget statement’ for hostels so that this could be shared easily with staff and residents in deciding how some of the available budgets should best be spent; and an IT Department worked with people using services to enable them to have access to the organisation’s intranet.
Critically, Team Recovery Implementation Planning is not a ‘one-off’ exercise but an ongoing process of co-producing and co-delivering action plans. Neither is it a quality rating scale or a ‘tick box’ exercise but a way of supporting recovery-oriented ways of working in teams: an heuristic tool to promote collaborative, ‘bottom up’, service development. Just as recovery is about recognising and building on strengths, TRIP provides a framework for bringing together the wisdom and resources of staff, people using the service, those who are close to them and community partners to create an environment in which all can grow and develop. Experience suggests that it is the collaborative process of using TRIP, rather than the specific content of the action plans, that is most critical in creating a more recovery focused culture and practice and changing the nature of interactions within teams.
Maintaining and developing recovery-oriented practice: the centrality of leadership
Whitley’s (2009) research into the core components of Recovery focused services demonstrated the importance of recovery focused leadership. Although recovery is now a central tenet of policy and practice guidance for all professional groups, in order to be enshrined in organisational culture it needs to be an explicit part of a shared vision that is understood and clearly led at every level of the organisation.
The principles of recovery translate effectively into principles for leadership. If services are to realise the changes in conversation discussed in this paper then they need leaders who inspire hope and belief in the possibility of improving services; facilitate a sense of personal control or agency among staff in the development and delivery of recovery focused initiatives, and create opportunities for personal development based on strengths, interests and experiences. These characteristics bear an uncanny resemblance to ‘transformational leaders’ (see Bass, 1997; Burns, 1978) who are recognised by their commitment to working with their organisation/team to identify needed change, creating a vision to guide the change through inspiration, and implementing the change in tandem with committed members of a group. Unlike transactional leaders who work within the status quo, transformational leaders strive for culture change to drive improvement and performance and stir their employees to look beyond their own self-interest for the good of the group (Investors in People 2017).
Bass (1997) identified four key components of transformational leadership. These have direct relevance to leading recovery focused culture change:
Idealized Influence – the leader serves as an ideal role model for followers; the leader “walks the talk,” and demonstrates the aspired behaviours of the whole team consistent with the overall vision. Within any mental health team, the influence of a leader who clearly models recovery focused behaviour; prioritises the needs of people using the service over paperwork, explicitly appreciates the contributions, ideas and achievements of staff members; always uses recovery focused language and maintains a strengths based perspective, is invaluable in transforming the culture.
Inspirational Motivation – Transformational leaders have the ability to inspire and motivate followers. By embodying recovery principles even in the most stressful situations, displaying an unwavering belief in the potential of people, recognising the challenges of competing demands but consistently seeking creative solutions, the transformational leader motivates others to share their beliefs and actively change their own behaviours.
Individualized Consideration – Transformational leaders demonstrate genuine concern for the needs and feelings of their team. This appreciative approach chimes with the strengths based and personalised aspects of recovery. If every member of the team feel that they are valued and supported as an individual then they are empowered to perform to their full potential.
Intellectual Stimulation – the leader challenges followers to be innovative and creative and constantly seeks higher levels of performance. Although transformational leadership has been criticised for being too ‘soft’, in reality it is about constantly striving Conclusion to achieve a shared vision and ensuring that everybody is fully committed to this: challenging their mindsets, ideas and beliefs to drive growth and performance, encouraging creativity, collaboration and the pursuit of excellence.
Whilst critiques of transformational leadership focus on the possibility of dependence on the leader and the need for a certain personality type to take up this role, research demonstrates the effectiveness of the approach. Transformational leadership is associated with greater leader effectiveness, higher staff commitment, role clarity and wellbeing and more positive outcomes than other leadership styles (Investors in People, 2017).
Conclusion
Although the culture of any organisation is highly influenced by the values and aspirations of Senior Managers, we contend that the experience of people using services is crucially dependent on the values, behaviours and beliefs of all practitioners. In order to change the conversation at the front line, it is essential to recognise, celebrate and develop both people who use services and the staff members with whom they have closest contact. It is also essential to develop relationships with community resources and facilities so that people using services have opportunities to build roles, relationships and meaningful lives beyond services.
All of this requires a a shift in priorities, practices and critically relationships so that everyone’s contribution is valued and there exists a collective vision that is owned and shaped by people working in and using services, their family members and the communities in which they live. This inclusive, valuing and supportive culture needs to place an emphasis on strengths and achievements and learning from success rather than problems and things that have not worked out as we had hoped. It replaces excluding, technical, pathologizing and professionalised language with personal, accessible, appreciative conversations. Relationships are underpinned by courtesy, respect and mutual learning. A recovery focused culture is led at every level, in every part of the service with genuine partnership and value afforded to everyone who uses the service and works in it.
References
Bass, B. M. (1990). From transactional to transformational leadership: Learning to share the vision. Organizational Dynamics, (Winter): 19-31
Boorman, S. (2009) NHS Health and Well-being Review. Interim Report, London: Department of Health
Burns, J.M (2010) Leadership. Harper Perennial Political Classics
Deegan, Patricia E. (2005) The importance of personal medicine: A qualitative study of resilience in people with psychiatric disabilities Scandinavian Journal of Public Health. 33 (66 suppl): 29–35.
Dunlop, B.J., Woods, B., O’Connell, A., Lovell, J., Rawcliffe-Foo, S. & Hinsby, K. (2021) Sharing Lived Experiences Framework (SLEF): a framework for mental health practitioners when making disclosure decisions. Journal of Social Work Practice https://doi.org/10.1080/0 2650533.2021.1922367 Accessed 7.7.21
Department of Health (2011) The Public Health Responsibility Deal, London: Department of Health
Department of Health (2015) The NHS Constitution, Department of Health Dorset Wellbeing and Recovery Partnership (2013) Framework for Using and Sharing Our Lived Experience within Health and Social Care.
Dorset Healthcare NHS Foundation Trust and Dorset Mental Health Forum. http:// www.dorsetmentalhealthforum.org.uk/pdfs/ other/supporting-staff-recovery.pdf
Gawande, A. (2014) ^The Idea of Wellbeing. Lecture 4 in the Reith Lectures 2014: The Future of Medicine, Indian International Conference Centre New Delhi, 20th December 2014
http://downloads.bbc.co.uk/radio4/openbook/2014_reith_lecture_4_delhi.pdf accessed 25/9/2021
Investors in People (2017) https://www. investorsinpeople.com/transformationalleadership-what-is-it/ accessed 17 September 2018.
Perkins, R. (2021) Valuing and using personal experience in IPS practice. London: IPS Grow
Perkins, R., Rinaldi, M. & Hardisty, J. (2010) Harnessing the expertise of experience: Increasing access to employment within mental health services for people who have themselves experienced mental health problems, Diversity in Health and Care, 7, 13-21
Repper, J., Aldridge, B., Gilfoyle, S., Gillard, S., Perkins, R. and Rennison, J. (2013a), Peer support workers: theory and practice ImROC briefing paper, London: ImROC, NHS Confederation Mental Health Network/Centre for Mental Health, London. http://www.imroc. org/media/publications/
Repper, J., Aldridge, B., Gilfoyle, S., Gillard, S., Perkins, R. and Rennison, J. (2013), Peer Support Workers: a practical guide to implementation, ImROC briefing paper, London: ImROC, NHS Confederation Mental Health Network/Centre for Mental Health, London. http://imroc.org/media/ publications/
Seligman, M. E. P. (1972). “Learned helplessness”. Annual Review of Medicine. 23 (1): 407–412.
Shepherd, G. Boardman, J. and Slade, M. (2008) Making Recovery a Reality. Nottingham: ImROC/London: CMH)
Whitley, R., Gingerich, S., Lutz, W.J. & Mueser, K.T (2009) Implementing the illness management and recovery program in community mental health settings: facilitators and barriers. Psychiatric Services, 60, 202- 209.
1 https://www.safewards.net/interventions/know-each-other
2 http://imroc.org/what-is-recovery/recovery-top-tips/
3 http://nhsconfed.org/~/media/Confederation/Files/public%20access/ImROC_briefing6_TRIP_for_web.pdf
4 http://imroc.org/media/publications/imroc_team_recovery_implementation_plan-3/
5 https://itunes.apple.com/gb/app/my-mind-western-trust/id802203395?mt=8
The Live Well model brings together best evidence for community development, social prescribing, health coaching, health education and volunteering – all linked and developed through a core coproduction forum. This paper describes the development and outcomes of the pioneer Live Well service – Let’s Live Well in Rushcliffe (LLWiR).
16. Developing Primary Care Networks and Community Focused Approaches: A Case Study
The Let’s Live Well in Rushcliffe Team
The ‘Live Well’ Model Report: An integrated approach to support, enable and empower people who are lonely, inactive and/or have long term conditions(s) to live well in their communities. The Let’s Live Well in Rushcliffe Team, April 2019
Acknowledgements
A big thank you to the very many people who have contributed to LLWiR.
This paper describes the model we have developed by working together as a large heterogeneous group of people with a passion for our local communities and a commitment to developing a community focused approach to support people who are isolated, inactive and / or have long term conditions.
Many of us live with ongoing health conditions or care for a family member who does; some of us offer medical services, health or social support; others work in local community services and facilities, others volunteer or are employed within the team. Some have received support from the Live Well team, others have worked on the evaluation and others have provided managerial support to the project.
Figure 1. Key Components of the Live Well Model
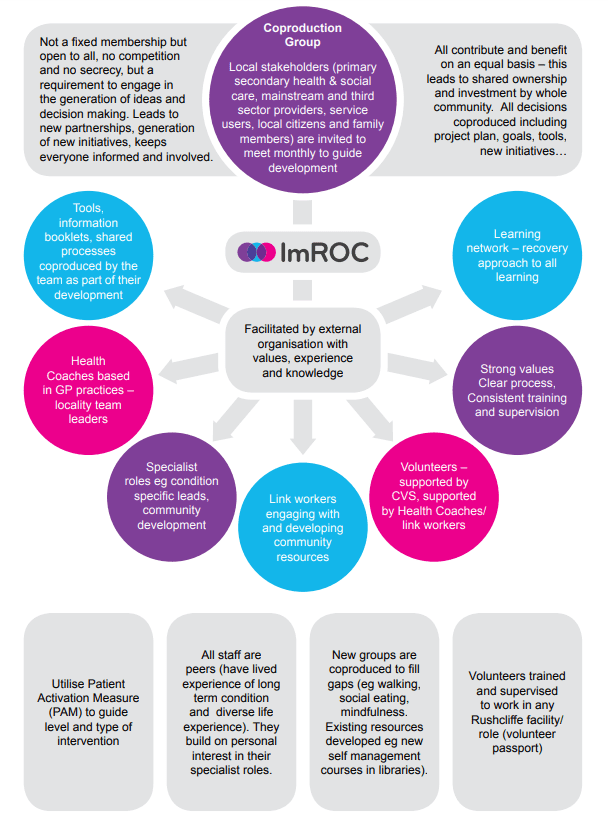
1. Introduction
The Live Well model brings together best evidence for community development, social prescribing, health coaching, health education and volunteering – all linked and developed through a core coproduction forum. This paper describes the development and outcomes of the pioneer Live Well service – Let’s Live Well in Rushcliffe (LLWiR).
LLWiR was developed to meet the needs of people living in Rushcliffe who have complex long term physical and/or emotional health conditions and/or who are isolated, excluded and/or find services difficult to engage with. The service is open to self-referrals as well as referrals from any primary care services, social services, the voluntary sector, family members and community facilities. It offers initial engagement, assessment and health coaching based in GP practices, and where appropriate this leads on to an introduction to a link worker who supports people to engage in activities related to their personal goals and works with community resources to extend and develop opportunities in the community.
The coproduction group is the core of the project. Regular meetings with a large group of stakeholders not only co-constructed the initial model, but facilitates an ever expanding range of additional initiatives including a learning network offering educational opportunities in a range of facilities, multiple community cafes (where people can meet others in a safe place, attend learning opportunities and buy refreshments); a volunteer pathway and strong links into existing services. Additional features of the model include the provision of a small funding resource for new initiatives; employment of peers (people with their own experience of long term conditions) in all roles within the team; and external facilitation and project management from a Recovery focused organisational development organisation (ImROC).
A full evaluation of the project was undertaken by Nottingham Trent university to assess impact on health and service use. 1483 referrals were received in the first 13 months of service provision . This study reported significant improvements in patients’ physical and mental wellbeing after the initial four month period which were maintained after eight months. There was also an increase in community group membership at 4 months which reduced slightly by 8 months. There was a decrease in both primary and secondary care usage over the evaluation period. The economic evaluation of the programme attached savings to the improvements in health as well as the changes in health and social care usage. Projected over a year post-baseline assessment, this estimates a ROI of £1.00. In other words, if the patient benefits recorded for the first four months are continued for the rest of the year, the programme will recoup 100% of its costs by January 2020.
“Well, most of a population’s health and wellbeing is determined by environmental factors, and things that are not to do with healthcare. And, you know, sometimes the traditional medical model, if you like, has been very, you know, our role is to just do the medicine and that’s it. But we work in a system, we work in… All these things are interdependent, and if we want to, we might not be the experts on it, but if we want to help our patients more and help the population, then we need to access these sort of broader things”.
GP
“I think social prescribing is having the time to explore an individual’s needs regarding their wellbeing and then tailoring support to the individual’s needs, rather than just saying, ‘You can go to X, Y or Z’. Not assuming that just because somebody has a diagnosis of X that they’ll need X, but really exploring an individual’s needs and seeing and supporting the individual to achieve those goals while promoting self-management. There is no point providing a wonderful service and then, when we go, the person is back at square one”
Health Coach
I think as we work with individuals to get them engaged more with the community, the community itself then benefits by having more people engaged with it, so it becomes almost organic and it can grow and develop itself, just to help to meet the needs of its members, I guess.
Link Worker
“… theory’s all very well, but I see the patients I’m referring coming to see me less. I can have a look at their notes and see what’s been written and see that they’re making connections”.
GP
The health coach and the patient, we work together to assess a way forward, essentially looking, in very broad terms, at goals and areas for goals to be placed in. This could be over one, two or three sessions, there’s no time limit on it [lines omitted] the end result is to come up with goals and then to break those goals down into achievable steps. If that needs some support in the community, in terms of physical support to help them get to a new group, for example, or to help look at the way they shop differently or something like that, then we have link workers.
Health Coach
2. The Context
2.1 The National Context
The pressures on todays’ health and social care system are well documented: life expectancy is increasing and numbers of people living with long term conditions now account for 70% of the healthcare budget; there is a widening gap in health inequalities largely due to social factors (like finances, education, housing and isolation) – issues which are not routinely addressed by health services; public expectations of services are rising and new treatments are continually developing, placing ever greater economic pressures on services.
Solutions to this complex picture have been proposed in the 5 year forward view1 and further detail is provided in the 5 year forward view for mental health2 and the GP forward view3. All of these documents place an emphasis on primary prevention through public health initiatives; secondary prevention through primary and secondary health care and self-management as people are further enabled to manage their own wellbeing through education, coaching and personal budgets. In addition these visions for a healthier future call for greater integration of primary and secondary services – including acute and urgent care; health and social care, mental health and physical health services, and far stronger partnerships between statutory services and the voluntary sector alongside the development of more confident, capable communities.
Many new structures and approaches are developing to support the transformation of health and social care services, for example Multi-speciality Community Providers that integrate expertise in one place based team; HiAP (Health in All Policies) informed by the Marmot review4, with localities seeking to reduce Health Inequalities by actively addressing the health implications of all developments in a community: transport, industry, housing, environmental issues, education etc. Vanguard sites to lead innovative new developments in health and social care with dedicated funding for pilot projects; Sustainable Transformation Plans, recently replaced by Integrated Care Systems working across systems in an area based approach to integrate and synthesise services and sectors to meet the needs of the local population. Yet the simultaneous development of integrated approaches, alongside the generation of evidence to demonstrate their effectiveness and efficiency, whilst ‘the aeroplane is in flight’ – continuing to provide treatment and care for the local population -is a huge ask for even the most motivated and well-resourced teams.
2.2 The Local Context
When NHS England published ‘Next Steps on the Five Year Forward View’5 it signalled the intention to move to Accountable Care Systems (ACS) in the NHS. NHSE describes a key duty of an ACS to: “Deploy (or partner with third party experts to access) rigorous and validated population health management capabilities that improve prevention, enhance patient activation and supported self- management for long term conditions, manage avoidable demand, and reduce unwarranted variation ….”. Nottinghamshire (specifically the Greater Notts STP) has been identified as an area that will adopt this way of working in the first wave.
Principia is a key element of the Greater Notts STP situated in Rushcliffe, a rural and suburban area to the south East of Nottingham city with a population of 125,0766. Although the proportion of the population aged over 65 years in Rushcliffe is 15% higher than the average in England, the CCG area has the least deprived population in Nottinghamshire. In terms of its Index of Multiple Deprivation (IMD) score, Rushcliffe (with a score of 8) is also better than the England average of 22 (England worst – 51; best 6) and it has a lower unemployment rate (0.8% compared to the England average of 1.8%), lower child poverty rates 7.2% compared with the England average of 18.6%. As expected with significantly lower levels of deprivation, Rushcliffe displays good health outcomes as compared to the England average despite its older population. Deaths from all causes in under 65 years is at 73.9 compared to the 100 England; hospital admissions caused by injuries in children (0-14 years) is 68.2 compared to the 109.6 England average and obesity and excess weight prevalence’s are significantly better in Rushcliffe compared to England across all ages, and in many instances have the best levels in the country.
As a Multi-specialty Community Provider (MCP) organisation Principia is a local partnership of GPs, patients and community services which has been selected as one of 50 ‘Vanguards’ across the country with funding to lead significant changes in the way local health and social care services are delivered. As part of this, Principia MCP is a registered intensive “Empowering People in their Communities” (EPC) site (see appendix 1). This involves an implementation plan that includes the following elements:
- Work with communities to grow these resources to meet health and wellbeing needs.
- Build a network of supported volunteer roles.
- Deliver of systematic self-care support for people with COPD, diabetes and with 3 or more long term conditions.
Principia’s ambition is to support its communities and clinical teams to begin to change the culture and approach to health and wellbeing. There is recognition that although many good areas of practice exist, but there is disconnection, fragmentation and sometimes duplication between health, local authority and third sector services. There have been tangible successes in delivering improved care and outcomes for people with physical health problems, supported by coordinated and motivated primary care services. However the “disparity of esteem” still exists for people with serious mental illness, whose life expectancy remains far lower than the rest of the population. Advances in healthcare have not been matched by progress in services to prevent illness and support self-care.
Principia aim to address these issues by investing in people and services to address this fragmentation, encourage systematic assessment of patient activation, and support routine referral of people all along the spectrum of health “risk” for self-care support. At the same time, gaps in provision will be identified with a view to further investment and development in years to come.
Principia Vanguard MCP divided population health management into 10 programmes, under the leadership of different clinical and managerial teams. However, there was a recognition that supported self-care and activation is needed across the whole population, and incorporated five MCP workstreams 1-5 (primary prevention, self-care, secondary prevention, ambulatory care sensitive conditions and mental health). The objectives of these workstreams included:
- Increase patient activation in people who see health coaches and community connectors
- Increase uptake of local authority and 3rd sector services provided to support selfcare
- Identify gaps in these services
- Reduce the financial impact on the NHS of people who access these services
3. Developing the ‘Live Well’ Model
3.1 Our Approach
The Live Well model developed through an ongoing co-productive process, continually drawing on the expertise and experience of a range of stakeholders (including General Practitioners and CCG staff with MCP roles for primary prevention/self-care), Local Authority staff including public health, reenablement, parks and leisure and IT staff, voluntary sector groups, emergency services, housing, employment, sports and leisure organisations) and increasingly, as the project progressed, responding to the experiences of staff working in the Live Well team, their clients and the community members with whom they worked. The power of coproduction has been well described (see Box 2): it is about bringing together all available expertise and experience around a shared challenge, to agree on goals, consider research evidence, share personal and professional experience and suggest possible courses of action. A coproduction group can discuss, debate, develop, test, amend and evaluate ideas over time. New solutions are generated, new group members are identified, everyone can both contribute and benefit in a synergy that is not possible in exclusive, closed or solely professional groups.
The overall model was informed by the ‘The Triangle that Moves Mountains’ philosophy that has been successful in developing complex social policy transformation in Thailand7. This focuses on three factors: providing relevant evidence, research and examples of practice from elsewhere; working with local people, organisations and resources to develop a ‘community sensitive’ approach over time; and engaging and influencing local leaders to create political pressure to transform systems, (see Box 1).
The Live Well coproduction group met regularly throughout the project. Initially agreeing on the nature of existing challenges, the values, aims and objectives to be met (see Box 2). Subsequently reviewing research underpinning potential approaches along with the expertise and experience presented by different members to determine the values of the project, an outline service model and a profile of the people who the project would target. There was a strong commitment to making the service accessible to anyone who felt they might benefit from it so the service initially targeted anyone over 18 years that is registered with a GP Practice in the Rushcliffe.
The ideas of the coproduction group were developed into a proposal which was successfully submitted for funding from Rushcliffe MCP Vanguard Site. The implementation of the model was then considered by the group and the project goals, objectives and time plan were agreed; values were developed. Relevant expertise within the group was utilised in the recruitment of staff (who were required to bring diverse lived and life experience which they could explicitly apply in their practice); the training of project staff (with input from coproduction group members for example Public Health England; NHS England; Local Authority leads for coproduction and for community learning.
Box 1. Our Approach: ‘The Triangle that Moves Mountains’
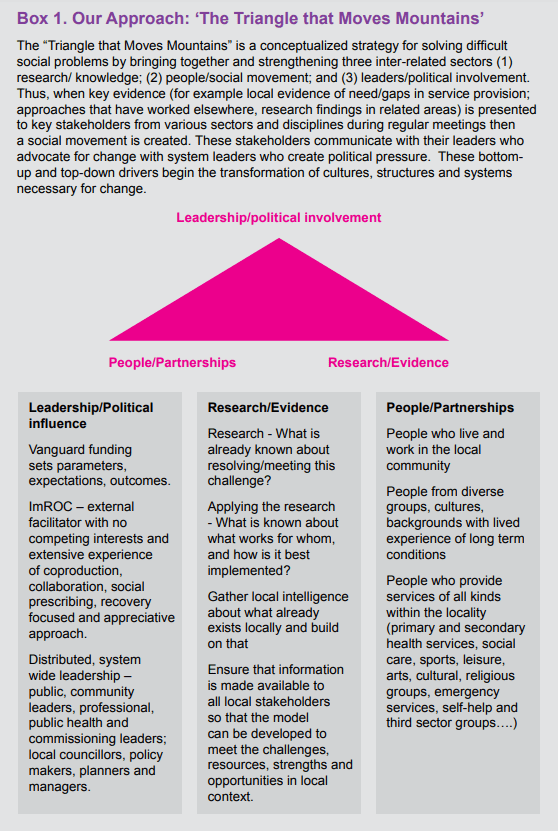
Perhaps the most innovative aspect of the coproduction process was the ongoing influence of the group on emerging challenges and the development of new initiatives for the whole community (for example the development of new learning opportunities across the whole patch and the development of community cafés in rural areas, a university campus and small towns). These partnership initiatives – involving religious groups, local public houses, sports centres, libraries, subject specialists and self-help groups – attracted an ever increasing group of coproduction group members, including key influencers, leaders and funders so that the model gradually infiltrated and strengthened a widening range of opportunities with the synergy to impact on the whole population in the locality.
“I came along to the Co-production meeting yesterday … and what a wonderful meeting it was! I found myself reflecting on the meeting last night and how powerful the sharing of stories, backgrounds and passions were … I fully appreciate that it took time but I feel it was incredibly valuable in developing those vital relationships and genuinely coproducing a community endeavour – full of admiration for you and what Lets Live Well in Rushcliffe is achieving!”
Newark Mind – co production partner
3.2 Project Leadership
One of the counter-intuitive aspects of any coproduction is the need for leadership. Although coproduction is all about partnership on an equal basis, unless the process is informed, facilitated, led and ‘serviced’ then it will stagnate as everyone waits for someone else to speak up or develop some rules or make a decision…. Yet the challenge facing any local provider who leads the coproduction process is the inevitable competition that exists between themselves and other members: all are likely to be chasing the same limited funding and the elevation of a local group to lead a project can exacerbate rivalry. Commissioning of services is generally based on a competitive tendering process which means that some services win and others lose out on funding. Coproduction, on the other hand, is all about mutual benefit generated in an open, transparent, sharing culture: win-win.
ImROC initiated the coproduction process in the LLWiR project well before any funding was won. Following an approach from a local GP for ideas about meeting the needs of people with severe depression, it was ImROC who suggested that rather than prescribing any solution, we should seek the views of the local community and relevant services and groups about what might work – in a co-productive process. The success of the early coproduction meetings led to increasing commitment to the project by service providers, commissioners, local citizens and ultimately funders. This has driven the ambition and momentum of the project, which has been sustained by well organised, engaging, relevant and mutually beneficial coproduction meetings which reliably lead to inclusive action and progress. The role of ImROC (see Box 2) has been to:
- manage the project in line with the project plan identifying and mitigating potential risks;
- facilitate coproduction meetings and ensure that decisions and plans made in the group are implemented as agreed enable the project to evolve organically over time in response to the experiences of project staff and clients and in line with the decisions made in the coproduction group;
- seek relevant evidence and expertise to ensure that the coproduction group is working with best research evidence and practice guidance rather than relying solely on local people’s experience (as required in the Triangle that Moves the Mountain);
- lead the recruitment, training and employment of staff;
- enable and oversee the evaluation of the project within the defined budget.
Overseeing the project, a steering group (with local and national representation from all sectors as well as ‘patient’ and peer worker representation ), chaired by a local GP met regularly to review progress, challenges and risks against the project plan.
Box 2. ImRO
Box 3. Coproduction
Coproduction is all about bringing together everybody involved in an issue to work in partnership, make decisions, deliver solutions, evaluate, review and respond together. As Nesta1 point out: “Co-production challenges the conventional model of public services as a ‘product’ that is delivered to a ‘customer’ from on high, and instead genuinely devolves power, choice and control to frontline professionals and the public”. By facilitating reciprocal and equal relationships, coproduction enables all participants to both contribute and benefit from the process so that change becomes more relevant, inclusive and effective. The New Economics Foundation2 have claimed that coproduction is an effective way of building up the local economy engaging, enabling and expanding the resources available. In his introduction to the NEF report, Edgar Cahn explains how coproduction is the root of community development:
“If social capital is critical to the well-being of society, then we must ask what its home base and source is. Social Capital is rooted in a social economy – and surely, the home base of that economy is the household, the neighbourhood, the community and civil society. That is the economy that co-production seems to rebuild and to reconstruct”.
NEF describe the elements of co-production within public organisations as:
- See people as assets, not burdens on an overstretched system – people are the real wealth (and wasted resource) in society – more than passive recipients in services.
- Invest in the capacity of local communities – so that communities shift from expecting professionals to have all the answers and take greater responsibility for themselves, building social and cultural capital, nurturing economic and mental capital.
- Use peer support networks to transfer/develop knowledge and capabilities so become a networked organisation with multiple partners.
- Reconfigure services to blur the distinction/change the power balance between producers and consumers of services – value work differently and create a demand for all contributions and reward appropriately.
- Public service agencies thus become catalysts for change rather than simply providers.
ImROC has described their experience and learning about coproduction and conclude with Ten Top Tips for Coproduction3:
- Gather the right people for the job.
- Just get started and build momentum around your shared purpose.
- Spend time agreeing the structure and the values of meetings.
- Support every member to contribute to their full potential.
- Tackle the challenge in small steps.
- Listen, listen, listen.
- Back up decisions with evidence.
- Beware the comfort zone.
- Look to the bigger picture.
- Cherish what you create.
1 NESTA (2010)Public Services Inside Out. London: NESTA
2 Ryan-Collins, J. and Stephens, L. (2008) New Economics Foundation: Co-production – a Manifesto for growing the core economy
3 Lewis, A., King, T., Herbert, L. and Repper, J. (2017) 13. Briefing paper 13. Co-Production – Sharing Our Experiences,Reflecting On Our Learning. Nottingham: ImROC
3.3 Developing project goals and agreeing underpinning values
The Live Well model aims to empower and enable local people to live well within their communities drawing on local resources and meeting local needs. It has the potential to target different groups within the population (for example older people, younger people, people with specific conditions; people from different minority ethnic groups); to focus on prevention (through health education, smoking cessation, weight reduction, community inclusion) and/or ongoing support (for people with existing conditions); to prioritise different activities (such as workplace wellbeing, access to employment and engagement with services). The specific goals of every project will be different – depending on the funding opportunities, local priorities and the local situation. However, it is important for the whole community, represented in the coproduction group, to be clear and united in setting the goals and values of the project.
The process of agreeing goals and values is an effective way of bringing together the coproduction group in productive relationships. The agreement of goals provides a clear focus and parameters for the project and is key to the establishment and ongoing membership of the coproduction group. The agreement of underpinning values for the project set the culture of the coproduction process, the values are the guiding principles that are most important to the group about the way that they work together. They guide decision making, influence the nature of conversations, inform the training and supervision of project staff and the ongoing development of the project.
3.3.1 The Goals of LLWiR – developed and agreed by the Coproduction Group:
We aim to improve the lives of people in Rushcliffe who are isolated, inactive and/ or have long term condition(s) by:
- Supporting and enabling them to do the things they want to do – demonstrating an increase in roles, relationships and activities and improvement in personal goal attainment scales.
- Increasing their understanding of their own condition and improving their ability and confidence in managing their own condition – demonstrating improvement on PAM Scores.
- Reducing their reliance on health services – demonstrating reduction in crises, unplanned admissions and frequency of GP attendance.
- Increasing engagement in local communities – demonstrating increase in activities, engagement with local community amenities, and achievement of personal goals.
- Increasing partnerships between different organisations and sectors to reduce duplication and gaps between services – demonstrated in discussions at coproduction meetings.
- Identifying gaps and developing new, accessible opportunities – demonstrated by collecting weekly updates about their community development activities from link workers.
3.3.2 The Values underpinning LLWiR – developed and agreed by the coproduction group
Live Well draws on the extensive experience of coproduction group members. Their collective belief in the potential of all citizens reflects a ‘Recovery’ approach. The term Recovery has been reclaimed by people with mental health problems to refer to their ability to live well in the presence or absence of symptoms of their condition8. For services to focus on Recovery they need to shift their focus from symptoms and problems to strengths, assets, experience and goals. For people to achieve recovery they need to identify their own goals – and work out what sort of information and support will enable them to achieve these goals. For communities to support recovery they need to become more confident about their own abilities to accommodate, support and benefit from the contributions of people who experience different conditions. Our values are quite simply:
To always inspire Hope by demonstrating our belief in people: everyone has the potential to live a more fulfilling and satisfying life.
To empower people to take Control of their own condition, their own treatment and their own lives.
To enable people to access the Opportunities (facilities, activities and resources) that will enable them to achieve their life goals9.
3.4 Integrating the service into GP practice
Living Well was originally conceived as part of the Rushcliffe NHS new care models vanguard- Principia MCP -and a business case was written and accepted to fund a pilot project that has evolved to become Lets Live Well in Rushcliffe. The return on investment was predicated on a reduction in the use of NHS services by people supported by the service. It was designed to be integrated and colocated with NHS GP services: this was necessary to get the service up and running, using the regular contact that people have with GPs and health centres to drive uptake and visibility.
In the first phase there have been three different referral pathways. Firstly people who are opportunistically identified during consultations with GPs are offered a health coach assessment. Secondly, patients attending for their annual long term condition health check, usually with a nurse, can be offered a referral. Finally, GP computer disease registries were analysed for people with characteristics suggesting they may benefit from the service, and invited by letter. Examples included people with serious mental illness at risk of developing further long term conditions.
Referrals have been made as easy as possible using a simple “E-referral” system embedded in the clinical IT system used by health care professionals every day. Health Coaches and Link workers use the same system to record their activity, making it simple for NHS professionals to see what has happened.
General Practice teams continuously recognise people who’s health wellbeing are influenced by psychological and social factors more than medical issues. It has been a source of frustration for GPs and nurses that they have had neither the time to address these problems, or any places to direct patients for support.
As GPs on the steering group have reflected, many clinicians have felt it is their job to deal with medical problems alone, with many very reluctant to explore concepts such as activation, address the social determinants of health, or support lifestyle change. With these factors in mind, there has been a concerted effort to communicate the benefits of Living Well during the first few months. GP leaders have visited practices, attended MDT meetings and presented at educational events. The evidence base for this approach, detailing the potential improvements in quality of life for Rushcliffe citizens, alongside reductions in use of NHS services has been emphasised. Real-life stories of local patients whose attendance at the GP surgery has dramatically dropped following their introduction to the service has helped support this message.
‘There is a feeling, supported by the early evaluation interviews, that hearts and minds are changing amongst medical teams. All practices, and most GPs have made at least one referral to Living Well. Stories of people’s lives being transformed are being discussed in clinical teams. The early adopters and enthusiasts are delighted to have an option to help people in a truly holistic way’
GP on steering group
4. Components of the Live Well model
4.1 Community Development
The Live Well model seeks to address the needs of the local population not only by changing local services, but by engaging and developing the communities that they serve. This allows health and social care services to focus on those people requiring specialist treatment and support, whilst communities offer roles, relationships and supports to maintain the wellbeing of the whole population. All communities offer a wealth of untapped resources, expertise and interest. There is ample evidence of the generosity, expertise and support that exists within communities, perhaps most marked in those facing crises – seen most recently in the UK following the Grenfell disaster. Community development approaches have rapidly developed over the past three decades (although different names have been used to describe this work – increasing social capital, community empowerment, improving social value, participatory and action research methods…). They essentially refer to working with communities to identify and build on existing resources, develop new resources, give everyone the opportunity to both engage and benefit from their community and contribute to it (see Box 6).
Within the Live Well project, new relationships have been developed in the coproduction group leading to partnership initiatives to meet the need of Live Well Clients and local communities. For example the Local Authority funded Library service has worked with link workers to a) increase the range of learning opportunities accessible and relevant to Live Well clients (including selfmanagement courses); b) increase the use of existing library facilities and opportunities by Live Well clients; and c) develop new courses and groups running in libraries. These new courses and groups are available to everyone in the community, not only Live Well clients – thus benefitting the whole community.
‘Following a ‘meet your village’ event in East Leake, LLWiR will be working with the Rotary Club, Lings Bar hospital and others to establish a Dementia café in East Leake and Kegworth. Rushcliffe Golf club want to meet with LLWIR and have offered use of their facilities to support a dusk time walking group. They are approaching Sport England to explore opportunities for golf to be more accessible in the community.’
Health Coach
Link workers and Health coaches are employed in one specific CCG care delivery group (localities of North, Central and South) and an early priority for each of these ‘placebased’ teams was community asset mapping. This involved visiting local resources and facilities and sharing the nature and purpose of the Live Well team as well as gaining an understanding of the resource: who it serves, what it offers, how accessible it is, whether they would like any further information or engagement with the Live Well team. This work was invaluable in the success of the Live Well project. Local teams were able to signpost clients to appropriate activities and to the right people within those activities. Local resources were able to join the coproduction group if they were interested. They might receive training and other types of support from the Live Well team to improve their accessibility and confidence (so, for example training on ‘working with people who hoard’ was offered at the request of the Fire Service and Housing Associations). Some worked in partnership with the team to develop new activities; others offer material support to the team (for example free facilities for groups).
Since starting the Notts County Football in the Community groups in Cotgrave and East Leake, we have had one gentlemen who has really benefitted from the groups who struggles with anxiety. He said: “I have opened up more to you guys in two sessions than I have with any therapist”
Link Worker Community Development
Setting up the East Leake Walking Group
I met with an individual at a health week event in December 2017 in East Leake Library. This individual and her daughter were keen to start a local walking group as there was nothing around locally with the nearest group being in Ruddington. Together, we agreed to make this idea a reality and begin building the group together. I met with the two on several occasions and helped them with creating a digital flyer to advertise the group as well as getting the group onto the Notts Help Yourself website. I helped to get the advertising material printed and distributed. On the 11th of January the group had its first walk with a good group of people turning up. I supported this group continuously on the walk each week thereafter. The walk commences each Thursday at 1.30pm and ends with a cup of tea or coffee and a chat in the local café. It has been fed back that the group is a really brilliant way to be active for those who want gentle exercise, but also a fantastic group of people to socialise with who are very welcoming and generally nice.
Anne, the walking group lead had this to say recently:
“Last week we had a bumper turn out with 9 people walking, two new people and 10 for tea!
We have now had 19 walks, 18 different people involved and 111 attendances which average out at about 6 people each week.”
This group is looking like something that will be around for a long while in the future.
Box 4. Community Development
What is community development?
Community development is variously defined as either a process or an outcome; a socio-political movement or an interpersonal phenomenon1. It includes:
- Empowering communities by strengthening the capacity of people as active citizens through their community groups, organisations and networks, and
- Empowering institutions and agencies to work in partnership with citizens to shape and determine change in their communities.
- Promoting the voice and action of disadvantaged and vulnerable groups by working with excluded groups in active process of participation, learning, action and reflection.
- Promoting strong communities by facilitating full active partnership in a mutual and reciprocal solution focused process focused on common problems or the prevention of such problems; increasing the confidence and capacity of local communities to understand, accommodate and appreciate everybody in the local population.
- Facilitating collaboration between individuals, interest groups, government, local organisations and funding agencies.
- Supporting the local population to define and voice their own wishes and needs and maximise their political influence (to achieve funding, support, recognition…).
In practice these processes redefine the relationship between the secondary and primary stakeholders so that the role of the outside agent shifts from ‘expert’ to enable; from advisor to catalyst releasing the ‘power-from-within’ the primary stakeholders2.
What do we mean by Community?
Within the Live Well model, we are primarily focusing on the population of a defined geographical locality, within this locality we focus on specific communities – these might be defined by interest, condition, profession, religion, politics, gender, culture or age, and we prioritise those whose needs are not being met with existing resources. The people who we work with are often multiply excluded on the basis of different characteristics such as (dis)ability, personal resources, race, religion, reputation and age. People with mental health problems, particularly schizophrenia, are among the most excluded in Western society so particular attention is paid to their inclusion in all Live Well coproduction processes.
Asset-Based Community Development3
(ABCD) “While deficit approaches focus on problems and deficiencies and designs services to fix these problems, they create disempowered and dependent communities in which people become passive recipients of services rather than active agents in their own and their families lives”. The Live Well model draws on ABCD as it is a well tried and tested approach which: Identifies health enhancing assets in a community; Sees citizens as co-producers of health and wellbeing rather than passive recipients; Promotes community networks and relationships that provide caring, mutual help and empowerment; Supports individuals wellbeing by increasing selfesteem, coping, resilience, relationships and personal resources; and Empowers communities to take control over their own future and values and create tangible resources such as services, funds and buildings.
1 Wallerstein N. Empowerment to reduce health disparities. Scandinavian Journal of Public Health, 2002, Suppl 59:72–77
2 Fetterman DM. Empowerment evaluation: building communities of practice and a culture of learning. American Journal of Community Psychology, 2002, 30(1):89–102
3 http://www.assetbasedconsulting.net/uploads/publications/A%20glass%20half%20full.pdf
4.2 Social Prescribing
Many people in the UK live in situations that have a detrimental effect on their health, indeed, it has been estimated that around 20% of patients consult their GP for what is primarily a social problem and 15% of GP visits are for social welfare advice10. Social prescribing is a way of linking primary care patients who have ‘psycho-social problems’ with sources of appropriate, non-medical support in the community. This has been seen as one way of making General Practice sustainable11 an approach to integrating health and social care with the voluntary and community sector.
Social prescribing began as a way of engaging people with mental health problems with activities and supports within their communities as a non-medical referral option to improve health and wellbeing12. It has developed into various forms, all offering support to people who are inactive, isolated and/or struggling with a long term condition. Whilst there are social prescribing initiatives that focus solely on ‘prescriptions’ for nonmedical support from general practitioners, others are based entirely in the voluntary sector. Whilst some focus entirely on arts or exercise prescriptions, others offer prescriptions for broader social support. Whilst some have narrow referral criteria, targeting people with certain conditions or levels of disability, others offer support to anyone who is referred or self-refers. Whilst some link people to a few selected groups, others link people with a range of resources determined by the person’s personal interests and goals. Whilst some offer information and signposting, others offer face to face practical support.
Social prescribing schemes generally have three key components:
i) a referral from a healthcare professional,
ii) a consultation with a link worker and
iii) an agreed referral to a local voluntary, community and social enterprise organisation.
“After working with the link worker I swim regularly which helps me manage my pain, I drive to new places unsupported, which helps me do the things I want to do! My next step is to volunteer with LLWiR”
Studies into the effectiveness of social prescribing are generally small, conducted over short time periods with different outcomes measured, however results are promising. The most recent systematic review of research into social prescribing concludes that: “Such interventions have been found to be cost-saving13, able to address the mental health needs of hard-toreach populations14, 15and help to combat loneliness16. Importantly, the provision of care outside clinical settings can facilitate the development of social relationships and widen individuals’ social networks. … Social relationships are positively associated with better physical and mental health, and have been shown to reduce mortality risk to an extent that is comparable to stopping smoking and reducing alcohol consumption17”,18.
The Live Well approach to social prescribing has been developed in the coproduction group. Rather than providing a service that simply connects clients with existing groups, this has focused on link workers engaging with people to identify their own goals. Using our ‘Green Book’ (another coproduced product, see Box 9), people are supported to develop their own wellbeing plan, working out how they can keep themselves as well as possible, how to recognise and respond to signs that they are having a bad day or ‘relapsing’, and planning action they can take to prevent a crisis. The Green Book also draws on the Five Ways to Wellbeing19 to support people to generate personal goals and prioritise ‘SMART’ action plans to begin working towards these goals. Link workers will support people over 6-8 sessions; for some people, support will include identifying and engaging in existing local groups or activities, for others it will focus on changing their behaviour – in relation to diet, daily routine, exercising or socialising; for others it will involve considering their employment – diary/time management, organising appropriate adjustments to their role, accessing relevant training. Where there are no appropriate groups or resources locally, the local Live Well team will consider how and whether to set up a new group, or they may come back to the coproduction group for their advice and ideas about how to respond – asking the group: who can help with this, what exists elsewhere, where is there relevant expertise and experience in this area.
An individual was referred to me via the GP. The individual struggles with managing their Type 2 Diabetes as well as feeling lonely due to the passing of their partner. The individual was not routinely taking their medication to best manage their Diabetes as they didn’t see the point. Since my contact with the individual, we have sorted home delivery of her medication to help her to be better organised in taking them at the correct times. We also discussed using weekly tablet trays and this individual has since not missed any of her medication. We worked a lot on motivation and have seemed to make good improvements. They feel much better in themselves and we are now working with them to join a walking group, something the individual wants to do to meet new people and get some exercise to help the management of their condition. Very positive steps are being made and I can see the difference in this individual’s attitude myself. They are much more positive now since our contact.
Box 5. The Green Book
Everyone referred to Live Well is provided with a ‘Green Book’. This is a self-completion tool with information and encouragement to work out how to keep well, prevent relapse, identify personal goals and make a plan to achieve these goals.
The Green Book draws on Wellness and Recovery Action Planning (WRAP)1 to help people recognise their own understanding of their condition and build on this to keep themselves well. It begins by supporting people to identify what makes them feel well, what seems to make them unwell, stressed or miserable (triggers) and how they recognise signs that they are becoming unwell. It goes on to help them use this information to make a plan to increase the things that keep them well and mimimise or avoid makes them, then to make a plan for managing early warning signs.
The Green Books uses the Five Ways to Wellbeing2 to help them to identify some personal goals that are meaningful them and build on their interests and experiences. Evidence suggests small changes in these areas can help to improve personal wellbeing:
- Connect – There is strong evidence that indicates that feeling close to, and valued by, other people is a fundamental human need and one that contributes to functioning well in the world.
- Be active – Regular physical activity is associated with lower rates of depression and anxiety across all age groups. Exercise is essential for slowing age-related cognitive decline and for promoting well-being.
- Take notice – Reminding yourself to ‘take notice’ can strengthen and broaden awareness. Studies have shown that being aware of what is taking place in the present directly enhances your well-being and savouring ‘the moment’ can help to reaffirm your life priorities. Heightened awareness also enhances your self-understanding and allows you to make positive choices based on your own values and motivations.
- Learn – Continued learning through life enhances self-esteem and encourages social interaction and a more active life. Anecdotal evidence suggests that the opportunity to engage in work or educational activities particularly helps to lift older people out of depression. The practice of setting goals, which is related to adult learning in particular, has been strongly associated with higher levels of wellbeing.
- Give – Individuals who report a greater interest in helping others are more likely to rate themselves as happy. Research into actions for promoting happiness has shown that committing an act of kindness once a week over a six-week period is associated with an increase in wellbeing.
The Green Book helps people to think about ways they could increase their activities in these areas and uses this process as a way of enabling them to set personal goals and make more detailed action plans.
Since the Green Book is a loose leaf booklet, individuals can add their own notes, and they can insert specific tools and information (coproduced by the Live Well team) as relevant to their own condition and lives.
1 http://mentalhealthrecovery.com/
2 http://issuu.com/neweconomicsfoundation/docs/five_ways_to_well-being?mode=embed&viewMode=presentation
4.3 Health Coaching
One of the underlying problems of our time is the construction of all health and social care problems as requiring professional help – from health and social services. We are increasingly a nation of ‘consumers’ socialised into believing that the best sources of help for our problems – whether long term pain, disability, mental health and physical problems or housing, employment and isolation – comes from public services. We have lost confidence in our own abilities to manage our own lives and conditions, and the breakdown of traditional communities contributes to a lack of confidence in communities as a resource to which we can contribute and from which we can gain meaningful roles and relationships. Many people who are house bound, disabled by ongoing mental and physical conditions, anxious about going out and meeting people, lacking confidence following diagnosis or illness have no understanding of their condition and how to manage it, they are not aware of what is possible for them or of what sort of supports and activities exist in their local community. In reality, we can all make a difference to our own health – whether preventing conditions arising or managing a long-term health conditions. It has been estimated that as many as 70 per cent of premature deaths are caused by behaviours that could be changed (Schneider, 2007). Clearly, huge benefits could be realised if people felt able to take a more active and engaged role in their own health care.
Research into ‘patient activation’ demonstrates the positive impact that empowering people to manage their condition and thereby continue a more active and meaningful life can make on health inequalities, outcomes, the quality of care and the costs of services (Box 10). A new role has developed to support patient activation: ‘health coaching’, which focuses on enabling the person to gain new skills in managing their condition, encouraging a sense of ownership of their health, considering changes to their social environment to support their wellbeing, and linking with relevant education, activities and opportunities.
Within the Live Well Model, the Health Coaches receive training in coaching and patient activation; they work closely with primary care teams to clarify their role and the sort of people who might benefit from health coaching. They supervise the link workers in their area and are the local contact point for anyone wanting to contact the team or considering making a referral. Health coaches see all new referrals to the service, initially engaging and assessing their situation and agreeing a way forwards that is most suitable for that person. Health coaches are not experts in long term conditions and their treatment, rather, ‘they are experts in not being the expert’20, they work in partnership with the client to find out the information and gain the skills the person needs. This might be through locating relevant literature either on the internet or in paper form; it might involve finding a relevant course or self-help group in the locality, it might be solution focused work or problem solving to work out a plan of action. The focus is largely on health related behaviour, with support being provided over 1-5 sessions. Where ongoing or social support is needed the health coach introduces the client to a link worker.
Saw a 54yr old in Jan 2018…BMI 35, 40u /week daily drinker, hypertensive with a new diagnosis of type 2 diabetes. Offered meds for the DM but he declined saying he wanted to adjust his lifestyle. He’s been working with the health coach on goal setting for the past 4 months. In 12 months, he has dropped his Hba1c from 63 to 44, drinks lightly now on only two days /week and has lost a decent amount of weight.
It’s all going really well, I’m drinking less, I’ve not had a cigarette for 4 weeks and my link worker is supporting me to become a volunteer– Thank you!”
Feedback from GP
Box 6. Patient Activation and Patient Activation Measure (PAM)
In the Kings Fund’s review of the research into patient activation, Hibbard and Gilbert1 conclude that patient activation is a better predictor of health outcomes than known socio-demographic factors such as ethnicity and age, with people who are more activated being significantly more likely to attend check-ups, adopt positive behaviours (eg, diet and exercise), and have clinical indicators in the normal range (body mass index, blood sugar levels, blood pressure and cholesterol); and people who are less activated being significantly less likely to prepare for a medical visit, know about treatment guidelines or be persistent in clarifying advice. Not surprisingly, patient activation scores are related to cost to services with less-activated patients costing approximately 8 per cent higher than more-activated patients. Studies of interventions to improve activation (such as Health Coaching) show that people who start with the lowest activation scores tend to increase their scores the most, suggesting that effective interventions can help engage even the most disengaged.
The Patient Activation Measure2 (PAM) is a simple, evidence-based tool for establishing the capacity of individuals to manage their health – and then using that information to optimise the delivery of care. PAM scores have been demonstrated to be related to most health behaviours, many clinical outcomes, health care costs and patient experiences. The Principia Vanguard applied to NHS England to be an intensive pilot site for “Empowering People & Communities” and as a result were accepted to use PAM, one of three intensive EPC sites across East Midlands. Within the Live Well model, the PAM is included in all baseline assessments to establish the intensity and focus of subsequent support. It is measured at three monthly intervals to provide both the health coach/link worker) and the patient with feedback about progress.
The PAM consists of 13 statements about beliefs, confidence in the management of health-related tasks and self-assessed knowledge designed to assess the extent of a patient’s activation. Patients rate the degree to which they agree or disagree with each statement giving a combined single activation score of between 0 and 100. For the purpose of intervention, these scores are divided into four groups or levels of activation, each requiring a different level and type of support.
- Level 1 – Individuals tend to be passive and feel overwhelmed by the idea of managing their own health. They may not understand their role in the care process.
- Level 2 – Individuals may lack the knowledge and confidence to manage their health.
- Level 3 – Individuals appear to be taking action but may still lack the confidence and skill to support their behaviours.
- Level 4 – Individuals have adopted many of the behaviours needed to support their health but may not be able to maintain them in the face of life stressors.
1 Hibbard, J. and Gilbert, H. (2014) Supporting People to Manage their Health: An introduction to Patient Activation. London: Kings Fund
2 Hibbard JH, Collins PA, Mahoney E, Baker LH (2010). ‘The development and testing of a measure assessing clinician beliefs about patient self-management’. Health Expectations, vol 13, no 1, pp 65–72.
4.4 Education
Education is central to personal ‘power’, identity and autonomy, status and life choices, so inevitably it is closely linked with health and wellbeing. In relation to general education, an additional four years of education lowers five-year mortality by 1.8 percentage points; it also reduces the risk of heart disease by 2.16 percentage points, and the risk of diabetes by 1.3 percentage points. People who are better educated report having lower morbidity from the most common acute and chronic diseases (heart condition, stroke hypertension, cholesterol, emphysema, diabetes, asthma attacks, ulcer) and are substantially less likely to report that they are in poor health or have anxiety or depression and spend fewer days in bed or not at work because of disease. Whilst we can rarely address a lack of general education, we can offer health related education to enable people to understand how to keep themselves well. In a review of the impact of health education, Lawn et al (2011) report improved self-management, reduced crises and unplanned admissions, reduced frequency of service use, improved social networks and greater confidence and self-efficacy. The development of Recovery Colleges (Perkins et al, 20011; 2018) offering coproduced, experiential and recovery focused education, primarily for people with mental health problems – but increasingly open to the whole population – has demonstrated the huge popularity, accessibility and benefits of learning with and from peers (see Box 11).
The Live Well project did not set out to provide self-management courses or group based learning opportunities, but it became apparent that many clients wanted to learn about their condition and how to manage their lives with their condition, but accessible, condition specific courses were not always available. Whilst a Recovery College does exist in Nottingham this is only open to people using secondary services and in primary care teams funded to provide courses.
The coproduction group considered this challenge and the Local Authority funded Inspire21 project offered to work in partnership with link workers to enhance the accessibility of courses and the range of learning opportunities already offered in local libraries to meet the needs of Live Well clients. In addition, specific courses were developed in response to identified need, for example healthy eating courses have been developed in partnership with a local nutritionist to provide dietary information alongside cookery classes for people who want to develop their own understanding and skills but do not feel able to join mainstream education.
As the project progressed, it became clear that local groups and services would also like to be able to access training to enable them to maximise their contribution to local people with long term conditions. This challenge was discussed at the coproduction group who drew on their expertise, networks and experience to focus on the best way of strengthening learning opportunities within the locality. The group were able to produce a list of learning opportunities already available and identified the need for additional courses focusing on self-management. It was agreed that a part time trainer should be employed to coproduce (with a peer link worker) bespoke training in subjects nominated by the coproduction group, like ‘mental health awareness’, ‘setting up community groups’, ‘understanding and managing hoarding behaviour’, for any member of the coproduction group, any of the Live Well team and any clients who would like to attend. In addition, to sustain the provision of training, Live Well staff were offered ‘training for trainers’ an accredited training course that enabled them to coproduce and co-facilitate training wherever it was needed.
Box 7. Recovery Colleges – Core Principles and Evidence of Effectiveness
Recovery Colleges have developed over the last ten years to become a key feature of mental health services in the UK and beyond. More recently they have developed in primary care, forensic, homeless, housing and third sector services. They offer courses based on the wishes and needs of those who use them and embody a shift from a focus on therapy to the inclusion of education to enable students to learn how to manage their own condition and their own life – housing, diet, sleep, activity, relationships …. They explicitly bring together the expertise of lived experience and professional expertise in an inclusive learning environment in which people can explore their possibilities.
Although there are now more than 85 Recovery Colleges in England, to date there are no formal controlled trials exploring their effectiveness. However, there is a strong and consistent body of evidence from an increasing number of uncontrolled studies of the positive impact of Recovery Colleges in several areas.
- The effectiveness of Recovery Colleges on people facing mental health with the vast majority of students achieving personal goals, moving on to volunteering, training, open employment and education.
- The quality of recovery-supporting care: Recovery Colleges are popular and students are highly satisfied with their experience.
- Positive evaluation of the staff attending Recovery Colleges
- Recovery Colleges are an effective vehicle for driving a change in the culture of organisations with improved staff attitudes and understanding and a higher value placed on coproduction and peer support.
Perkins et al22 review the development and research into Recovery Colleges and conclude with 6 key principles that both define them and account for their success.
- They are based on educational principles but do not replace formal individual therapy or mainstream educational opportunities.
- Coproduction, co-facilitation and colearning lie at the core of their operation: they bring together lived/life expertise with professional/subject expertise on equal terms.
- They are recovery-focused and strengths-based in all aspects of their functioning. They do not prescribe what people should do but provide a safe environment in which people can develop their understanding to keep themselves well and build skills and strategies to live the lives they wish to lead.
- They are progressive, actively supporting students to move forwards in their lives both by progressing through relevant courses that enable them to achieve their identified goals ,and by identifying exploring possibilities outside services where they can move on in their lives and work.
- They are integrated with their community and can serve as a bridge between the services and communities: serving as a way of promoting a recovery-focused transformation of services more generally, and creating communities that can accommodate people with long term conditions.
- They are inclusive and open to all. People of different ages, cultures, genders, abilities and impairments, as well as people in local communities who have health conditions/physical impairments), people who are close to them and people who provide services.
Education – Case example
I have been supporting an individual in the Rushcliffe South area to reconnect with their local community in the hope that this will support them to further manage and reduce their anxiety. This anxiety has adversely affected employment and living arrangements, and social circumstances.
The individual wants to start gaining some more independence and manage her anxiety throughout the whole day. I have worked with the Individual to explore their needs and identified the possibility of attending courses which would benefit wellbeing, ideally close to home and with small class sizes. We have researched some local groups with smaller class sizes and closer locations.
Part of this work has been to liaise with Inspire (the library education service) to see if they could extend their courses to more local libraries. Inspire have now offered a taster course at the local library, with a possible view to expand. The individual has been accompanied to first few courses and says that accessing the course at their local library helped them to build friendships and networks with people in their local community. Further joint investigation of what the Community can offer is underway regard a range of activities. All the time the team is allowing the individual to express her needs and then look to see what the community can offer.
4.5 Peer Support
There is increasing evidence that support from a person who shares similar experiences and is managing their own wellbeing improves outcomes when compared with standard support23. Although this evidence draws on research undertaken exclusively in mental health services, the LLWiR team and the coproduction group agreed that employees providing health coaching and link working would bring their own experience of living with a long term condition themselves, or caring for someone who does – in addition to the other desirable and essential characteristics of community support workers. This built on ImROC’s experience of developing opportunities for peer support (including training, supervision, supportive employment and development of peers), it also provided an inspirational example for people using the service to follow and was consistent with the coproduction approach at the heart of the project.
Peer support refers to the explicit use of personal experience in the support of others who share similar experiences. The core characteristics of effective peer support have been identified (see Box 8) and the training provided for all employees focused on them understanding and applying these principles in their practice.
Employing peer workers ensures that the project remains true to its values with integral reflection on the accessibility, appropriateness, relevance and likely effectiveness of the developing approach. People who live with a long term condition and manage it on a daily basis bring practical expertise and experience to every aspect of their work. However, the successful and effective employment of peer workers requires exemplary employment support so that they stay well in work and contribute to their full potential. This is not ‘special’ support, but the kind of consideration that every employee would benefit from. For example consideration of reasonable adjustments, a personal wellbeing at work plan, access to additional supervision when times become difficult for an employee.
The preparation and training of all team members was given careful consideration within the coproduction group, and by the ImROC team. An over view of their training is given in Box 9. This was supplemented with monthly team meetings which provided a forum for ongoing development as training needs arose. Issues addressed in this way included: Supporting people in acute crisis; Supporting people to set personal goals; Starting and ending relationships with people you work with.
“The service is one of the major big things that helped me to get better. In fact, I would say that it has been the most important thing in me getting better. I had never spoken to anyone on that level before or with someone who knows what it feels like. Whenever my link worker left I would always feel massively better and like a weight had been lifted off my shoulders. It has taught me how to be compassionate to myself and look after myself”
Case example – Peer Support
In the first meeting with this A, they were very negative. They believed nothing could help them and that they were unable to physically do anything and therefore felt like they had no purpose and no belonging. This person suffers from depression as well as some physical conditions that mean they cannot use their hands, which is how they used to earn their living.
In the second meeting, I tried to keep the conversation as positive as possible. However, the individual kept bringing the conversation back to the past and everything they had lost. I explained through a diagram that things in the past can feel like a large chunk of your life and that we think these feelings will get better in time and that the impact of the past on our lives will get smaller with time. However, I understand that this is not the case. I gave an example of a time when I experienced loss myself and explained that for me, the impact of that on my life didn’t get smaller as time went on. Therefore, to make the impact of that loss in my life smaller, the only thing to do was to grow my life in other areas. Make sure I was seeing friends/family, make sure I was active and doing things, make sure I was taking notice of what I did have and making sure I was trying and learning new things. This seemed to resonate with the individual quite well. The meeting from that point on seemed very positive and we spoke of things they were looking forward to and came up with a plan of what we could discuss in future meetings to help produce of ideas in which the individual could try to ‘grow’ their life to make the past seem smaller in comparison to their overall life.
They said “I really appreciate you coming to see me, talking really does help”.
4.6 Specialist Areas of Interest
The Live Well model offers a range of interventions and types of support to people with a range of different conditions and life circumstances. It is simply not possible for every employee to hold every piece of information about community resources, conditions, approaches and population groups. It therefore works well to support link workers and health coaches to develop an area of special interest. This might draw on their life experience or their previous employment experience, their interests and hobbies or their cultural awareness. For example, an employee with experience of work in a sales and marketing job might take a lead on social media developments; an employee with interest or a qualification in teaching might lead the development of learning opportunities; another might take a lead on sustaining community developments, or working with younger/older people.
These areas of specialist interest need to have direct relevance and utility within the project, so they might not be apparent when the project starts, but can evolve over time. They ae yet another way of modelling Recovery focused practice: building on personal strengths and interests, developing individuals so that they can progress their career.
Within LLWiR, it became apparent that community groups developed by link workers needed additional attention to ensure that they become sustainable in the longer term with less input from the project. A link worker with previous experience of community development was given the lead on monitoring, sustaining and creating a consistent process for developing new community groups and resources. Another worker with an interest in IT and apps development took a lead on working with the University to develop a mobile phone application which listed details of local groups and resources already existing in the area, building on the resources listed on the Notts Help Yourself website. Once it became apparent that volunteers would be employed in the project, one of the link workers with experience of staff support and supervision took the lead on working with the Council of Voluntary Services to develop the volunteer pathway. Many other opportunities have been taken up by employees in line with both their own areas of interest and the evolution of the project.
In order to be successful, these roles need to be rewarding in themselves rather than exploitative. It is important to integrate the roles in personal development plans, support individuals to access relevant training and ensure that supervision covers these areas.
When carefully managed, this system of distributed leadership not only provides personal development opportunities for employees on the project, it also offers a framework for project development, a method of growing the sum of expertise within and available to the whole team, and an approach to working with coproduction group members in a rational and effective manner.
4.7 Developing a Library of Relevant Resources
Resource Library
As the project has worked with many people who face similar challenges, have similar goals and present similar dilemmas for workers, a huge amount of work has been undertaken by both employees in the service and the people they support to research appropriate coping strategies, supportive tools, services, groups, activities. Rather than individuals repeatedly undertaking the same research, all relevant material has been collected together, reviewed and develop into Live Well guides.
So, for example there are now toolkits, information booklets and lists of useful resources for many different long term condition and there is a growing compendium of local services, facilities, activities, groups and clubs available in the local area. These are formatted in such a way that people can insert them as pages into their Green Book.
As the team has developed, there have been a number of difficult situations which have fallen outside the experience and role of the team so the team has drawn on external expertise to develop clear pathways and guidance for managing these. For example, the team has developed Ten Top Tips for supporting someone expressing suicidal ideas and a pathway for accessing appropriate help.
At present these resources are all maintained on a team shared drive, but as the LLWiR mobile phone app is developed this ever expanding library of information will be available to all those using the service.
4.8 Volunteers
The Live Well model offers time limited support (up to 6 meetings with health coaches and/or up to 6 meetings with link workers). Inevitably there are people who would benefit from longer term support to enable them to continue to work towards their goals. Similarly, the goal for new groups and activities set up by Live Well is to become independent and sustained within and by their local community on a voluntary basis.
People who receive support from Live Well, and those who attend Live Well groups are often keen to continue their involvement as a volunteer but their role is limited if there is no process for them to gain DBS clearance and relevant training.
Once again, this situation was communicated to the coproduction group who shared their experience of managing similar challenges and offered their support in various ways. It was agreed that funding from the project would be provided to Rushcliffe Council of Voluntary Services to train and employ volunteers to work on Live Well initiatives.
A small working group was set up to develop appropriate recruitment procedures, training and ongoing supervision of volunteers. Rather than preparing volunteers for one specific role within Live Well, a Rushcliffe wide system was developed so that once recruited, checked and trained, volunteers are able to work with individuals as befrienders, or supporting groups and activities.
The first cohort of volunteer trainees included 22 ex-Live Well clients who wanted to ‘give something back’ and continue their involvement with the project.
Box 8. The core principles of peer support24
- Mutuality – The experience of peers who give and gain support is never identical. However, peer workers in mental health settings share some of the experiences of the people they work with. They have an understanding of common mental health challenges, the meaning of being defined as a ‘mental patient’ in our society and the confusion, loneliness, fear and hopelessness that can ensue.
- Reciprocity – Traditional relationships between mental health professionals and the people they support are founded on the assumption of an expert (professional) and a non-expert (patient/client). Peer relationships involve no claims to such special expertise, but a sharing and exploration of different world views and the generation of solutions together.
- Non-directive – Because of their claims to special knowledge, mental health professionals often prescribe the ‘best’ course of action for those whom they serve. Peer support is not about introducing another set of experts to offer prescriptions based on their experience, e.g. “You should try this because it worked for me”. Instead, they help people to recognise their own resources and seek their own solutions. “Peer support is about being an expert in not being an expert and that takes a lot of expertise.” (Recovery Innovations training materials. For details see www. recoveryinnovations.org)
- Recovery-Focused – Peer support engages in recovery focused relationships by: inspiring HOPE: they are in a position to say ‘I know you can do it’ and to help generate personal belief, energy and commitment with the person they are supporting; supporting people to take back CONTROL of their personal challenges and define their own destiny; facilitating access to OPPORTUNITIES that the person values, enabling them to participate in roles, relationships and activities in the communities of their choice.
- Strengths-based – Peer support involves a relationship where the person providing support is not afraid of being with someone in their distress. But it is also about seeing within that distress the seeds of possibility and creating a fertile ground for those seeds to grow. It explores what a person has gained from their experience, seeks out their qualities and assets, identifies hidden achievements and celebrates what may seem like the smallest steps forward.
- Inclusive – Being a ‘peer’ is not just about having experienced mental health challenges, it is also about understanding the meaning of such experiences within the communities of which the person is a part. This can be critical among those who feel marginalised and misunderstood by traditional services. Someone who knows the language, values and nuances of those communities obviously has a better understanding of the resources and the possibilities. This equips them to be more effective in helping others become a valued member of their community.
- Progressive – Peer support is not a static friendship, but progressive mutual support in a shared journey of discovery. The peer is not just a ‘buddy’, but a travelling companion, with both travellers learning new skills, developing new resources and reframing challenges as opportunities for finding new solutions.
- Safe – Supportive peer relationships involve the negotiation of what emotional safety means to both parties. This can be achieved by discovering what makes each other feel unsafe, sharing rules of confidentiality, demonstrating compassion, authenticity and a non-judgemental attitude and acknowledging that neither has all the answers.
Box 9. Overview of training provided for Health Coaches and Link Workers
A 10-day training programme.
Most of the training was developed and delivered by the ImROC project team and includes some content from established recovery and peer support training programmes delivered by ImROC. Some was delivered by local and national experts.
A broad outline is included below:
Day 1 – Understanding personal care and support planning – delivered by NHSE
Day 2 – Getting underpinning principles of LLWiR: “lets be…”, project and roles, recovery principles, co production, exploring, negotiating working within our values and principles
Day 3 – Health coaching and using the PAM – delivered by NHSE
Day 4 – Essential Skills: Active Listening and Problem Solving, developing part one Green Book
Day 5 – Goal setting, goal attainment scaling and 5 ways to wellbeing, part two Green Book
Day 6 – Using lived and life experience safely, appropriately and effectively, lone working policy
Day 7 – Supervision and personal development, supervising staff / volunteers, developing a recovery focussed supervision protocol , developing your life passion at individual, practice and community level
Day 8 – LLWiR evaluation – what this means in practice – delivered by Clifford Stevens and team NTU
Day 9 – Co production reviewing content of Green Book, community development ABCD
Day 10 – Health Coaching part two – NHSE
Ongoing Training and Development
The team meets for one day every month to focus on shared issues that need further consideration. Thus, meetings include a catch up – sharing progress, achievements, challenges and questions, then goes on to provide training on a particular subject, often with an external trainer, for example:
- Supporting someone in crisis
- Problem-solving and setting personal goals
- Understanding the contribution of various community organisations and services
- Setting up a community group ….
In addition all members have monthly personal supervision, and can access support from the project manager or their health coach whenever they feel they need it.
Figure 2. Let’s Live Well in Rushcliffe at a Glance
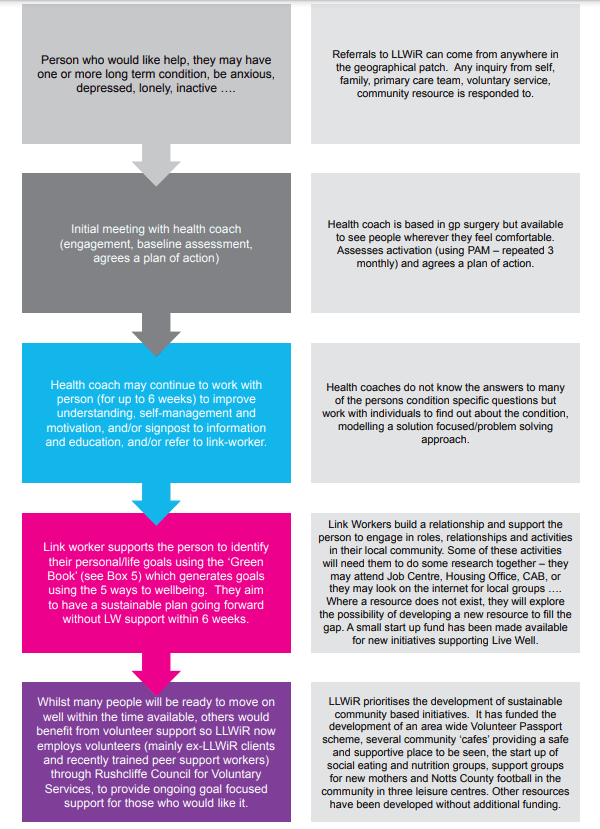
5. Evaluating LLWiR
Evaluation of Let’s Live Well in Rushcliffe (for full report see Dr Moon Halder, Elizabeth Mair, Dr Juliet Wakefield, Dr Blerina Kellezi, Dr Niamh McNamara, Dr Mhairi Bowe, Dr Iain Wilson & Dr Clifford Stevenson (March 2019) Evaluation of the Let’s Live Well in Rushcliffe Initiative: Final Report FULL REPORT WITH TECHNICAL APPENDICES, Department of Psychology, Nottingham Trent University)
A full evaluation of the project was undertaken by Nottingham Trent university to assess impact on health and service use. This study reported significant improvements in patients’ physical and mental wellbeing after the initial four month period which were maintained after eight months. There was also an increase in community group membership at 4 months which reduced slightly by 8 months. There was a decrease in both primary and secondary care usage over the evaluation period. The economic evaluation of the programme attached savings to the improvements in health as well as the changes in health and social care usage. Projected over a year post-baseline assessment, this estimates a ROI of £1.00. In other words, if the patient benefits recorded for the first four months are continued for the rest of the year, the programme will recoup 100% of its costs by January 2020.
The Nottingham Trent University (NTU) evaluation set out to capture the degree to which the LLWiR pathway impacts upon the health and service use of its beneficiaries. Accordingly, it involved three studies: a patient survey study to establish the extent of the effects, a survey of GP and practice nurse perceptions and experiences of the pathway and an interview study with clients, providers and third sector organisations to understand how it works. Of the 1483 referrals received in the first 13 months of service provision, 1176 had received support by the end of February 2019 and 655 had agreed to participate in the evaluation and 630 provided usable responses at baseline. 178 at a four month follow-up and 63 at a final eight month follow-up.
There were significant improvements in patients’ physical and mental wellbeing after the initial four month period which were maintained after eight months. There was also an increase in community group membership at 4 months which remained stable after 8 months. There was a decrease in primary and secondary care usage over the evaluation period.
The economic evaluation of the programme attached savings to the improvements in health as well as the changes in health and social care usage. Projected over a year post-baseline assessment, this estimates a ROI of £1.00. In other words, if the patient benefits recorded for the first four months after initial assessment are continued for the rest of the year, the programme will recoup 100% of its costs by January 2020. This compares favourably with many other comparable programmes in this area.
Interviews with 7 GPs, 3 HCs, and 6 LWs indicated that they recognise both the increasing importance of addressing social factors in patient care and the need for person-centred care in addressing holistic needs. Their experiences of referring or delivering treatment on the pathway point to the importance of improving social connectedness among patients in the improvement of their health and wellbeing, even for those with a focus on specific health concerns. These findings were supported by the GP/practice nurse survey, which found substantial support for the programme and positive experiences of its performance.
Interviews with 19 beneficiaries evidence a range of physical and social benefits which patients had gained from their experience of engaging in the LLWiR programme. Of particular importance to patients were their relationships with LLWiR staff and their ability to connect effectively with activity groups, both of which contributed towards their confidence in meeting their set goals.
Interviews with 8 members of the co-production group, 8 group leads, and 3 volunteers pointed to the good work done by LLWiR in establishing supportive relationships across the voluntary sector, in setting up new groups to meet patients’ needs, and in drawing upon the skills of those with lived experience to develop the programme and support patients. Co-production members and group leads also highlighted the need to stimulate and maintain community engagement with groups whilst supporting their sustainability.
Key challenges for the programme include refining and promoting a clear message as to the purpose and focus of the pathway. Some GPs confessed to having only a basic grasp of the content of the pathway and lack of programme clarity was reported as the main reason for failing to refer to the programme. Lack of fit between expectations and service delivery was a key reason for negative experiences among beneficiaries, who occasionally reported that their groups were unfamiliar with their needs as LLWiR patients.
The evidence base for Recovery offers achievable answers to the resource restrictions and system pressures that mental health providers, commissioners and others in the system are facing on a daily basis. Co-authored by Institute of Mental Health, London School of Economics and ImROC, Recovery: the business case is an outcome analysis and economic review of Recovery. This is a Call to Action for leaders in service provision, policy and influential parties to take a ‘leap of faith’ into a new way of supporting Recovery with the firm foundation of evidence beneath them. Coproduction at every level of system design and service delivery; a workforce employed specifically for their skills and expertise of their lived experience valued equally to other roles within the workforce; recovery education and greater self management are essential elements of the future of supporting recovery.
The concept of ‘recovery’ has become a dominant theme in mental health system policy internationally in the 21st century. Thus, the World Health Organization Mental Health Action Plan 2013-2020 identifies the need for ‘a recovery-based approach that puts the emphasis on supporting individuals with mental disorders and psychosocial disabilities to achieve their own aspirations and goals.’ The challenge for mental health services in each country is therefore not ‘whether to support recovery?’, but ‘how?’ Yet sustained reductions in public spending intended to reduce the government budget deficit and the welfare state in the United Kingdom have created austerity policies that have severely impacted outcomes for people living with serious and long term mental health conditions and those supporting them.
This important new paper from ImROC analyses a broad range of evidence to evaluate the health and social care impact and economic argument for supporting people to live the lives they want to lead. Structured around the ImROC 10 key organisational challenges, the paper covers every aspect of an organisation, system and community and provides practical solutions, innovations and strategic overview to enhance and support Recovery.
“Whilst the challenge – and importance – of supporting people with mental health conditions to recovery full, meaningful and contributing lives has long been recognised, there has been widespread doubt and scepticism about the most effective ways of doing achieving this. Recovery: the Business Case rigorously demonstrates the effectiveness and efficiency of interventions and approaches that really do support people with mental health conditions in their Recovery. It absolutely validates the ImROC ten challenges as a framework for organisations to improve their recovery orientation, and perhaps most critical in this time of financial austerity, it is clear that by supporting people to achieve their own Recovery we reduce their need for lengthy, unplanned and crisis led admissions. We now have the evidence that Recovery focused services are ethical, effective and efficient”. Dr Julie Repper, ImROC Director
“This report bring together recovery-related evidence from scientific research, personal experience and economic evaluations. It will be helpful in making the case for why it is in the interests of all of us – including people who use mental health services, their families, workers, managers and commissioners – to develop a focus on recovery. There are of course other reasons to support recovery: people who use services want their recovery supported, and a recovery orientation is national policy. But alongside these reasons, there is now a compelling business case for many of the ImROC key organisational challenges.” Mike Slade, Professor of Mental Health Recovery and Social Inclusion, University of Nottingham and lead author.
14. Recovery: the Business case
Mike Slade, David McDaid, Geoff Shepherd, Sue Williams and Julie Repper
Executive summary
This paper makes the Business Case for supporting recovery. We believe that this should be informed by three types of data: evaluative research (such as randomised controlled trials); the perceived benefits for service users – what might be termed ‘customer satisfaction’; and best evidence about value for money.
Some of the ImROC 10 key challenges have a very strong research base. For example, there is substantially more randomised controlled trial evidence supporting the value of peer support workers (challenge 8) than exists for any other mental health professional group, or service model.
Similarly, the scientific evidence for supporting self-management (challenge 1) is compelling. Other challenges have a strong evidence base indicating that they improve people’s experience of services. The positive experiences of students at Recovery Colleges (challenge 3) and the beneficial impact on experience of more involvement in safety planning (challenge 6) are clear.
Finally, the economic evidence is strong for some challenges. There is for example an established financial benefit from workplace mental health programmes (challenge 9), and a very strong value-for-money argument supporting the importance of access to decent housing, education and employment opportunities (challenge 10).
Of course, the Business Case is only one reason services should be attempting to support recovery. Some people would argue that it is a ‘rights’ issue. Those who use services simply deserve – by right – to be provided with the services that they appear to find most helpful. A third reason is political – mental health policy in many countries including the UK is clear that tax-payer funded services should focus on supporting recovery. A fourth reason is the pressure on Trusts to meet efficiency savings; a clear focus on supporting recovery can inform evidencebased resource allocation decisions. A final reason stems from the impact of political and economic pressures on the work of managers and practitioners in mental health. In countries throughout the developed world the demand for mental health services far exceeds the political will to dedicate adequate resources to it. This means that we may all have to think again about the nature of mental health services themselves – what should their priorities be? And, how should they be provided? Supporting recovery has some of the answers to these difficult questions. We believe there is now sufficient evidence to justify a focus on recovery as the ‘core business’ of the mental health and social care system.
1 Professor of Mental Health Recovery and Social Inclusion, School of Health Sciences, Institute of Mental Health, University of Nottingham
2 Associate Professorial Research Fellow, Personal Social Services Research Unit, London School of Economics and Political Science
3 Senior Consultant, ImROC
4 Senior Peer Trainer, CNWL Recovery and Wellbeing College
5 Director, ImROC
Introduction
This Briefing Paper presents the business case for offering recovery-focused services in health, social care, housing and other relevant sectors. It builds on existing work on investing in recovery which attempted to review some of the economic and social benefits of enabling people to achieve their own life goals, supporting them to manage their own condition, get a job, make friends, and maintain safe and secure housing of their choice1. The paper is aimed at senior managers, chief executives and commissioners in health and social care and other related sectors, policy makers, clinicians, people who use services, their families and carers. In this Briefing Paper we use ‘mental health services’ as a shorthand for the full range of services across all sectors which support people’s recovery.
The concept of ‘recovery’ has become a dominant theme in mental health system policy internationally in the 21st century2. Thus, the World Health Organization Mental Health Action Plan 2013-2020 identifies the need for ‘a recovery-based approach that puts the emphasis on supporting individuals with mental disorders and psychosocial disabilities to achieve their own aspirations and goals’3. The challenge for mental health services in each country is therefore not ‘whether to support recovery?’, but ‘how?’.
To do this, we must be clear what we are talking about when we use the word ‘recovery’. It is still a contested term and there remains considerable variation in how it is used by different commentators. In the ImROC programme we have consistently used it to describe the efforts of people with mental health problems to live meaningful and satisfying lives4. This is often referred to as ‘Personal Recovery’ to distinguish it from a process of symptom reduction (‘Clinical Recovery’)5. ImROC has also leant heavily on the early work by Repper and Perkins which highlighted the importance of ‘hope’, ‘control’ and ‘opportunity’ as key processes underlying these individual journeys6. Hope Control Opportunity.
These ideas have been confirmed in a systematic review of the literature which added two other key processes: ‘connectedness’ and ‘meaning’. This produces the ‘CHIME Framework’ 7 which consists of Connectedness (social support/ integration), Hope (optimism for the future), Identity (beyond that of a ‘patient’), having Meaning (in one’s life), and the importance of Empowerment (achieving some control over one’s mental state and adjustment). CHIME Connectedness Hope Identity Meaning Empowerment This framework has been widely used to identify the processes of personal recovery which need to be supported in mental health services.
Overall, recovery is consistent with an emerging new paradigm about the delivery of services, which places far greater emphasis on people’s strengths and possibilities than on their problems and deficits.
Supporting recovery therefore involves working differently. An international analysis of best practice in recovery support identified the need for transformation at four different levels8, shown in Box 1.
“The challenge for mental health services in each country is therefore not ‘whether to support recovery?’, but ‘how?’.”
“CHIME: Connectedness Hope Identity Meaning Empowerment”
Box 1: Best practice in supporting recovery
- Supporting recovery – providing treatments and other supports as a resource for the person to use in their recovery journey, rather than doing things to the person
- Working relationships – ‘how’ you work with the person matters, i.e. the relationship is more than the vehicle to provide treatment, it is the ‘treatment’ – which has implications for e.g. relationships in a care co-ordination context
- Organisational commitment – the culture within services directly impacts on how our services work, e.g. a disempowering management culture creates a disempowering (and disempowered) work-force.
- Promoting citizenship – recovery happens in ‘real life’, as individuals find a safe home to live in, make friends, engage in meaningful occupation, etc. – these are the things we all need for wellbeing.
So, supporting recovery involves using clinical expertise as a resource, engaging with people as partners in care, not simply recipients, ensuring top-to-bottom alignment with recovery values in our organisations, and focussing efforts beyond health and social care systems to create pathways to citizenship. The ImROC programme identified ‘10 Key Organisational Challenges’ to support these levels of transformation9, shown in Box 2.
Box 2: 10 key organisational challenges as published in 2010
- Changing the nature of day-to-day interactions and the quality of experience
- Delivering comprehensive, user-led education and training programmes
- Establishing a ‘Recovery Education Unit’ to drive the programmes forward
- Ensuring organisational commitment, creating the ‘culture’. The importance of leadership
- Increasing ‘personalisation’ and choice
- Changing the way we approach risk assessment and management
- Redefining user involvement
- Transforming the workforce
- Supporting staff in their recovery journey
- Increasing opportunities for building a life ‘beyond illness’
“Hope Control Opportunity”
Some of these key challenges have been updated in the light of experience, as will be discussed later. We also note that the journey of understanding about recovery is not finished, and anticipate the need to focus more in the future on for example experiences of family10, physical health (drawing on studies such as SHINE11 and IMPARTS12), ethnicity13 and community partnerships.
In this paper, these 10 key challenges are used to organise the information for the business case. For each organisational challenge, three important types of evidence of effectiveness will be summarised:
- evaluative evidence from formal research studies. We now have credible scientific evidence for a number of effective approaches to supporting recovery, which we will describe later in this document.
- evidence from narrative accounts and experience of individuals regarding the impact of these ‘recovery-supporting services’ on them, their families and on workers in the services (organisational/ cultural changes). People using services have also talked about the transformative potential of recovery: Being supported in my recovery, rather than just having my symptoms of mental illness treated, meant that I got my life back, albeit a different one… I’d ended up with no hope, believing I was ‘untreatable’ and inadequate, but now I am back in the ‘driving seat’ of my life. I have friends, a job and an active role in my community because I was lucky enough to come into contact with people who could see the person behind the label and focus on me and my life, rather than just my symptoms.
- economic evidence where available on the cost and efficiency of these new services. We will argue that investing in effective actions to support recovery also makes economic sense; something that is vital when health and other public services are under enormous pressure. Recovery is associated with a lower need to make use of specialist health services, increased participation in paid and voluntary work, as well as in social activities, more stable accommodation, and positive impacts for family units.
These three forms of evidence (research, personal experience and economic) constitute the Business Case justifying a move towards more recovery-oriented services. This paper, like all ImROC Briefing Papers, is co-written between people with a range of professional and lived experience.
“Recovery is consistent with an emerging new paradigm about the delivery of services”
Key organisational challenge 1: Changing the nature of day-to-day interactions and the quality of experience
Key concepts: Narratives; Strengths-based; Coaching; Shared decision-making; Self-management; Joint crisis planning; Open Dialogue
Research studies
The first challenge – and the most fundamental one – is to change the nature of day-to-day interactions between staff and people who use mental health services so that they are continually perceived to be supporting personal recovery and improving the quality of care experienced. This is an ambitious aim, but it must be the ultimate objective of all the organisational changes to be discussed later. It is also needed –only 31% of people nationally report having a very good experience of care based on their contact with mental health services14.
Supporting personal recovery, whether inside or outside formal mental health services, is dependent on access to trusted and enduring relationships – what have been called recovery promoting relationships15. They are based on establishing shared values, demonstrating empathy, warmth, and respect for the individual, combined with a willingness to go the ‘extra mile’16. These qualities form the bedrock for all forms of mental health care17 and the evidence for the importance and effectiveness of these relationship skills is now well-established18 19. All professions make some effort to include them in their basic training, but the extent to which they are central to accreditation varies across professional groups.
There is also now evidence regarding unhelpful characteristics of staff working with people with severe mental health problems. A systematic review of the literature concluded that conversations which are pessimistic, uncaring, paternalistic or disrespectful hindered the development of helpful relationships and contributed to instilling hopelessness and inhibiting personal growth20. These detrimental effects were particularly damaging in the context of services characterised by discontinuity, coercion or insufficient time.
However, there are approaches which reflect recovery-supporting values, involve prorecovery working practices and have an emerging evidence base. These include:
Use of narrative accounts
In terms of recovery-oriented practices, the best starting point is listening to the persons own account of what has happened to them. Everyone has a story to tell and the process of telling your own version of your story in your own words is almost always experienced as positive and validating. Such narratives help people to make sense of their experiences, they provide a basis for formulating personal goals and monitoring progress. They also provide a source of information and explanation which is complementary to a conventional, ‘evidence-based medicine’ approach21. Approaches like Photovoice22 are emerging as ways of enabling people to find ways of presenting their own perspectives, experiences and feelings using different media.
“It [inpatient care] was a frightening and bewildering time for me. I felt completely lost and did not know what was happening to me or what the future might hold…(then) I met a nurse who proved, literally, to be my life-saver…She was a great inspiration. She told me that I would not always be in this state, although a lot of that would be up to me. With her support, I started to learn about myself…This wonderful woman gave me the strength to carry on, and not end my life as I had planned.”
Service user
“My experience of using services was mainly that the focus was always on what was wrong with me….. I was always on the receiving end of other people’s decisions about me, and I was not asked for my opinion. This just increased my own feelings of having nothing of any value to anyone…then one time my care co-ordinator asked what I thought about a decision … I remember feeling really surprised that he was asking me, but it actually started me thinking for the first time in a long time, about my own situation and what I could do about it.”
Service user
Building on strengths
A second important practice is the consistent use of a ‘strengths’ approach23. This seeks to identify the person’s qualities, assets and competencies and their environmental resources (friends, neighbours, local opportunities) which might be used firstly as a basis for relationship building, secondly to confirm their personal value and achievements which they often struggle to identify, and thirdly as the foundations for building up skills and strategies to further their personal life goals24. A review of strengthsbased interventions for people with severe mental illness identified benefits in relation to hospitalisation rates, employment/educational attainment, and intrapersonal outcomes such as self-efficacy and sense of hope23.
Coaching
Another recovery-supporting practice, which has been developed in the last few years, is the ‘coaching’ model25. This uses many of the same techniques as the strengths approach, e.g. an emphasis on the service user taking the lead, the importance of identifying personally-relevant goals26, and a focus on strengths and natural supports. However, there is greater emphasis on the importance of staff behaviour as a ‘coach’, or learning partner (‘on tap, not on top’) and on the service user’s responsibilities to make a commitment to action. There is now emerging evidence for the effectiveness of coaching in relation to supporting recovery, both in27 and beyond28 the mental health system.
Shared decision-making
Systematic review evidence indicates that collaborative relationships which help individuals increase their sense of control over their lives are the best approach to supporting hope29. This can be achieved by establishing a greater focus on shared decision-making30, particularly in relation to medication management31. NICE Guidelines state that shared decision-making should be used with all people using mental health services (Quality Statement 3), including specifically those detained under the Mental Health Act (Quality Statement 11)32.
Joint crisis planning
This is an important application of shared decision-making in the context of discharge planning following inpatient admissions. The ‘Joint Crisis Plan’ (JCP) is formulated by the service user, together with peer support if available, and the key mental health staff involved in their care, including the treating psychiatrist. In an initial randomised controlled trial, people who were discharged with a JCP were shown to have significantly fewer compulsory admissions compared with controls over a 15 month follow-up period33. Qualitative data also suggested that the JCP group felt more ‘in control’ of their mental health problems34. A second study produced less impressive results, due to practical difficulties in ensuring that the joint planning meetings always occurred and were effectively facilitated35. Implementation of JCPs also depends on successfully engaging clinicians and overcoming their prejudices regarding the validity of service users’ views and the feasibility of meeting them36.
“The challenge for modern, recovery-oriented, mental health services is not just doing more of the same thing”
Self-management
Closely allied to shared-decision-making is the support of ‘self-management’. A comprehensive review of the evidence by the Health Foundation (550 systematic reviews, randomised controlled trials and large observational studies) concluded that “the totality of evidence suggests that supporting self-management can have benefits for people’s attitudes and behaviours, quality of life, clinical symptoms and use of healthcare resources” (p. v)37. The review found robust evidence that effective self-management support leads to higher self-efficacy and subjective well-being. Lower-quality evidence linked more effective self-management with improved clinical outcomes and the potential to reduce visits to health services by as much 80%. Specifically, in relation to mental health, peer-led self-management programmes improve primary care contact and physical health-related quality of life38. Approaches which include the full and active involvement of the person, rather than simply the passive provision of information, are most likely to be effective. Thus, the Health Foundation recommends, “a fundamental transformation of the patient-caregiver relationship into a collaborative partnership” (p.vi).
“I have noticed a gradual shift in the way the [memory service] team relate to people living with dementia since the peer support workers have been in post. They focus more on the existing skills and strengths of each person and how these can be built upon”
Project lead
Open Dialogue
A final approach which brings together a number of recovery- supporting practices is ‘Open Dialogue’39. This was developed in a small rural community in western Lapland, but is now beginning to attract international attention. It places the service user and their immediate carers at the centre of a shared decision-making process and assumes that their key role is to listen and try to make sense together of the personal meaning of psychosis. Implementation of the approach is based on rigorous training and implies significant organisational change but much is currently being claimed for its effectiveness in helping people achieve long-term valued outcomes, particularly in relation to reducing dependence on medications. At the moment, the evaluative research requires replication in larger, more heterogeneous and urban populations.
To summarise, the challenge for modern, recovery-oriented, mental health services is not just doing more of the same thing – more staff, greater professional expertise, more ‘evidence-based’ treatments, etc. We need to change the fundamental characteristics of the interactions between those tasked with delivering the services and those receiving them. We need to provide high quality, basic human relationships which develop trust, based on a respect for individuality and personal experiences of developing resilience in managing their experiences (of ‘illness’). This will involve developing services which build on people’s strengths and resources to help them use professional expertise to move towards personally valued social goals (housing, integration, employment), not simply the reduction of symptoms.
Economic evidence
If better long term social functioning is achieved as a result of reshaping the nature of the relationship between staff and people who use mental health services then positive economic outcomes will be achieved. For instance we know that participation in employment is both empowering, associated with better health (and thus lower need for health care services) and reduces the need for social welfare benefit support. Specific economic evidence on the different approaches that we have described are however limited.
Evidence on the economic benefits of shared decision making (for any health condition) is mixed, but studies appear to focus solely on short term outcomes rather than longer term benefits of better social functioning40. Separately there is also a literature on the value of peer support for decision making which is discussed later. Studies on shared decision making suggest that despite initial increase in staff contact time required for collaborative discussions, there are positive long term impacts on health service use. For instance several studies show that health coaching (particularly telephone coaching) for long term conditions can be cost effective. Analysis in the US of almost 10,000 people who received health coaching for conditions including depression and schizophrenia revealed consistent cost savings due to lower inpatient and outpatient contacts41. There is also some evidence in England that investing in coaching in community mental health teams, can be done without any immediate (one-year) significant impact on costs to the health system27. A German study looking at telephone coaching for different patient groups including people with mental health needs also did not identify any significant impact on health outcomes or costs42. Another small English case study which looked at costs and benefits of providing training in health coaching for a wide range of health conditions, reported substantial cost savings due to reduced time needed to treat people which would more than cover the costs of training. It did however acknowledge the need for large scale quantitative evaluation of coaching to formally determine costs and benefits43.
The economic evidence on approaches to self-management tends to focus on physical rather than mental health needs44 45. This often suggests actions are cost effective. However little is known specifically about the economic case for self management in people with chronic mental health problems such as depression or anxiety disorders, although some economic analysis is underway46.
There is evidence on the economic case for the joint crisis planning trials that we have discussed. The first of these studies found that there was almost an 80% probability of crisis planning being at least cost effective and often cost saving per additional 1% of hospital admissions averted compared to a standard information service, when taking into account use of health, social care and criminal justice system services over the subsequent 15 months47. The second study reported a similar likelihood of being cost effective from a health system perspective; in addition crisis planning had a 44% chance of being cost saving, although there was no significant difference in costs compared to routine support, when the broader impacts of criminal activity and time out of employment were taken into account48. A trial of joint crisis planning in the Netherlands found that it reduced future compulsory hospital admissions over the following 18 months, but there were no other significant impacts on health service use49.
Key organisational challenge 2: Delivering comprehensive, co-produced learning opportunities
This key challenge has been updated in the light of experience.
Key organisational challenge 2: Coproduced Recovery focused learning and development opportunities are available for all staff working in services
Key concepts: Adult education; Self-directed learning; Problem-centred learning
Research studies
Adult learning is inextricably intertwined with recovery50. In general terms, adult learning in younger adults has been empirically shown to be an effective approach to reducing health inequalities51-53. There is also evidence from across the age range that participating in learning events can have positive effects on life satisfaction, health and wellbeing54 55. For mental health service users, adult learning can also enhance resilience and help build social capital56; it can also reduce symptomatology and enhance wellbeing57. Overall, adult learning is therefore likely to impact beneficially on health and well-being and may increase community participation58.
Specifically in relation to supporting recovery, adult learning is at the heart of developments like Recovery Colleges (key challenge 3) and peer support (key challenge 8) and it is through staff learning that changes in attitudes occur – especially among those in senior positions – and these lead to changes in organisational culture (key challenges 4 and 9). However, how these educational processes are organised is critically important.
Learning is not the same as being taught. Both teaching and learning are important. Some individuals prefer one method to another and some topics lend themselves more easily to one approach over the other. Nevertheless, ‘perhaps the most critical shift in education in the past 20 years has been a move away from a conception of “learner as sponge” toward an image of “learner as active constructor of meaning” ’59. The key differences between ‘teaching’ and ‘learning’ (adapted from Wilson and Peterson59) are summarised in Box 3.
“Achieving authenticity and integrity…that’s the challenge! I think genuine transformational leadership can be achieved by creating increased opportunities for dialogue between service users, carers and practitioners which is unfettered by the institutional restraints of the organisation. This is not “a quick fix” but a complex, slow process which requires a lot of hard work. If this process is endorsed corporately, it enables an on-going conversation at all levels of the organisation which facilitates the development of common values, aims and more open, genuine co-productive relationships between all the participants.”
Recovery Programme Lead
“I think a recovery focused leader needs all the usual qualities of transformational leadership but they also need to really ‘get recovery’ and to be able to communicate it in a way that inspires others. They don’t give up and they keep going even when the odds are stacked against them. They are prepared to take a leap of faith and although they know the direction of travel, they don’t think they have all the answers.”
Clinical Director
Box 3: Difference between teaching and learning
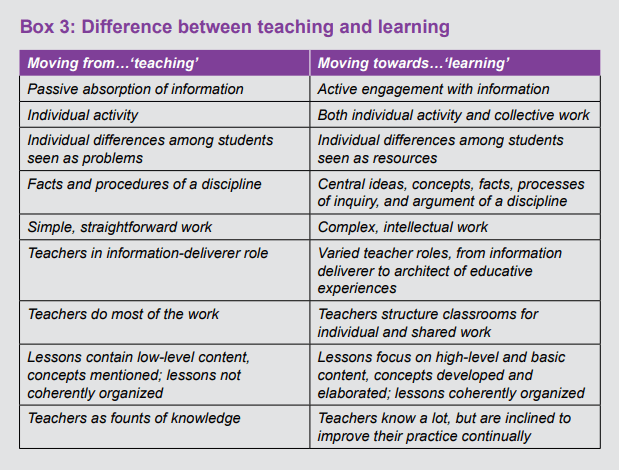
An approach to learning that ImROC uses with whole teams (including staff from all professions and people using the service) is the Team Recovery Implementation Planning Process (TRIP)60. This process is a collaborative learning experience founded on co-production, in which the service becomes a catalyst for change rather than a creator of change by (a) enabling people to lead their own recovery and (b) supporting the development of recovery-oriented services and empowering people to develop resources in peer networks and communities. Early evaluation of the impact of TRIP is promising61.
To summarise, changing staff (and thus organisations) to become more supportive of recovery involves using modern educational ideas which assume that people come to training with an active interest in learning, but also with their own pre-existing beliefs. Learning is about providing opportunities where these beliefs can be made explicit and can be discussed and, if appropriate, challenged. This is often best done in a group setting where everyone – not just the teacher – is encouraged to contribute. Approaches such as Schwartz Rounds62 and engaging leadership63 address the dynamic, relational and distributed nature of leadership.
“In order for staff to be able to work effectively within the recovery approach, they must feel empowered by their managers. Giving recovery targets or instructions to deliver recovery just won’t work. Recovery focused leadership looks for the strengths of individual staff members and teams and brings them out, by giving support and encouragement. This does not mean that managers overlook problems or ignore bad practice, but looking for problems is not their starting point.”
Service Director
Economic evidence
It is important to assess the economic impacts on staff of co-produced learning and development opportunities, as well as understand whether there are any financial and/or organisational barriers to participation in such learning opportunities. However much of the existing literature on co-production does not appear to devote much attention to outcomes and impacts on staff, other than changes in attitudes, as seen in the REFOCUS study. Improved understanding and insights for staff as a result of this type of learning, may be beneficial in terms of their own mental and physical health and perhaps also in terms of staff turnover – something that has been seen with the implementation of co-produced approaches to safety planning that are discussed in key challenge 6. This however needs to be assessed in future studies that look more at the impacts on the workforce and not just at changes in attitudes or knowledge.
Key organisational challenge 3: Establishing a ‘Recovery Education Unit’ to drive the programmes forward
This key challenge has been updated in the light of experience.
Key organisational challenge 3: Coproduced, Recovery focused learning opportunities are available for everyone using the service where people with mental health conditions, the staff and families who support them and others in local communities can share expertise and learn together
Key concepts: Recovery Colleges, Educational Approach, Co-production, Adult learning
“The recovery and social inclusion course felt amazing for me .… I have owned and worn a coat of stigma for most of my life. It was made to measure. Nowadays though, whenever I feel its weight upon my shoulders, I take it off and hang it on the nearest hook. It has become outworn, unnecessary and for the first time in my life, I feel confident enough to say that my own business with it is finished.”
Coming to the college was an important first step in regaining confidence and motivation to do more with my life.”
Research studies
Recovery Colleges are one of the key developments for promoting co-produced learning64 and are probably the most visible change in mental health services which are attempting to engage with the recovery agenda. Currently there are nearly 70 Recovery Colleges in England65 and they are being developed in several different European countries, and in Australia, Japan and Hong Kong66. The theoretical foundations for Recovery Colleges include: shared decision-making and self-management (key challenge 1), adult learning (key challenge 2), coproduction (key challenge 7) and community participation (key challenge 10). They therefore embody a number of the central principles for supporting recovery. However, while the theoretical foundations are strong, the empirical evaluations are still weak.
Overall the available empirical evidence is consistently positive. Recovery Colleges are popular with service users, they engage people who often find traditional day services unattractive and attendance rates are consistently high65. There is also some evidence that they are associated with improved outcomes, both subjectively (higher hopefulness, more goal-directed behaviour) and reduced use of community mental health services, particularly among those who attend at the majority of scheduled sessions. Care co-ordinators with clients who attend RCs are also more likely to value and support selfmanagement67.
“The ‘telling your story’ course gave me a different perspective on what I was feeling. I realised I still had some work to do, but was helped to see how to do it. Meeting other people who told their stories in different ways helped too.”
There is also evidence of benefits for the organisation as a whole in terms of improved staff expectations and attitudes68. There is patchy evidence that they can help with restarting education, voluntary work or employment69 with one study finding 70% of students going on to be mainstream students or to paid or volunteer work70. This led an independent think-tank report to state that Recovery Colleges have ‘significant potential for impact on improving employment outcomes’71.
However, the methodologies used to investigate these outcomes consist primarily of single case, prospective, follow-up studies using cross-sectional interviews or observational approaches72 73 69 74 75. There is little agreement on standardised outcome measures76. There is also a need to conduct further research to clarify the key elements of the ‘independent variable’ (i.e. attendance at the college). At the moment it is not known exactly what characteristics are critical77. These issues are being addressed in a NIHRfunded study called RECOLLECT (www.researchintorecovery.com/recollect).
“I have found the course to be a source of inspiration – I feel it breathed new life into my practise. It gave me a new approach to my patients, not seeing his/ her problems, but their strength”
“It was helpful hearing people describe problems similar to those of my son.”
“Recovery Colleges are one of the key developments for promoting co-produced learning”
Economic evidence
There is positive albeit limited evidence on the economic impact of recovery colleges. In England in-house evaluations of recovery colleges do suggest that there is a justified business case. The most methodologically robust evaluation compared the use of mental health services by students in the 18 months prior to and post enrolment in a recovery college. Overall there was a reduction in inpatient stays, admissions under the Mental Health Act and in community contacts while mental health outcomes also improved. Reductions were greater for students who completed a course compared with a retrospectively identified population that did not. It was estimated that overall there was a significant reduction in NHS Trust resource demands of £1,200 per student per year, even after taking into account the additional costs of delivering the Recovery College78. Costs averted increased to £1,760 for students who successfully completed a course.
An in-house evaluation of another Recovery College also identified a significant reduction in the use of health services by students (costs averted of more than £845 per year for those the completed a course) twelve months after attending courses79, but students may have not have been comparable to those who did not use the college78. Overall, the evidence is encouraging, and potentially conservative. Some of the other benefits of using Recovery Colleges that may be realised, such as more confidence in seeking employment, will likely make the economic case more powerful. They also need to take account of the value of volunteer / co produced time and discretionary unpaid additional inputs from staff80. Going forward it will be important to compare investment in Recovery Colleges with appropriate alternative options to support recovery, using methods including controlled trials.
Key organisational challenge 4: Ensuring organisational commitment, creating the ‘culture’. The importance of leadership at every level
This key challenge has been updated in the light of experience.
Key organisational challenge 4: Recovery focused leadership at every level and a culture of Recovery
Key concepts: Organisational commitment; Recovery as a priority; Empowering management; REFOCUS; Illness Management and Recovery (IMR); Team Recovery Implementation Plan (TRIP)
“We must think beyond simply ‘training’ staff to behave in different ways.”
Research studies
Helping mental health services better support recovery means addressing some of the organisational changes necessary to establish a unique and distinctive culture. Of course, the quality of support for individuals will ultimately depend on the quality of care provided by individual staff in their everyday interactions (key challenge 1) but, in order for this to happen consistently across the organisation, we must think beyond simply ‘training’ staff to behave in different ways. This is illustrated in a study examining the implementation of ‘Illness Management and Recovery Programmes’ across 12 community settings in the USA81. Training was found to be important, but it only had a lasting effect if issues of supervision and leadership were also addressed. A ‘culture of innovation’ was also found to be important, i.e. organisations being open to considering changes in existing practices. This aspect of organisational readiness has also been found important in England82. If all these factors were present then they acted synergistically, but no one element was sufficient on its own. So, how can we ensure that the shared values of recovery permeate the whole culture of the organisation and are reinforced by leaders at all levels?
This is particularly difficult at a time when there are ‘unclear goals, overlapping priorities that distract attention, and compliance-oriented bureaucratised management’83. These directly impact on how the organisation performs and, across the NHS at the moment, staff and managers feel overloaded, disempowered and are failing to deliver the high quality care that they seek to achieve. These three elements of organisational culture – goal clarity, clear priorities and an empowering management style – all therefore need to be addressed.
- Goal clarity – Implementation of the REFOCUS intervention15 in England was directly related to staff perceptions about organisational commitment82, i.e. did the Trust really want to change? The commitment of the organisation was judged by staff on the basis of resource allocation (e.g. what training is compulsory and back-filled?) and the choice of Key Performance Indicators and outcome measures currently used by the Trust. Put simply, the dimensions an organisation chooses to notice (and then either celebrate or punish) send a powerful message about its core business – what it is really here to do. If these don’t reflect recovery concepts and values76 then staff will not think that the organisation is really committed to delivering a more recovery-oriented service. One approach is to collect and publish recovery-related outcome data76, such as the proportion of people on the caseload meeting normal citizenship expectations (e.g. meaningful occupation, decent housing, at least one close relationship, enough money to live on) and personally valued life goals84.
- Clear and recovery-focused priorities – A grounded theory study (n=97) across England showed that staff experience conflicting organisational demands and priorities85. This was confirmed in a systematic review which found that organisational priorities influenced staff understanding of recovery support86. However, simply having a clear priority does not guarantee that recovery is being supported, especially when there are multiple meanings of the word. Thus, there is currently a rather cynical conceptualisation of ‘recovery’ which sees it as simply subservient to the financial needs of the organisation, using success indicators such as cost reduction, throughput, discharge, and setting limits on service provision. Although this co-opting of the word ‘recovery’ to meet organisational goals has been criticised by both the people who work in services2 and those who use them87, nevertheless it persists. It highlights the need not just to set recoveryoriented priorities but to be clear about what this means. This involves addressing questions such as how the Trust Board will know that people recover, and from a wider sociopolitical perspective how Trust activities relate to the public health agenda, support community resilience, address health inequalities and improve overall population health.
- Empowering management style – There is a close link between empowerment and wellbeing in the workplace88 and there is also good evidence that improving staff wellbeing improves the experience of care89. We should therefore be thinking about ways to increase feelings of empowerment among frontline staff (and users). One way that we have found very useful in achieving this in the ImROC programme has been the use of a team-based, practice development instrument, the Team Recovery Implementation Plan (TRIP) as described in Challenge 260. The TRIP operates at the first level of leadership in the organisation (frontline staff and people who use services) but, of course, leadership is to be found at all levels and in all disciplines. Furthermore, organisations don’t change from the ‘top down’, or the ‘bottom up’: they change when leadership at all levels of the organisation are giving consistent messages. ‘The most important determinant of the development and maintenance of an organisation’s culture is current and future leadership’90. This is why any attempt to help services become more recovery-oriented in their practice must grapple with the organisational context (for example by engaging in compassionate leadership91), not simply the behaviour of individual staff members or groups. Addressing organisational inhibitors (e.g. bureaucracy, paperwork, caseload size, Serious Untoward Incident processes, safety policies, risk averse cultures) has been one of the most important lessons of ImROC.
“My experience of recovery focused management is having a manager who can have a conversation with you that leaves you feeling supported and like they are getting to know you as a person. Someone who has got to know your particular skills, interests and expertise, and has the confidence in you to take responsibility in those areas for the benefit of the team as well as for me as an individual.”
Physical health and wellbeing lead
Economic evidence
There is little economic evidence specifically on the notion of recovery focused leadership and a culture of recovery, but this Briefing Paper has highlighted the value of other aspects of meeting the key challenges of recovery. Effective recovery focused leadership potentially should improve the working environment. A management style that empowers frontline workers and service users to make co-produced decisions is consistent with the principles of a healthy workplace environment. Following the implementation of TRIP in one ward in a London Trust the level of staff sickness absence and assaults on staff over the following year decreased, but a comparative evaluation is required in order to determine whether this reduction is due to TRIP60. More broadly the economic benefits of a healthy workplace environment that may arise in part due to a recovery-focused orientation, such as improved productivity, innovation and creativity, as well as reduced absenteeism and staff turnover are set out in response to key challenge 9. The economic benefits of a co-produced and recovery focused approach to safety management are set out in key challenge 6.
Key organisational challenge 5: Increasing personalisation and choice
Key concepts: Personal budgets; WRAP; Advocacy
This relates to both personal budgets (addressed in key challenge 10) and approaches to supporting self-management and personal control (addressed in key challenge 1). The focus here is on the translation of these challenges through care planning and advocacy processes.
“For me my Health and Wellbeing plan is a way I can manage my life. It constantly changes but it makes me reflect on the things I can do for myself and what I need to do to keep balanced. This has helped me inform my careplan, but that is always something I have felt more imposed on me. It’s my Drs opinion of what they need to do, it never really helped me know myself. As you know. It gave me a context to hang the strategies I already had and used, I just hadn’t seen them that way before.”
Peer trainer
Research studies
As different people’s recovery journeys are different, a central task for mental health services is to ensure that individual care is genuinely personalised and maximises involvement and choice. This is not easy. Despite repeated exhortations, in various Department of Health policy documents over many years, a cross-sectional study of care planning in England and Wales found that care planning remains very bureaucratic, often with little evidence of user involvement or shared decision-making, and lacking in clarity regarding support for personal recovery92.
One way around this is for services to use specific tools aimed at documenting personal recovery plans. The Wellness Recovery Action Planning (WRAP) provides such a framework and covers developing a personal plan, coping with distressing symptoms, managing crises, and staying ‘well’. It was designed by a service user for service users and has been widely used around the world93. WRAP guides the individual or group to reflect on what has assisted them to stay well in the past and to examine strategies that have assisted others with their recovery. The focus is on approach motivation (defining wellness and supporting goal striving) rather than avoidance motivation (e.g. symptomatic relief), in line with the insight from positive psychology that positive (‘approach’) goals are more likely to be sustainably attained than negative (‘avoidance’) goals94. The process also relies on peer facilitation to activate the hope-inducing benefits of authentic role models95. A large randomised controlled trial involving people using community mental health services in the USA showed positive results for WRAP in terms of reduced symptomatology, increased hope and quality of life compared with standard care96.
Whatever their derivation, Personal Recovery Plans should contain an identification of the person’s internal and external resources and a plan for how they can use these to achieve their chosen goals. It is also desirable that they are clear and as short as possible. The person should not necessarily have to share their recovery plan with staff: it belongs to them. This creates new expectations about role expectations and the balance of power. So recovery plans are not the same as care plans, although there should be as much overlap as possible between the two. Learning from maternity services in which the mother owns her plan may be relevant.
“Recovery plans are not the same as care plans”
“It [Health & Wellbeing Plan] makes me more reassured and less stressed to know that we have a way to communicate easily and effectively with others involved in his [my son’s] life.”
Carer
Economic evidence
There is limited evidence on the resource impacts of individual care planning. Some approaches in England to care planning have been criticised for excessive paperwork and bureaucracy, whilst reforms in the way in which mental health services are paid for may act as a disincentive towards genuinely individualised care plans92. The business case needs to be strengthened for mechanisms to promote increased personalisation and choice. WRAP has been the subject of some economic assessment. A randomised trial in the US found that compared to individuals who received non-peer delivered nutrition or wellness education, individuals who received WRAP subsequently made use of fewer mental health services over an eight month follow up period, which implies a reduction in health care costs. Their perceived need for services also reduced, while both groups had positive recovery-related outcomes97. In a small qualitative study in Ireland some service users cited how WRAP had helped them avoid hospitalisation98.
“I meet with people and we try to identify what they would like to do and how best they can achieve their goals supporting them on their road to recovery…..I support people to complete the Self Directed Support (SDS) questionnaire….For me the most important part of this is encouraging and enabling the individual to rediscover passions and hobbies that they may have forgotten about/or think is no longer possible because of their mental health and I also encourage and support them to try something new.”
Peer support worker
Key organisational challenge 6: Changing the way we approach risk assessment and management
This key challenge has been updated in the light of experience.
Key organisational challenge 6: Reducing restrictive practice; changing conceptions of risk as something to be avoided towards working together to improve safety
Key concepts: Safety planning; Seclusion and restraint, No Force First
“Professionals and people using services need to work together to agree the right balance of risk and choice.”
Research studies
Accurately predicting the risk of violence or self-harm in a given individual is extremely difficult99. However, notwithstanding the lack of evidence that it is possible, mental health services have become increasingly preoccupied with procedures for the assessment and management of risk and this has sometimes become a barrier to personal recovery100. Many staff have become so risk averse that they are no longer prepared to engage in what might have previously been seen as positive risk-taking, i.e. working with the service user to help them manage those risks which are necessary for them to pursue reasonable and realistic life goals101. This has happened despite clear government and professional guidance to the contrary102. A 2016 article in the British Journal of Psychiatry concluded that risk prediction is not only ‘futile’, it is ‘potentially harmful, confusing clinical thinking’103. Instead the authors argued ‘for a shift in focus towards real engagement with the individual patient, their specific problems and circumstances’ (p.271).
Real engagement with the individual in the context of risk management is exemplified in the work done on safety planning104. Safety planning is not casual or reckless, but it promotes a way of working with risk that enables practitioners to support people in taking risks as a route to positive outcomes.
The change in language from ‘risk’ to ‘safety’ also recognises that risk is an inevitable part of life and should be an integral part of informed (and shared) decision-making regarding a person’s life goals. Professionals and people using services need to work together to agree the right balance of risk and choice. For people using services, it is important to be an active participant in conversations and subsequent decisions about keeping themselves safe. This way they contribute to, and see the relevance of certain decisions, and are more likely to feel able to take responsibility for letting staff know what can be done to help them feel safe; what their ‘triggers’ are; what can be done to avoid or minimise these situations. Thus they are able to take more responsibility for their actions and to learn how to increase their confidence in managing their own risk. This process of ‘co-producing’ (see key challenge 7) their safety and wellbeing plans at every stage in the process has not been empirically investigated.
One area where the management of risk is based on much greater involvement of service users is regarding the reduction of serious and violent incidents in hospital, particularly those which result in the use of physical restraints, seclusion or forcible medication. Research in the U.S. identified ‘6 core strategies’ for reducing seclusion and restraint in hospital105 106. These are shown in Box 4.
Box 4: Core strategies for reducing seclusion and restraint
- Ensuring leadership to support organizational change, involving the senior management team
- Developing the workforce (training in de-escalation techniques, ‘trauma induced care, modifying the environment, etc.)
- Planning ahead to prevent incidents occurring
- Developing the roles of service users as staff trainers, advocates and peer workers
- Using debriefing techniques to promote learning.
- Using data to inform practice
“It goes without saying that it can at times be quite emotive seeing people suffer from their mental illness or from the effects of being sectioned, particularly having been there myself and being able to identify with their pain and frustrations. It was initially quite hard to see the use of physical interventions but going on the training helped to ease my discomfort and gave me an opportunity to provide valuable feedback so that the training can be developed to be more recovery focused.”
Peer support worker on acute inpatient ward involved in co-producing de-escalation training
A training curriculum based on these strategies has been developed and evaluated across 43 facilities in 7 States over a fouryear period107 108. Two-thirds (n=28) were able to achieve stable implementation, and on these sites 54% were able to reduce restraint hours by an average of 55% and the percentage of people restrained by an average of 30%. Reductions in seclusion and restraint were less impressive where full implementation was not achieved. There were also increases in both user and staff satisfaction, significant reductions in staff turnover and related costs. These results have also been replicated in Canada and a similar study is currently being conducted in England by Professor Joy Duxbury.
A second example of reducing seclusion and restraint which is based directly on the implementation of recovery principles has been reported by Ashcraft and colleagues109. They called their approach No Force First, and used similar strategies to the six described above with an emphasis on leadership, staff training, consumer debriefing and regular feedback. However, they placed the contribution of service users as trainers, alongside staff, at the centre of the initiative. With constant support they were able to eliminate seclusions and restraints in two crisis centres over a period of two-and-a- half years. Later revisits found no replacement with chemical restraints. The No Force First approach has been replicated in this country, particularly by Mersey Care NHS Foundation Trust. It explicitly uses a process of coproduction, with professionals and service users working together to design, implement and evaluate the programme. Early data from two pilot wards assessed over two years indicated 60% reduction in physical and medication-led restraint, 46% reduction in staff assaults, staff sickness reduced by 25%, improved staff morale and satisfaction, and a positive improvement in service user experience110 111. As a result, the Care Quality Commission positively acknowledged No Force First as a restraint-reduction strategy. More generally, there is evidence that coproduced approaches to reducing violence on wards are effective, from trials in Finland112 and Spain113.
Economic evidence
There are substantial costs associated with seclusion and restraint, some of which may be averted through the adoption of a coproduced approach to safety management. A number of studies have highlighted costs for service users and staff related to adverse health impacts, such as injuries, falls and deaths114. Agitation and distress, which can be inevitable consequences of restraint, have themselves in a review been associated with longer inpatient stays115. Analysis in Spain also suggests that the costs of managing agitation in service users using seclusion and restraint are roughly three times the costs of verbal or psychological actions alone116.
There are substantial costs associated with the intensive levels of staff time that are needed for the management and implementation of traditional seclusion and restraint policies. One costing study in England estimated the costs of managing conflict and the use of restraint on adult inpatient psychiatric wards in 2005117. It estimated that around 50% of all nursing resources were taken up in the management of conflict and use of containment strategies. Costs of manual restraint per year per ward were reported to be £14,084 while costs of seclusion were a further £5,007.
There will also be legal and other costs associated with adverse events arising from the use of restraints. Although not well studied, violence and injuries are likely to have an adverse impact on workplace staff sickness rates and staff turnover, implying further costs to mental health care systems118. The mean costs per violent incident were estimated to be £3,212 in six inpatient wards in East London, of which 54% was for staff sickness absence, and replacement staff costs, with the remainder attributed to response team costs, legal costs and medication119.
Few studies outside of the US have evaluated the economic impacts of introducing measures to reduce the use of restraints118. For instance one US study looked at the impact of a policy to reduce the use if restraints at one inpatient facility for young people aged 13-18120. The costs of staff time and medication related to restraint reduced by 91% in the year following the introduction of the policy – 3,991 restraint events fell to 373 events. Costs for managing restraint were then just 8% of what they had been prior to the policy change.
More potential benefits can also be seen in a randomised trial in Finland of a co-produced approach, which found that staff time for seclusion and restraint could be significantly reduced without any increase in violence, although impacts on staff sick leave were equivocal121; it did not however report actual changes in costs. The No Force First pilot study in Merseyside did realise estimated savings of £0.25 million per annum in secure awards alone due to reduced staff sickness and absence related to assaults and injuries, according to an independent assessment110. This assessment also concluded that scaling up implementation to all wards potentially might avoid costs of £1.2 million per annum.
“Another area where peer support has helped, I believe, is in the use of physical interventions. I think those who have been there have an awareness of how apparently trivial issues, like not being allowed to go out for a cigarette for example, can become magnified when you’re an in-patient, and how quickly such situations can escalate and result in physical restraint. Working on a very busy in-patient ward, I think my particular focus has been on trying to identify and respond quickly to the day to day individual issues that arise for service users in a way that prevents any escalation. I’ve found it be very helpful just talking quietly to the person, acknowledging (with the benefit of lived experience) just how difficult and frustrating their current situation is, and trying to figure out solutions together.”
Peer support worker
“I completed my health & wellbeing plan and asked for the advanced statement part of it to be scanned onto my notes. Many months later, I experienced a ‘blip’ and ended up in A&E. The doctor got a copy of my plan and reminded me of what I had said would be helpful in a crisis. Just being able to share this information in this way made a massive difference and I was in a position to return home much sooner than had ever happened before.”
Peer trainer
Key organisational challenge 7: Redefining user involvement
This key challenge has been updated in the light of experience.
Key organisational challenge 7: User involvement is replaced by fully resourced coproduction so that the views, experiences and aspirations of people using services and their family members are accorded the same value as the views of staff in the organisation
Key concepts: Co-production; Power
Research studies
The importance of user and carer involvement in mental health services has been emphasised for many years. However, making it a reality is difficult and timeconsuming, and many services are still essentially staff-led, with users and carers being consulted at the end of the process when most of the important decisions have already been taken. For this reason when we have been promoting services to support recovery through ImROC we have continually come back to the concept of co-production.
Co-production represents a new way of thinking about the delivery of health services. The ideas came from an analysis of the difficulties faced by public bodies in delivering effective and relevant services in times of economic austerity. They have been popularised in England through the work of independent think-tanks such as the New Economics Foundation (nef) and Nesta. In a seminal publication they defined coproduction as, ‘delivering public services in an equal and reciprocal relationship between professionals, people using services, their families and their neighbours. Where activities are co-produced in this way, both services and neighbourhoods become effective agents of change’ (p.11)122.
According to the New Economics Foundation, Nesta and the Innovation Unit123 the main features of co-production are shown in Box 5.
“It [co-production] feels democratic and about mutual respect, rather than pity. It’s about everyone learning together. It feels exciting. It just feels so much better.”
Mental health worker
Box 5: Key features of co-production
- Recognising people as assets – transforming the perceptions of people as passive recipients of care and ‘burdens’ on the system, to equal partners in designing and delivering services.
- Building on people’s existing capabilities – actively supporting people to recognise and use their strengths, rather than conforming to a deficit model.
- Reciprocity and mutuality – offering people who use services opportunities to develop reciprocal relationships with professionals (and with each other) and enter into mutual responsibilities and expectations.
- Peer support networks – enhancing knowledge generation and transfer through engaging personal and peer networks alongside those of professionals.
- Breaking down barriers – blurring the distinctions between professionals and producers and consumers of services. Reconfiguring the power relations and the way services are developed and provided.
- Facilitating rather than delivering – enabling professional staff to become catalysts of change, instead of sole providers of services.
“Co-production represents a new way of thinking.”
Co-production is about doing things with people, rather than for or to them. It assumes that the people who use mental health services and their carers have specific knowledge and expertise that traditional professionals don’t have (or at least not in the depth that service users and carers have it). It further assumes that both professional expertise and personal experience are important, so the most effective services arise from both parties being fully involved in their design, delivery and evaluation.
Co-production is not the same as the ‘big society’. It is not simply using service users and carers to do the traditional things that professionals do without training or paying them appropriately. Co-production is about service users and carers working together with professionals in different ways, bringing their experience and expertise to produce different solutions, and then integrating these – wherever possible – with professional approaches, e.g. in Recovery Colleges (key challenge 3) or Peer Support (key challenge 8). Co-production is therefore explicitly about a change in the power relationship between professionals and people who use services124. This is probably the most controversial and challenging implication of trying to work in this way.
Nevertheless, the value of co-production for public services is now widely acknowledged. It underpins policy initiatives in England (e.g. People Powered Health programme123, Cocreating Health125 126), Wales127 and Scotland128. For people using services it means improved outcomes and quality of life and better, more realistic and sustainable, public services. For frontline staff it means shared responsibility and increased job satisfaction from working with more satisfied service users. For managers it means more positive ways of limiting demands on services, making them more efficient. For all citizens it means increasing social capital, social cohesion, and reassurance about the availability and quality of services in the future. True co-production must therefore lie at the heart of mental health services which aim to support recovery129.
“I know first-hand, just how transformative being involved in co-production can be. I have moved from feeling I was just a burden on services to now being full involved in helping to develop them… At one time the only adults in my life were mental health professionals, now I have work colleagues and a network of friends!”
Peer trainer
Economic evidence
In many cases evaluations that have looked at co-production have not put an economic value on the benefits of this approach. In order to calculate the return on investment it is important to know about the financial costs of supporting co-production. Little information has been published on these costs, but it is likely that value of the time and other inputs of people with lived experience into co-production will more than outweigh additional formal resources that are required. Co-production in effect should provide net additional resources and capacity to mental health services. This hypothesis needs though to be formally tested.
It is also important to know what the economic consequences of co-production are. A review of evidence on co-production in mental health identified a number of studies (both small scale evaluations and trials) that reported an association with reduced health care costs, e.g. for medications and specialist mental health services. The review also identified benefits from improved social functioning outcome, e.g. employment and reduced dependency on public services124.
Recently a significant trend in reduced costs in contacts with health and social care services six months and nine months after beginning to participate in peer support groups was observed in England. This uncontrolled analysis combined the experiences from people involved in one or more peer support activities, including online peer support. Overall, including impacts on employment, education and volunteering, costs were 28% lower than baseline at 6 months and 53% lower at nine month follow up130.
This finding reinforces an earlier review which suggested that “an approach which may also in time offer the biggest scope for cost savings in mental health care is to promote and expand co-production, drawing on the resources of people who are currently using mental health services, for example in peer support roles”1 (p.6).
“Co-production is about doing things with people, rather than for or to them.”
“As a service-user, I’ve been asked a quite a lot about my opinions on the professional’s ideas in mental health services, but now through co-production, I am able to also share my ideas and hear the professional’s opinions on these. That is really empowering!”
Service user
Key organisational challenge 8: Transforming the workforce
Key concepts: Peer support workers; Peer trainers; Stigma; Staff attitudes
“Working as a Senior Peer Support Worker is an opportunity that is beyond any expectations that I had when I was unwell. During my time in hospital I thought a lot about wanting to use my experience as a way of supporting others in future, in order to help them feel understood and less alone. At the time I never thought this role would exist and I feel privileged to be part of an initiative that I believe has and will continue to have an invaluable impact on mental health services. Doing this work gives me a sense of purpose, and has given meaning to the difficulties that I went through in the past. I believe that my role keeps me motivated to keep well and look after myself, in order to support others in doing the same and this responsibility has added huge value to my daily life and future aspirations.”
Peer support worker
Research studies
In addition to Recovery Colleges, the other most visible sign of services moving explicitly towards supporting recovery is the inclusion of peer workers. These are individuals with mental illness who use their lived experience to support others to recover131. The value of peer support has long been recognised in mental health services132 but only recently have peer workers begun to be taken seriously as an effective addition to the workforce. A Cochrane review conducted in 2013 identified eleven randomised trials involving 2,796 people, showing equivalent outcomes from peer support workers compared with professionals employed in similar roles133. Wider reviews using a greater range of studies have shown more positive effects134 135 136. These are summarised below.
- In no study has the employment of peer support workers been found to result in worse health outcomes compared with those not receiving the service. Most commonly the inclusion of peers in the workforce produces the same or better results across a range of outcomes.
- The inclusion of peer support workers tends to produce specific improvements in service users’ feelings of empowerment, self-esteem and confidence. This is usually associated with increased service satisfaction.
- In both cross-sectional and longitudinal studies, patients receiving peer support have shown improvements in community integration and social functioning. In some studies they also bring about improvements in self-reported quality of life measures, although here the findings are mixed.
- In a number of studies when patients are in frequent contact with peer support workers, their stability in employment, education and training has also been shown to increase.
Some of these findings are not replicated across all studies depending on the methods used and the quality of the evidence (which is quite variable). Nevertheless, the overall evidence shows that having contact with a peer support worker leads to an increased sense of empowerment and positive benefits in terms of social inclusion. The next frontier is therefore implementation, and both ImROC137 138 and others139 140 have developed guidance to assist in this process.
“One of the main benefits to working with a peer support worker is that of positivity; seeing someone who has experienced mental health problems but has moved forward and is now working. I believe the PSW is good at validating service users’ experiences whilst also seeing the potential in people and being able to identify people’s strengths rather than looking at all the negatives.”
Mental health worker
If individuals are to be supported in their personal recovery by traditional staff or peers then staff have to believe that it is possible. There is evidence that some mental health professionals still hold stigmatising views about people using services141. This ‘othering’ behaviour – emphasising differences rather than commonalities – can foster low expectations and negative attitudes to the possibility of change hindering the development of ‘non-patient’ identities and getting in the way of recovery. This needs to change and we therefore need to think about how to change staff attitudes so as to make them more generally supportive of recovery.
The most effective approaches to reducing stigma in the general population are those that include direct contact between persons from the stigmatised group and those that hold the stigmatising attitudes142. If managed correctly, this contact should allow both groups to identify and share their common humanity, which then breaks down stereotyped attitudes. An early peer support service in assertive outreach found that peer workers “created a more positive attitude toward persons with mental illness”143. A comprehensive review concluded that antimental health stigma programmes aimed at staff should contain personal testimony from a trained and enthusiastic speaker who has lived experience and who shows that recovery is both real and possible, demonstrating by their example competence and a successful way of living144. This is what peers do, and so the inclusion of peer workers in the workforce should be a powerful way of addressing negative staff attitudes. Where peer workers are well-established there is good anecdotal evidence that this is indeed the case. Thus, the inclusion of peer workers not only has direct benefits for people receiving this service (and for those delivering it) it also contributes to changing the organisational culture so as to make support for recovery more generally acceptable.
“Having contact with a peer support worker leads to an increased sense of empowerment and positive benefits in terms of social inclusion.”
Economic evidence
It can be difficult to distinguish between studies focused on the economic benefits of peer worker interventions and other types of peer support interventions. Evidence on the broader benefits of peer support interventions was discussed in challenge 7. Here we focus on the economic case for peers who are salaried members of the workforce, though studies on volunteer peer workers have also been conducted.
One review looked at the impact of paid peer workers on the use of psychiatric hospital beds, where peer workers provided additional services such as befriending, mentoring or advocacy in community mental health teams or in the community145. Six studies (one from Australia and five from the US) were identified, four of which generated a positive return on investment, with a weighted average return on investment of almost 5:1. While this is a limited evidence base, the economic benefits may be understated as the analysis does not take account of any positive impact on quality of life and other outcomes.
Findings from one of the US studies in this review were used to help model potential cost savings to the mental health system in England through peer mentoring, although the precise value of mental health specific savings was not reported146. This analysis may be limited by its assumption that changes in the future use of psychiatric services in one hospital in Connecticut through the use of peer mentoring would apply to the English context147.
A pilot randomised trial in the UK looked at 4 weeks support provided by peer support workers to people who had recently been discharged from inpatient mental health care148. The study was too small to identify any statistical differences in costs or outcomes, but did suggest that a larger study might be able to confirm the observed good probability of being cost effective. Another US study looking at the use of peer mentors in homeless veterans found no difference in the costs or use of health services149.
“There is no sense of ‘us and them’ in our team, and I feel that the unique perspective that I have brought having been a service user on the ward, who understood first-hand how it can feel, was genuinely appreciated. I saw how perceptions and stereotypes relating to mental health could be transformed by having someone that used to be a patient on the ward working there. More than one colleague and a number of service users have said things along the lines of “I can’t believe you were ever on the ward!” Many said in different ways, that they were inspired by seeing such a thing was possible – I know because two years ago I’d have agreed with them!”
Peer support worker
“I would like to think that my practice very much embraces the concept of recovery, yet (the peer support worker) has arrived and made me pause and rethink, not in a critical way but in a gentle questioning way.”
Consultant psychiatrist
Key organisational challenge 9: Supporting staff in their recovery journey
This key challenge has been updated in the light of experience.
Key organisational challenge 9: Supporting staff to cope effectively with the stressors that are inevitable in working in mental health services
Key concepts: Lived experience in the workforce; Reducing absenteeism and presenteeism; Expertise in wellbeing
“Supporting staff makes sense every way you look at it.”
Research studies
Supporting staff makes sense every way you look at it. Stressed, demotivated and demoralised staff either go off sick or are vulnerable to ‘presenteeism’ (consistently under-performing at work) – both of which reduce organisational effectiveness. However, there are further recovery-specific reasons to attend to staff wellbeing.
First, to harness the un-tapped resource of lived experience in the non-peer workforce. A national survey found approximately 2 in 5 of the NHS mental health workforce have personal experience of mental ill-health, and over three-quarters have supported a family member or friend with mental health problems150. However, less than half had fully disclosed their lived experience to colleagues. Initiatives around ‘valuing the life, lived and professional skills and experiences of staff’151 will involve organisational leadership with engaged support from human resources.
Second, there is evidence that staff hold different views about sources of wellbeing for themselves compared with people using their services. Mental health staff in England hold a more deficit-based perspective on wellbeing for service users and a more strengths-based view for themselves (i.e. ‘they’ need fixing but ‘we’ need a meaningful and enjoyable life)152. Developing expertise in sources of resilience and wellbeing as a core part of professional experience has the potential to positively impact on this anti-recovery attitude.
Third, developing expertise about wellbeing makes ideas about recovery easier to understand. For example, the CHIME framework aligns very closely with the Foresight work on mental capital153, summarised by the New Economics Foundation as five-a-day for wellbeing: Connect, Be active, Take notice, Keep learning, Give154. Supporting the development of worker expertise in wellbeing will increase their skills in support recovery, because in many senses wellbeing is recovery155.
Finally, as noted in key challenge 4, improving staff wellbeing is a pathway to improve the experience of using services: ‘Individual staff wellbeing is best seen as an antecedent rather than as a consequence of patient care performance; seeking systematically to enhance staff wellbeing is not only important in its own right but also for the quality of patient experience’89.
Specifically in relation to wellbeing in the workforce, evidence-informed strategies are now possible. A systematic review of workplace interventions for common mental disorders such as depression or anxiety synthesised 140 reviews including 20 of moderate or high quality, incorporating findings from 481 studies156. The review identified empirically-supported approaches to primary prevention to reduce onset (enhancing employee control, promoting physical activity), secondary prevention to mitigate effects (cognitive-behavioural therapy-based stress management), and tertiary prevention to support symptom reduction and return to work (exposure therapy, CBT-based and problem-focused return-to-work programmes).
“He (the nurse) just seem really tired and stressed and like he just did not have the energy to bother with me at all, let alone care about me.”
Experience of being treated by stressed, demotivated and demoralised staff
“She (the doctor) looked at me, but there was no eye contact and she rushed me away. It made me wonder what she’d been on. She seemed in a worse place than me.”
Experience of being treated by stressed, demotivated and demoralised staff
“A long time ago, I saw a doctor after I’d attempted to take my own life. I remember that he asked me what it proved? I replied ‘a lot.’ I never saw him again and I heard that he took his own life. I’ve often wondered if my comment had an effect on him.”
Experience of being treated by stressed, demotivated and demoralised staff
Economic evidence
It has been argued that an extension of the recovery based approach to the health and wellbeing of staff working in mental health services may help the NHS to have a healthier workforce and reduce levels of absenteeism151. In fact many of these principles, e.g. empowering staff to have more control over the way that they work, focusing on workplace environmental factors that can be conducive to occupational stress and poor mental health, flexible working arrangements, increasing the value that line managers place on their staff and the importance of maintaining contact with staff when they are on sick leave are entirely consistent with what are now regarded as key approaches to promoting mental health and wellbeing in the workplace157-159.
Moreover there is a strong business case for adopting these principles for workplace mental health promotion programmes. While most of the evidence tends to focus on specific interventions, such as the introduction of workplace wellbeing programmes or brief psychological support for staff experiencing stress, there is also a recognition that broader workplace measures such as training for line managers to recognise stress and workplace environmental assessments, including measures to establish a healthy working culture, can generate positive returns on investment to workplaces, including health services160. Positive benefits include a reduction in sickness absence, presenteeism, staff turnover and early retirement. There is a very broad literature on the level of return on investment from these types of workplace health promotion activities. While caution must be exercised on how the results of these studies are interpreted as many different methodologies are used in different country contexts, in broad terms there tends to be at least a 2:1 return on investment to the workplace of evidence-based actions to address common mental disorders and an even greater level of return on investment for some workplace (mental and physical) health promotion actions160.
Key organisational challenge 10: Increasing opportunities for building a life ‘beyond illness’
This key challenge has been updated in the light of experience.
Key organisational challenge 10: Prioritisation of life goals (full citizenship and community integration) in all care planning processes
Key concepts: Housing First; Personal budgets; Individual Placement and Support (IPS); Community participation
“Leaving home at 16 was the start of a long personal journey into homelessness, and a 20 year battle with complex mental and physical health difficulties. After several intensive hospital admissions, time spent sofa surfing, in hostels, and insecurely housed, I became what is often termed a ‘revolving door patient’, with little hope of finding the way out. I now have a place that I can call home, a place that feels safe and warm and where I have the choice to stay for as long as it suits me.. .. I have skills and strengths that health care and social workers helped me to find and to build upon…The things that helped me to find a way to stop the door revolving, to find a door to a home, were being seen and respected as an individual, not being defined by my problems or my label of ‘damaged’ or ‘vulnerable’ or ‘homeless’ …Respect, compassion, empathy, being seen and heard and valued… Life being homeless is hard. People usually don’t end up homeless because they have had easy lives up to that point. Having no security, no stability, no support system, alongside the demoralising and damaging effect that homelessness can have on mental and physical health, where just surviving feels like a battle”
Peer researcher working with people experiencing homelessness
Research studies
If supporting recovery is about one thing, it is about placing the achievement of personal life goals (full citizenship and community integration) alongside symptom reduction as the major objective of mental health services8. This is reflected in a focus on housing, money, employment and social integration. There is now a robust evidence base for the effectiveness of a range of approaches to achieving these objectives and these now need to be (re)incorporated into service design.
Housing
Good housing is more than just shelter161: it is the bedrock of successful community living. Notwithstanding this simple fact, the topic of housing has received little attention over the years from mental health professionals. An exception to this rule is the Housing First initiative. This was developed in the U.S.A. to meet the needs of homeless people with complex mental health and substance misuse problems. It prioritises the identification of suitable housing, based on personal preference, and then delivers other supportive services to the person once they are housed, without a pre-requisite that their substance misuse must cease first. The use of permanent housing options and the commitment to floating support means that the resident does not have to make continual moves between different types of accommodation as their support needs change.
A definitive randomised controlled trial across Canada showed that homeless people living with mental illness (n=1,198) who received the Housing First intervention had increased housing stability over 24 months compared to those not receiving the intervention162. A qualitative study with a sub-group of participants (n=60) also found positive impacts on hope and recovery goals163. In this study, despite there being no requirement for the Housing First group to abstain from substance misuse, there was actually no significant difference between the two groups regarding their levels of drug and alcohol use. The annual per capita costs of the Housing First programme were also around half those of ‘treatment first’ programme. This approach has been tried in England164 but is not widespread.
Employment
The Individual Placement and Support (IPS) approach is now the best researched approach to supporting people with mental health problems to access and retain mainstream employment. It has a number of similarities with the Housing First approach in that it is also based on placing the person in a work position of their choice as quickly as possible and then providing them and with an integrated package of vocational and clinical support in situ. A 2013 Cochrane review (14 trials, 2,265 people) concluded that IPS ‘is effective in improving a number of vocational outcomes relevant to people with severe mental illness’165. IPS consistently achieves employment rates 2-3 times better than traditional alternatives such as pre-vocational training and sheltered workshops. This holds true in high and low income settings, across different countries, irrespective of the underlying employment rate. Longer term follow-up studies of people placed through IPS suggest that the higher rates of employment are maintained and have positive impact on non-vocational outcomes such as improved confidence and wellbeing, and reduced sense of stigma. The one study where IPS failed to produce such impressive results was where it was not implemented with good fidelity to the research model166 167. A more recent review and meta-analysis of 19 international studies also found that IPS was more than twice as likely to lead to competitive employment compared to vocational support even where economic growth was low168.
In contrast to supported employment, much less attention has been focused on assessing the cost effectiveness of supported education services to help young people remain in and complete their education, which in turn will increase career opportunities and earning potential. There is emerging evidence on adapting IPS to deliver supported education, for instance in Australia169.
Money
For people with serious mental health problems – as for the rest of the community – not having enough money clearly reduces both the meaning and enjoyment of life170. Since people with serious mental health problems are more likely than the rest of the community to experience poverty, it is specially important to ensure that they have access to financial advice in various forms1. The topic of material support is only recently receiving attention from mental health professions171 172.
An approach which aims to give the person direct control over a substantial proportion of their financial support is known as Personal budgets (or self-directed care). This has been tried both in the U.S.A.173 and in England174, and aims to provide the person with the resources that would otherwise be spent on services to allow them to spend them on whatever they think will be most helpful. This sounds like it must be a good idea, but there are considerable practical problems in its implementation, both bureaucratic and in ensuring that resources are effectively targeted on those in greatest need. The effectiveness of personal budgets also depends very much on the quality and continuity of the supportive relationships175. It therefore remains to be seen whether it will be possible to get personal budgets to work effectively and if they can be rolled out on a large scale in statutory services. (The best examples of effective use of personal budgets are currently still in the voluntary sector). If these problems of implementation could be successfully addressed then personal budgets could undoubtedly make a significant contribution to supporting community integration and social inclusion.
Social integration
Personal networks are important for recovery at an individual and a group level. Each one of us, whether living with mental health problems or not, can probably name a few key individuals who have helped us keep on going when times are tough. Close, personal, social supports help reassure, they shape identity, provide meaning to life, give a sense of belonging and access to new resources176. There is specific evidence that positive relationships can be the tipping point that starts a person’s recovery journey177 178. Similarly, feeling a part of the community, not just physically located within it, is a fundamental human need. However, despite the obvious importance of social support, interventions to support social network development have not been much researched in the mental health literature. Approaches like wellbeing networks and asset mapping179 therefore need to be given more attention and evaluated in terms of their practical value.
“People with serious mental health problems are more likely than the rest of the community to experience poverty.”
“I know only too well the barriers to getting (and using) treatment that come with the label of ‘homeless’. Not having support or the hope that things can be different… Lacking the confidence and understanding of unfamiliar health systems…Feeling undeserving, worthless… These things can make it impossible to even identify the help you so desperately need, never mind where to get it.”
CNWL Recovery Stories, 2014
“Positive relationships can be the tipping point that starts a person’s recovery journey.”
Economic evidence
There is a strong evidence base on the benefits of facilitating recovery and preventing relapse through actions that support education, housing and employment, and other aspects of social functioning1. In this Briefing Paper we can only provide a brief flavour of this evidence base. A key challenge though is to work effectively not only within the health sectors, but across sectors, such as with the private sector, financial services and banking sectors to reduce the risks of unmanageable debt, with employers, and not least with the non-government sector such as housing associations to both fund and implement evidence based actions.
It is vital to measure and highlight the personal, social and economic outcomes such impacts on the rate of employment, the completion of education and training, and securing stable housing, in addition to more narrow mental health specific measures of recovery. Achieving secure employment will benefit society through a reduced need for welfare support while better educational outcomes increase the likelihood of securing good employment. Employment in turn can promote independence. A lack of access to secure housing and employment, as well as unmanageable debt and poverty are also associated with an increased risk of future poor physical and mental health.
Housing
As well as being a key component of a recovery strategy, there are substantial economic opportunities along the care pathway to improve outcomes and reduce costs for mental health service providers through use of appropriate housing services, rather than more expensive mental health services. These housing options are heavily dependent on the level of housing stock available in any local area; clearly this is challenging in England.
Recovery may be aided by better access to long term (albeit still transitional) housing support as well as long term independent housing. Housing associations can play a very important role. For instance the ‘One Housing Group’ and an NHS Trust in London have developed a Care Support Plus model which initially provided 15 high quality self contained supported housing units, helping service users prepare for the transition to other forms of accommodation. The service has reduced hospital stays and costs to the health services by more than £440,000 per annum with a reduction in hospital admissions from a total of 408 weeks in the two years prior to the scheme compared with 57.7 in the subsequent two years, with a further 12 flats built180.
Looking at longer term support, a review of economic studies on Housing First in Canada, the US and Australia suggests that they ‘can lead to significant cost offsets. When considering improvements in housing stability, health, and quality of life, Housing First may be a very cost-effective intervention for chronically homeless populations’181. However the follow up time periods for most of these studies are quite short so less is known on long term impacts. Furthermore Housing First has had to operate in a climate with a severe shortage of social housing and affordable private-market housing in many Canadian communities. This can impact on the potential benefits of the programme.
“Around two-thirds of all of the costs of poor mental health are due to lost opportunities to participate in employment.”
The City of Toronto’s 2007 examination of the Streets to Homes programme found that the low supply of affordable housing resulted in a reliance on shared accommodation, which was less desirable to participants and generally led to worse outcomes, when compared to individuals housed in private apartments182. This is pertinent given the housing shortage in England.
An observational study of the Housing First approach in England reported decreased repeated homelessness for people who on average had previously experienced 14 years of homelessness. Potential cost-savings were estimated to be £15,246 per person per year, assuming potential savings between £4,873 and £3,098 per person in support costs, as well as from reductions in A&E visits and fewer contacts with the criminal justice system. While promising, sustainable funding will be an important factor for the continued success in the provision of this type of open-ended support183. This may also be dependent on rules governing entitlements in respect of housing benefit.
A national survey of 619 people from 22 residential care, 35 supported housing and 30 floating outreach services across England also looked at the costs of mental health supported accommodation services. It estimated mean costs of £371,445 for supported housing compared to £474,339 for residential care184. After adjusting for differences in need, quality of life was similar in supported housing to residential care, but with greater levels of social inclusion and a higher risk of experiencing crime. Floating support was much less expensive but associated with poorer quality of life outcomes and higher risk of crime.
Employment
Around two-thirds of all of the costs of poor mental health are due to lost opportunities to participate in employment. Most evaluations suggest that IPS is more effective than vocational rehabilitation in helping people return to competitive employment168. There is evidence particularly from the US on long term sustainability of benefits, although these have been hampered by funding structures185.
In Europe evidence from Switzerland indicates that higher rates of competitive employment can be sustained over at least five years: 43% employed for at least 130 weeks versus 11% in the vocational rehabilitation groups. In this analysis there were no significant differences in overall costs of the two programmes – the higher costs of the supported employment programme were offset by reduced in patient admissions and lengths of stay. However mean incomes from employment in the supported employment group in the study were also almost double those in the vocational rehabilitation group186.
A review of economic studies drew the conclusion that in the English context IPS would pay for itself within a year – with then annual costs per individual of £2,700 being offset by reductions in the use of mental health services of more than £3,000 per annum187. In an earlier multi-country trial, including supported employed in London, IPS was found to be less costly than vocational rehabilitation, with an overall mean net benefit to society, taking account of additional productivity through employment, of £22,615 per client compared to vocational rehabilitation services188.
“So it’s the day after my release…I’m on my way to sort out my script and prevent myself from going in to withdrawals and using. The first key worker I saw there was brilliant! Not only did she ensure my script…she also spoke about actually where to go from here….the ambition I had from before drugs was slowly coming back but I didn’t honestly know how to get back into society and work etc.”
CNWL Recovery Stories, 2014
“Good housing is more than just shelter.”
These findings can be replicated even in very different country contexts: a recent evaluation of IPS plus psychological therapy was compared with traditional vocational support in Japan. At one year follow up while there were no overall differences in costs between the two groups, rates of employment were higher and clinical outcomes better in the supported employment group189. In contrast to employment, insufficient attention has been given to the assessing the economic case for comparable supported education services; a gap in the evidence that should be addressed.
Money
Evidence on the cost effectiveness of personal budgets is modest, in part because evaluations have tended to focus on different client groups rather than people with mental health needs. A systematic review on personal budgets for people with mental health problems only identified cost effectiveness evidence in two of 15 studies assessed190. The more recent of these English studies concluded that the additional cost of delivering personal budgets was a cost effective use of resources given the improvements in quality of life and neutral impact on costs191.
However, there remain many logistical and administrative challenges in expanding the use of personal budgets; the flip side of more individual choice is that the sustainability of existing services and supports is also weakened. Some of these issues may be explored further in ongoing evaluation of the relatively new Integrated Personal Commissioning areas that are being rolled out in England. These IPCs can include personal budgets as one element of an approach that in theory should be co-produced with service users192.
People with some mental health needs may also be particularly vulnerable to falling into debt. Financial difficulties reduce the likelihood that people will recover from mental health difficulties. Investing in services that provide specialist welfare advice to people with mental health needs is likely to be a cost saving intervention even if only a small number of clients then have a reduced risk of using inpatient mental health services193. A recent economic modelling analysis suggests that the provision of face to face debt advice would aid recovery rates from depression, with costs of service provision being more than outweighed by a small reduction in costs to the NHS and a much greater impact on the wider economy by decreasing barriers to work194. Other new modelling work also suggests that there is a return on investment to face to face debt advice services of almost £3 for every £1 invested due to the avoidance in the general population of depression and anxiety problems associated with problematic debt195.
“There is a strong evidence base on the benefits of facilitating recovery and preventing relapse through actions that support education, housing and employment.”
Conclusion
We have considered a broad sweep of evidence and across a wide range of subject areas. That is inevitable with a topic like supporting recovery since it is as much about a set of underlying ideas, principles and values which can be applied to almost any intervention, as it is about the effectiveness of specific approaches. However, we believe it may be helpful for commissioners, health and social care leaders, and other stake-holders to be aware that there is a defensible and growing business case for the ten key organisational challenges.
Where the business case can be made specific, the traditional outcome evidence is – unsurprisingly – patchy. The scientific evidence supporting self-management (Challenge 1) is compelling and the emphasis on ‘learning’ – particularly joint learning (‘coproduction’) is highly consistent with modern educational thinking (Challenges 2 & 7). The evidence regarding the effectiveness of Recovery Colleges is promising (Challenge 3), but, at present, it is methodologically weak. A recovery-oriented approach to leadership and management (Challenge 4) is also very much supported by a substantial literature on organisational change, and a highly individualised approach to the planning and delivering of care (Challenge 5) is globally accepted as the bedrock of good practice in mental health services. Staff are also commonly overworked and undervalued, so the evidence that practising in a way that supports recovery is helpful to their morale and well-being (Challenge 9) is therefore potentially very important. There is good randomised controlled trial evidence supporting the value of peer support workers (Challenge 8), and the evidence in favour of the benefits of helping people pursue common personal recovery goals – stable housing, employment, financial support, social integration (Challenge 10) – is well established. Thus, the overall picture is of general support for a recovery-oriented approach, with more evaluative evidence needed, but strong evidence for high service user satisfaction and promising evidence for cost-effectiveness in certain key areas. It is this general picture which led the World Health Organisation to make supporting recovery one of its central organising principles for mental health services across the globe3.
In terms of the strength of the evaluative evidence it is not surprising that randomised controlled trials are relatively rare. This is generally a new approach and it will take time for researchers (and funders) to catch up with the promising nature of these new developments and give it rigorous attention. However, this is balanced by the very strong evidence for increased satisfaction from people who use recovery-supporting services. In our view it is unusual for service developments to have generated such consistently high support from the people who use them – and from most of the people who deliver them. This leads us to believe that supporting recovery is a process which taps into some of the basic reasons why people approach mental health services for help and the essential motivation of staff to try to help them. This has to be a powerful combination.
Finally, we believe that supporting recovery may be a part of the solution to the global crisis of apparently almost limitless demand for care in the face of increasingly constricted resources. If these two pressures are to be reconciled we believe it will require a fundamental rethink of not only what is delivered by mental health services, but also how it is delivered. As part of this reevaluation we believe that governments, managers and practitioners will have to redefine their goals and re-examine their workforce. Our speculation is that this transformation will involve changes in skills (such as a far greater emphasis on coaching to support self-management), structures (e.g. more partnerships with, and working through, community resources) and workforce, with the involvement of many more peer workers alongside traditional professionals. This transformation is perhaps the most daunting – but exciting – challenge.
Acknowledgements
We would like to thank the people using Central and North West London NHS Foundation Trust (CNWL) services who gave quotes and shared their invaluable insights, including the staff and students of CNWL Recovery & Wellbeing College, CNWL peer support workers, peer researchers, carers, service leads and practitioners. We thank Jane Rennison and Steve Trenchard for their comments.
Reference
1. Knapp M, Andrew, A., McDaid, D., Iemmi, V., McCrone, P., Park, A., Parsonage, M., Boardman, J., Shepherd, G. Investing in recovery. London: Rethink Mental Illness 2014.
2. Slade M, Amering, M., Farkas, M., Hamilton, B., O’Hagan, M., Panther, G., Perkins, R., Shepherd, G., Tse, S., Whitley, R. . Uses and abuses of recovery: implementing recovery-oriented practices in mental health systems. World Psychiatry 2014;13:12-20.
3. World Health Organization. Mental Health Action Plan 2013-2020. Geneva: WHO 2013.
4. Shepherd G, Boardman J, Slade M. Making recovery a reality. Briefing Paper. London: Sainsbury Centre for Mental Health 2008.
5. Slade M. Personal Recovery and Mental Illness. Cambridge;: Cambridge University Press. 2009.
6. Perkins R, Repper J. Social Inclusion and Recovery. London: Bailliere Tindall 2003.
7. Leamy M, Bird V, Le Boutillier C, et al. A conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. Br J Psychiatry 2011;199:445-52.
8. Le Boutillier C, Leamy M, Bird VJ, et al. What does recovery mean in practice? A qualitative analysis of international recovery-oriented practice guidance. Psychiatr Serv 2011;62:1470-76.
9. Shepherd G, Boardman J, Burns M. Implementing Recovery. A methodology for organisation change. London: Sainsbury Centre for Mental Health 2010.
10. Piat M, Sabetti J, Fleury MJ, et al. “Who believes most in me and in my recovery”: the importance of families for persons with serious mental illness living in structured community housing. Journal of Social Work in Disability & Rehabilitation 2011;10(1):49-65.
11. Central and North West London NHS Foundation Trust. Shine 2014 Final report. Care bundles to improve physical healthcare in services for people with long-term mental health needs. London: Health Foundation 2015.
12. Rayner L, Matcham, F., Hutton, J., Stringer, C., Dobson, J., Steer, S., Hotopf, M. Embedding integrated mental health assessment and management in general hospital settings: feasibility, acceptability and the prevalence of common mental disorder. Gen Hosp Psychiatry 2014;36:318-24.
13. Whitley R. Ethno-Racial Variation in Recovery From Severe Mental Illness: A Qualitative Comparison. Canadian Journal of Psychiatry 2016;DOI: 10.1177/0706743716643740
14. Care Quality Commission. CQC’s response to the 2015 Community Mental Health Survey. London: Care Quality Commission 2016.
15. Bird V, Leamy, M., Le Boutillier, C., Williams, J., Slade, M. REFOCUS (2nd edition): Promoting recovery in mental health services. London: Rethink Mental Illness 2014.
16. Borg M, Kristiansen K. Recovery-oriented professionals: Helping relationships in mental health services. Journal of Mental Health 2004;13 493-505.
17. National Institute for Health and Clinical Excellence. Psychosis and schizophrenia in adults: treatment and management. NICE Clinical Guideline 178. London: NICE 2014.
18. Carkhuff R, Truax, C. Helping and Human Relations. Volume I: Selection and Training. New York: Holt, Rinehart & Winston 1969.
19. Carkhuff R, Truax, C. Helping and Human Relations. Volume II: Practice and Research. New York: Holt, Rinehart & Winston 1969.
20. Ljungberg A, Denhov, A., Topor, A. Nonhelpful relationships with professionals – a literature review of the perspective of persons with severe mental illness. Journal of Mental Health 2016;25:267-77.
21. Roberts G. Narrative and severe mental illness: what place do stories have in an evidence-based world?’. Advances in Psychiatric Treatment 2000;6:432-41.
22. Petros R, Solomon, P., Linz, S., DeCesaris, M., Hanrahan, M. Autovideography: The Lived Experience of Recovery for Adults with Serious Mental Illness. Psychiatric Quarterly 2016;87:417-26.
23. Tse S, Tsoi, E., Hamilton, B., O’Hagan, M., Shepherd, G., Slade, M., Whitley, R., Petrakis, M. Uses of Strength-Based Interventions for people with serious mental illness: A critical review. Int J Soc Psychiatry 2016;62:281-91.
24. Biringer E, Davidson, L., Sundfor, B., Ruud, T., Borg, M. Experiences of support in working toward personal recovery goals: a collaborative, qualitative study. BMC Psychiatry 2016;16:426.
25. Bora R, Leaning S, Moores A, et al. Life coaching for mental health recovery: the emerging practice of recovery coaching. Advances in Psychiatric Treatment 2010;16:459-67.
26. Moran G, Westman, K., Weissberg, E., Melamed, S. Perceived assistance in pursuing personal goals and personal recovery among mental health consumers across housing services. Psychiatry Res 2017;249:94-101.
27. Slade M, Bird, V., Clarke, E., Le Boutillier, C., McCrone, P., Macpherson, R., Pesola, F., Wallace, G., Williams, J., Leamy, M. . Supporting recovery in patients with psychosis using adult mental health teams (REFOCUS): a multi-site cluster randomised controlled trial. Lancet Psychiatry 2015;2:503-14.
28. Ejbye J, Holman, A. Making it happen. Practical learning and tips from the five Realising the Value local partner sites. London: NHS England 2016.
29. Schrank B, Bird V, Rudnick A, et al. Determinants, self-management strategies and interventions for hope in people with mental disorders: systematic search and narrative review. Soc Sci Med 2012;74:554-64.
30. Slade M. Implementing shared decision making in routine mental health care. World Psychiatry 2017;16:146-53.
31. Baker E, Fee, J., Bovingdon, L., Campbell, T., Hewis, E., Lewis, D., Mahoney, L., Roberts, G. From taking to using medication: recovery-focussed prescribing and medication management. Advances in Psychiatric Treatment 2013;19:2-10.
32. National Institute for Health and Clinical Excellence. Service user experience in adult mental health: improving the experience of care for people using adult NHS mental health services. CG136. London: National Institute for Health and Clinical Excellence 2011.
33. Henderson C, Flood C, Leese M, et al. Effect of joint crisis plans on use of compulsory treatment in psychiatry: single blind randomised controlled trial. BMJ 2004;329 136-40.
34. Henderson C, Flood C, Leese M, et al. Views of service users and providers on joint crisis plans: single blind randomized controlled trial. Soc Psychiatry Psychiatr Epidemiol 2009;44(5):369-76.
35. Thornicroft G, Farrelly, S., Szmukler, G., Birchwood, M., Waheed, W., Flach, C., Barrett, B., Byford, S., Henderson, C., Sutherby, K., Lester, H., Rose, D., Dunn, G., Leese, M., Marshall, M. Clinical outcomes of Joint Crisis Plans to reduce compulsory treatment for people with psychosis: a randomised controlled trial. Lancet 2013;381:1334-41.
36. Farrelly S, Lester, H., Rose, D., Birchwood, M., Marshall, M., Waheed, W., Henderson, C., Szmukler, G., Thornicroft, G. Barriers to shared decision making in mental health care: qualitative study of the Joint Crisis Plan for psychosis. Health Expectations 2015;19:448-58.
37. Health Foundation. Helping people help themselves. London: Health Foundation 2011.
38. Druss B, Zhao, L., von Esenwein, S., Bona, J., Fricks, L., Jenkins-Tucker, S., Sterling, E., Diclemente, R., Lorig, K. The Health and Recovery Peer (HARP) Program: a peer-led intervention to improve medical self-management for persons with serious mental illness. Schizophrenia Reseach 2010;118:264-70.
39. Seikkula J, Alakare, B., Aaltonen, J. The Comprehensive Open-Dialogue Approach in Western Lapland: II. Long-term stability of acute psychosis outcomes in advanced community care. Psychosis 2011;3:192- 204.
40. Health Foundation. Helping people share decision making. 2012
41. Jonk Y, Lawson K, O’Connor H, et al. How effective is health coaching in reducing health services expenditures? Medical care 2015;53(2):133-40. doi: 10.1097/ mlr.0000000000000287 [published Online First: 2015/01/15]
42. Harter M, Dirmaier J, Dwinger S, et al. Effectiveness of Telephone-Based Health Coaching for Patients with Chronic Conditions: A Randomised Controlled Trial. PloS one 2016;11(9):e0161269. doi: 10.1371/journal.pone.0161269 [published Online First: 2016/09/16]
43. Carter A, Tamkin P, Wilson S, et al. The Case for Health Coaching. Lessons learned from implementing a training and development intervention for clinicians across the East of England Brighton: Insitute for Employment Studies 2015.
44. Turner A, Anderson JK, Wallace LM, et al. An evaluation of a self-management program for patients with long-term conditions. Patient education and counseling 2015;98(2):213-9. doi: 10.1016/j.pec.2014.08.022 [published Online First: 2014/12/03]
45. Houle J, Gascon-Depatie M, BelangerDumontier G, et al. Depression selfmanagement support: a systematic review. Patient education and counseling 2013;91(3):271-9. doi: 10.1016/j. pec.2013.01.012 [published Online First: 2013/02/19]
46. Zoun MH, Koekkoek B, Sinnema H, et al. Effectiveness and cost-effectiveness of a self-management training for patients with chronic and treatment resistant anxiety or depressive disorders: design of a multicenter randomized controlled trial. BMC psychiatry 2016;16:216. doi: 10.1186/s12888-016-0927-1 [published Online First: 2016/07/09]
47. Flood C, Byford S, Henderson C, et al. Joint crisis plans for people with psychosis: economic evaluation of a randomised controlled trial. BMJ 2006;333(7571):729.
48. Barrett B, Waheed W, Farrelly S, et al. Randomised controlled trial of joint crisis plans to reduce compulsory treatment for people with psychosis: economic outcomes. PloS one 2013;8(11):e74210. doi: 10.1371/journal.pone.0074210 [published Online First: 2013/11/28]
49. Ruchlewska A, Wierdsma AI, Kamperman AM, et al. Effect of crisis plans on admissions and emergency visits: a randomized controlled trial. PloS one 2014;9(3):e91882. doi: 10.1371/journal. pone.0091882 [published Online First: 2014/03/22]
50. Griffiths CR, P. Recovery and Lifelong Learning: Interrelated Processes. International Journal of Psychosocial Rehabilitation 2008;13:51-56.
51. Marmot Review Team. Fair Society, Healthy Lives: Strategic review of health inequalities in England post-2010. London: Marmot Review Team 2010.
52. Commission on the Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health. Final report of the Commission on Social Determinants of Health. Geneva: World Health Organisation 2008.
53. Institute of Health Equity. Review of the Social Determinants and the Health Divide in the WHO European Region. Copenhagen: WHO Europe 2013.
54. Schuller T, Brasset-Grundy, A., Green, A., Hammond, C., Preston, J. Learning, Continuity and Change in Adult Life. Wider Benefits of Learning. Research Report No. 3. Nottingham: Centre for Research on the Wider Benefits of Learning 2002.
55. Jenkins A, Mostafa, T. . Learning and Wellbeing Trajectories Among Older Adults in England. London: Institute of Education 2013.
56. Lewis L. “You become a person again”: mental health and community learning. Birmingham: Worker’s Educational Association 2012.
57. Mental Health Foundation. Learning for life. Adult learning, mental health and wellbeing. London: Mental Health Foundation 2011.
58. Dolan P, Fujiwara D., Metcalfe, R. BIS Research Paper 90: Review and Update of Research into the Wider Benefits of Adult Learning. London: Department for Business, Innovation and Skills 2012.
59. Wilson S, Peterson, P. Theories of Learning and Teaching What Do They Mean for Educators? Best practices Working Paper. Washington DC: National Education Association 2006.
60. Repper J, Perkins R. ImROC Briefing Paper 6. The Team Recovery Implementation Plan: a framework for creating recovery-focused services. London: Centre for Mental Health 2013.
61. Vacher G. Utilising Team Recovery Implementation Plan (TRIP): embedding recovery-focused practice in rehabilitation services. Mental Health and Social Inclusion 2017;21:240-47.
62. Goodrich J. Schwartz Center Rounds. Evaluation of the UK pilots. London: King’s Fund 2011.
63. Alban-Metcalfe J, Alimo-Metcalfe, B. Engaging leadership part one: competencies are like Brighton Pier. International Journal of Leadership in Public Services 2009;5:10-18.
64. Perkins R, Repper, J., Rinaldi, M., Brown, H. ImROC 1. Recovery Colleges. London: Centre for Mental Health 2012.
65. Shepherd G, McGregor, J., Meddings, S., Roeg, W. Recovery Colleges and Co-production. In: Slade M, Oades, L., Jarden, A., ed. Wellbeing, Recovery and Mental Health. Cambridge: Cambridge University Press 2017.
66. McGregor J, Brophy., L., Hardy, D., Hoban, D., Meddings, S., Repper, J., Rinaldi, M., Roeg, W., Shepherd, G., Slade, M., Smelson, D., Stergiopoulos, V., RCICoP Group. Proceedings of June 2015 Meeting: Recovery Colleges International Community of Practice (RCICoP) 2016.
67. Rinaldi M, Suleman, M. Care coordinators attitudes to self-management and their experience of the use of the South West London Recovery College. London: South West London and St George’s Mental Health NHS Trust 2012.
68. Zabel E, Donegan , G., Lawrence, K., French, P. Exploring the impact of the recovery academy: a qualitative study of Recovery College experiences. Journal of Mental Health Training, Education and Practice 2016;11:162-71.
69. Meddings S, Campbell, E., Guglietti, S., Lambe, H., Locks, L., Byrne, D., Whittington, A. From service user to student: the benefits of Recovery Colleges. Clinical Psychology Forum 2015;268:32-37.
70. Rinaldi M, Wybourn, S. The Recovery College Pilot in Merton and Sutton: longer term individual and service level outcomes. London: South West London and St. Georges Mental Health NHS Trust 2011.
71. Taggart H, Kempton, J. The route to employment: the role of mental health recovery colleges. London: CentreForum 2015.
72. McCaig M, McNay, L., Marland, G., Bradstreet, S., Campbell, J. Establishing a recovery college in a Scottish University. Mental Health and Social Inclusion 2014;18:92-97.
73. Meddings S, Byrne, D., Barnicoat, S., Campbell, E., Locks, L. Co-Delivered and Co–Produced: Creating a Recovery College in Partnership. Journal of Mental Health Training, Education and Practice 2014;9:16-25.
74. Rennison J, Skinner, S., Bailey, A. CNWL Recovery College Annual Report April 2013 – March 2014. London: Central and North West London NHS Foundation Trust 2014.
75. Zucchelli F, Skinner, S. Central and North West London NHS Foundation Trust’s (CNWL) Recovery College: the story so far… Mental Health and Social Inclusion 2014;17:183-89.
76. Shepherd G, Boardman, J., Rinaldi, M., Roberts, G. ImROC Briefing paper 8. Supporting recovery in mental health services: Quality and Outcomes. London: Implementing Recovery through Organisational Change 2014.
77. McGregor J, Repper, J., Brown, H. “The college is so different from anything I have done”. A study of the characteristics of Nottingham Recovery College. Journal of Mental Health Training, Education and Practice 2014;9:3-15.
78. Bourne P, Meddings S, Whittington A. An evaluation of service use outcomes in a recovery college. . Journal of Mental Health forthcoming
79. Rinaldi M, Marland M, Wybourn S. Annual Report 2011 – 2012. South West London Recovery College. London: South West London and St George’s Mental Health Trust 2012.
80. Burhouse A, Rowland M, Marie Niman H, et al. Coaching for recovery: a quality improvement project in mental healthcare. BMJ quality improvement reports 2015;4(1) doi: 10.1136/bmjquality. u206576.w2641 [published Online First: 2016/01/07]
81. Whitley R, Gingerich, S., Lutz, W., Mueser, K. Implementing the Illness Management and Recovery Program in Community Mental Health Settings: Facilitators and Barriers. Psychiatr Serv 2009;60:202-09.
82. Leamy M, Clarke, E., Le Boutillier, C., Bird, V., Janosik, M., Sabas, K., Riley, G., Williams, J., Slade, M. Implementing a complex intervention to support personal recovery: A qualitative study nested within a cluster randomised controlled trial. PLoS One 2014;9:e97091.
83. Dixon-Woods M, Baker, R., Charles, K., Dawson, J., Jerzembek, G., Martin, G. McCarthy, I., McKee, L., Minion, J., Ozieranski, P., Willars, J., Wilkie, P., West, M. Culture and behaviour in the English National Health Service: overview of lessons from a large multimethod study. BMJ Quality and Safety 2014;23:106-15.
84. Slade M. Measuring recovery in mental health services. Israel Journal of Psychiatry 2010;47(3):206-12.
85. Le Boutillier C, Slade, M., Lawrence, V., Bird, V., Chandler, R., Farkas, M., Harding, C., Larsen, J., Oades, L., Roberts, G., Shepherd, G., Thornicroft, G., Williams, J., Leamy, M.,. Competing priorities: staff perspectives on supporting recovery. Administration and Policy in Mental Health and Mental Health Services Research 2015;42:429-38.
86. Le Boutillier C, Chevalier, A., Lawrence, V., Leamy, M., Bird, V., Macpherson, R., Williams, J., Slade, M. . Staff understanding of recovery-orientated mental health practice: a systematic review and narrative synthesis. Implementation Science 2015;10:87.
87. Mental Health “Recovery” Study Working Group. Mental Health “Recovery”: Users and Refusers. Toronto: Wellesley Institute 2009.
88. Chester P, Ehrlich, C., Warburton, L., Baker, D., Kendall, E., Crompton, D. What is the work of Recovery Oriented Practice? A systematic literature review. International Journal of Mental Health Nursing 2016;25:270-85.
89. Maben J, Peccei, R., Adams, M., Robert, G., Richardson, A., Murrells, T., Morrow, E. Exploring the relationship between patients’ experiences of care and the influence of staff motivation, affect and wellbeing. Final report: NIHR Service Delivery and Organisation programme 2012.
90. West M, Eckert, R., Steward, K., Pasmore, B. Developing collective leadership for health care. London: King’s Fund 2014.
91. West M, Eckert, R., Collins, B., Chowla, R. Caring to change How compassionate leadership can stimulate innovation in health care. London: King’s Fund 2017.
92. Simpson A, Hannigan, B., Coffey, M., Barlow, S., Cohen, R., Jones, A., Všetečková, J., Faulkner, A., Thornton, A., Cartwright, M. Recovery-focused care planning and coordination in England and Wales: a cross-national mixed methods comparative case study. BMC Psychiatry 2016;16:147.
93. Copeland ME. Wellness Recovery Action Plan. Brattleboro: VT Peach Press 1999.
94. Sheldon KM, Williams G, Joiner T. SelfDetermination Theory in the Clinic: Motivating Physical and Mental Health. New Haven Yale University Press 2003.
95. Smith-Merry J, Freeman, R., Sturdy, S. Implementing recovery: an analysis of the key technologies in Scotland. International Journal of Mental Health Systems 2011;5:11.
96. Cook JA, Copeland ME, Jonikas JA, et al. Results of a randomized controlled trial of mental illness self-management using Wellness Recovery Action Planning. Schizophr Bull 2012;38(4):881-91.
97. Cook JA, Jonikas JA, Hamilton MM, et al. Impact of Wellness Recovery Action Planning on service utilization and need in a randomized controlled trial. Psychiatr Rehabil J 2013;36(4):250-7. doi: 10.1037/ prj0000028 [published Online First: 2013/12/11]
98. Horan L, Fox J. Individual perspectives on the Wellness Recovery Action Plan (WRAP) as an intervention in mental health care. International Journal of Psychosocial Rehabilitation 2016;20(2):110-25.
99. Langan J. Challenging assumptions about risk factors and the role of screening for violence risk in the field of mental health. Health, Risk & Society 2010;12:85-100.
100. Sykes M, Brabban, A., Reilly, J. Balancing harms in support of recovery. Journal of Mental Health 2015;24:140- 44.
101. Felton A, Wright, N., Stacey, G. Therapeutic risk-taking: a justifiable choice. BJPsych Advances 2017;23:81- 88.
102. Department of Health. Independence, Choice and Risk: A Guide to Best Practice in Supported Decision Making. London: Department of Health 2007.
103. Mulder R, Netwon-Howes, G., Coid, J. The futility of risk prediction in psychiatry. Br J Psychiatry 2016;209:271-72.
104. Boardman J, Roberts, G. Risk, Safety and Recovery. ImROC Briefing Paper 9. London: Centre for Mental Health 2014.
105. Huckshorn K. Reducing the use of seclusion and restraint in mental health systems: A public health prevention approach with interventions. J Psychosoc Nurs Ment Health Serv 2004;42:22–33.
106. Huckshorn K. Re-designing State mental health policy to prevent the use of seclusion and restraint. Adm Policy Ment Health 2006;33:482– 91.
107. Substance Abuse and Mental Health Services Administration. Promoting alternatives to the Use of Seclusion and Restraint. Issue Brief #1. [Download at https://www.samhsa.gov/sites/default/ files/topics/trauma_and_violence/ seclusion-restraints-1.pdf]. Rockville, Maryland: SAMHSA 2010.
108. Substance Abuse and Mental Health Services Administration. Promoting alternatives to the Use of Seclusion and Restraint. Issue Brief #21. Rockville, Maryland: SAMHSA 2010.
109. Ashcraft L, Bloss, M., Anthony, W. The Development and Implementation of “No Force First” as a Best Practice. Psychiatr Serv 2012;63:415-17.
110. NHS Improvement. Developing a noforce culture to improve quality and safety on mental health wards. London: NHS Improvement 2016.
111. Positive Practice. No Force First – Mersey Care NHS Foundation Trust. Available at http:// positivepracticemhdirectory.org/adults/ no-force-first/ 2017 [
112. Putkonen A, Kuivalainen, S., Louheranta, O., Repo-Tiihonen, E., Ryynänen, O.-P., Kautiainen, H., Tiihonen, J. ClusterRandomized Controlled Trial of Reducing Seclusion and Restraint in Secured Care of Men With Schizophrenia. Psychiatr Serv 2013;64:850-55.
113. Guzman-Parra J, Aguilera Serrano, C., García-Sánchez, J., Pino-Benítez, I., Alba-Vallejo, M., Moreno-Küstner, B., Mayoral-Cleries, F. Effectiveness of a Multimodal Intervention Program for Restraint Prevention in an Acute Spanish Psychiatric Ward. Journal of the American Psychiatric Nurses Association 2016;22:233-41.
114. Chan J, LeBel J, Webber L. The dollars and sense of restraints and seclusion. Journal of law and medicine 2012;20(1):73-81. [published Online First: 2012/11/20]
115. Rubio-Valera M, Luciano JV, Ortiz JM, et al. Health service use and costs associated with aggressiveness or agitation and containment in adult psychiatric care: a systematic review of the evidence. BMC psychiatry 2015;15:35. doi: 10.1186/s12888- 015-0417-x [published Online First: 2015/04/17]
116. Serrano-Blanco A, Rubio-Valera M, Aznar-Lou I, et al. In-patient costs of agitation and containment in a mental health catchment area. BMC psychiatry 2017;17(1):212. doi: 10.1186/s12888- 017-1373-4 [published Online First: 2017/06/07]
117. Flood C, Bowers L, Parkin D. Estimating the costs of conflict and containment on adult acute inpatient psychiatric wards. Nursing economic$ 2008;26(5):325-30, 24. [published Online First: 2008/11/05]
118. LeBel J. The Business Case for Preventing and Reducing Restraint and Seclusion Use. HHS Publication No. (SMA) 11-4632. Rockville, MD: Substance Abuse and Mental Health Services Administration 2011.
119. Taylor-Watt J, Cruickshank A, Innes J, et al. Reducing physical violence and developing a safety culture across wards in East London. British Journal of Mental Health Nursing 2017;6(1):35-43.
120. Lebel J, Goldstein R. The economic cost of using restraint and the value added by restraint reduction or elimination. Psychiatric services 2005;56(9):1109- 14. doi: 10.1176/appi.ps.56.9.1109 [published Online First: 2005/09/09]
121. Putkonen A, Kuivalainen S, Louheranta O, et al. Cluster-randomized controlled trial of reducing seclusion and restraint in secured care of men with schizophrenia. Psychiatric services 2013;64(9):850- 5. doi: 10.1176/appi.ps.201200393 [published Online First: 2013/06/19]
122. Boyle D, Harris M. The challenge of co-production. London: new economics foundation 2009.
123. Nesta. People powered health coproduction catalogue. London: Nesta 2012.
124. Slay J, Stephens, L. Co-production in mental health: A literature review. London: new economics foundation 2013.
125. Wallace L, Turner, A., KosmalaAnderson, J., Sharma, S., Jesuthasan, J., Bourne, C., Realpe, A. Co-creating Health: Evaluation of first phase. London: Health Foundation 2012.
126. Newbronner L, Chamberlain, R., Borthwick, R., Baxter, D., Sanderson, D. Sustaining and spreading selfmanagement support: Lessons from Cocreating Health phase 2. London: Health Foundation 2013.
127. Bradley P, Willson, A. Achieving prudent healthcare in NHS Wales (revised). Cardiff: Public Health Wales 2014.
128. Loeffler E, Power, G., Bovaird, T., HineHughes, F. Co-Production of Health and Wellbeing in Scotland. Birmingham: Governance International 2013.
129. Needham C. Co-production: an emerging evidence base for adult social care transformation. Social Care Institute for Excellence: London 2009.
130. McDaid D, Park A-L. Side by Side. Economic analysis. London: MIND, 2017.
131. Mead S, Hilton, D., Curtis, L. Peer support: A theoretical perspective. Psychiatric Rehabilitation Journal 2001;25:134–41.
132. Davidson L, Bellamy, C., Guy, K., Miller, R. Peer support among persons with severe mental illnesses: a review of evidence and experience. World Psychiatry 2012;11:123-28.
133. Pitt V, Lowe D, Hill S, et al. Consumerproviders of care for adult clients of statutory mental health services. Cochrane Database of Systematic Reviews 2013(3) doi: Artn Cd004807 Doi 10.1002/14651858.Cd004807.Pub2
134. Warner R. Recovery from schizophrenia and the recovery model. Current Opinion in Psychiatry 2009;22:374-80.
135. Repper J, Carter T. A review of the literature on peer support in mental health services. Journal of Mental Health 2011;20(4):392-411.
136. Shepherd G, Repper, J. Empowerment and Inclusion: The Introduction of Peer Workers into the Workforce. In: Gaebel W, Rossler, W., Sartorius, N., ed. The Stigma of Mental Illness – End of the Story? Switzerland: Springer International Publishing 2016:591-612.
137. Repper J. ImROC Briefing Paper 5. Peer Support Workers: Theory and Practice. London: Centre for Mental Health 2013.
138. Repper J. ImROC Briefing Paper 7. Peer Support Workers: a practical guide to implementation. London: Centre for Mental Health 2013.
139. Chinman M, Henze, K., Sweeney, P. Implementing Peer Support Services in VHA. Pittsburgh: VA Pittsburgh Healthcare System 2013.
140. Sunderland K. Guidelines for the Practice and Training of Peer Support. Ottawa: Mental Health Commission of Canada 2013.
141. Henderson C, Noblett, J., Parke, H., Clement, S., Caffrey, A., Gale-Grant, O., Schulze, B., Druss, B., Thornicroft, G. Mental health-related stigma in health care and mental health-care settings. Lancet Psychiatry 2014;1:467-82.
142. Thornicroft G. Shunned: Discrimination against People with Mental Illness. Oxford: Oxford University Press 2005.
143. Dixon L, Hackman, A., Lehman, A. Consumers as Staff in Assertive Community Treatment Programs. Administration and Policy in Mental Health and Mental Health Services Research 1997;25:199-208.
144. Knaak S, Modgill, G., Patten, S. Key Ingredients of Anti-Stigma Programs for Health Care Providers: A Data Synthesis of Evaluative Studies. Canadian Journal of Psychiatry 2014;59:S19-S26.
145. Trachtenberg M, Parsonage M, Shepherd G, et al. Peer support in mental health care: is it good value for money? London Centre for Mental Health 2013.
146. PPL. Impact and cost: Summary of the economic modelling tool for commissioners. London: PPL 2016.
147. Sledge WH, Lawless M, Sells D, et al. Effectiveness of peer support in reducing readmissions of persons with multiple psychiatric hospitalizations. Psychiatric services 2011;62(5):541-4. doi: 10.1176/ ps.62.5.pss6205_0541 [published Online First: 2011/05/03]
148. Simpson A, Flood C, Rowe J, et al. Results of a pilot randomised controlled trial to measure the clinical and cost effectiveness of peer support in increasing hope and quality of life in mental health patients discharged from hospital in the UK. BMC psychiatry 2014;14:30. doi: 10.1186/1471-244X-14- 30 [published Online First: 2014/02/06]
149. Yoon J, Lo J, Gehlert E, et al. Homeless Veterans’ Use of Peer Mentors and Effects on Costs and Utilization in VA Clinics. Psychiatric services 2017;68(6):628-31. doi: 10.1176/appi. ps.201600290 [published Online First: 2017/02/02]
150. Leamy M, Clarke, E., Le Boutillier, C., Bird, V., Choudhury, R., Macpherson, R., Pesola, P., Sanger, K., Williams, J., Williams, P., Slade, M. A national survey of recovery practice in community mental health teams. Br J Psychiatry 2016;209:340-46.
151. Walker L, Perkins, R., Repper, J. Creating a recovery focused workforce: supporting staff well-being and valuing the expertise of lived experience. Mental Health and Social Inclusion 2016;18:133-41.
152. Schrank B, Brownell, T., Riches, S., Chevalier, A., Jakaite, Z., Larkin, C., Lawrence, V., Slade, M. Staff views on wellbeing for themselves and for service users. Journal of Mental Health 2015;24:48-53.
153. Foresight Mental Capital Wellbeing Project. Mental Capital and Wellbeing: Making the most of ourselves in the 21st century. Final Project Report. London: Government Office for Science 2008.
154. Aked J, Marks, N., Cordon, C., Thompson, S. Five Ways to Wellbeing: The Evidence. London: New Economics Foundation 2008.
155. Slade M, Oades, L., Jarden, A., editor. Wellbeing, Recovery and Mental Health. Cambridge: Cambridge University Press, 2017.
156. Joyce S, Modini, M., Christensen, H., Mykletun, A., Bryant, R., Mitchell, P., Harvey S. Workplace interventions for common mental disorders: a systematic meta-review. Psychol Med 2016;46:683- 97.
157. CSA Group, Bureau de normalisation du Quebec. Psychological health and safety in the workplace — Prevention, promotion, and guidance to staged implementation. Ottawa: Mental Health Commission of Canada 2013.
158. National Institute for Health and Clinical Excellence. Mental wellbeing at work. London: NICE 2009.
159. Health and Safety Executive. How to tackle work-related stress. A guide for employers on making the Management Standards work London: HSE 2009.
160. McDaid D, Park AL. Investing in wellbeing in the workplace: more than just a business case. In: McDaid D, Cooper C, eds. Economics of wellbeing. Oxford, UK: Wiley-Blackwell 2014:215- 38.
161. Boardman J. More than shelter. Supported accomodation and mental health. London: Centre for Mental Health 2016.
162. Stergiopoulos V, Hwang, S., Gozdzik, A., Nisenbaum, R., Latimer, E., Rabouin, D., Adair, C., Bourque, J., Connelly, J., Frankish, J., Katz, L., Mason, K., Misir, V., O’Brien, K., Sareen, J., Schutz, C., Singer, A., Streiner, D., Vasiliadis, H., Goering, P. Effect of Scattered-Site Housing Using Rent Supplements and Intensive Case Management on Housing Stability Among Homeless Adults With Mental Illness. A Randomized Trial. Journal of the American Medical Association 2015;313(9):A905.
163. Kirst M, Zerger, S., Harris, D., Plenert, E., Stergiopoulos, V. The promise of recovery: narratives of hope among homeless individuals with mental illness participating in a Housing First randomised controlled trial in Toronto, Canada. BMJ Open 2014;4:e004379.
164. Shelter. Good practice briefing: Housing first. London: Shelter 2008.
165. Kinoshita Y, Furukawa, T., Kinoshita, K., Honyashiki, M., Omori, I., Marshall, M., Bond, G., Huxley, P., Amano, N., Kingdon D. Supported employment for adults with severe mental illness. Cochrane Database of Systematic Reviews 2013;9:CD008297.
166. Howard L, Heslin, M., Leese, M., McCrone, P., Rice, C., Jarrett, M., Spokes, T. Supported employment: randomised controlled trial. Br J Psychiatry 2010;196:404-11.
167. Latimer E. An effective intervention delivered at sub-therapeutic dose becomes an ineffective intervention. Br J Psychiatry 2010;196:341-42.
168. Modini M, Tan L, Brinchmann B, et al. Supported employment for people with severe mental illness: systematic review and meta-analysis of the international evidence. The British journal of psychiatry : the journal of mental science 2016;209(1):14-22. doi: 10.1192/bjp. bp.115.165092 [published Online First: 2016/04/23]
169. Killackey E, Allott K, Woodhead G, et al. Individual placement and support, supported education in young people with mental illness : an exploratory feasibility study. Early intervention in psychiatry 2016 (early online publication)
170. Kahneman D, Deaton, A. High income improves evaluation of life but not emotional well-being. Proceedings of the National Academy of Sciences 2010;107:16489-93.
171. Psychologists for Social Change. Universal Basic Income: A Psychological Impact Assessment. London: PAA 2017.
172. McGrath L, Griffin, V., Mundy, E. The psychological impact of austerity: Psychologists Against Austerity 2016.
173. Cook J, Russell, C., Grey, D., Jonikas, J. A Self-Directed Care Model for Mental Health Recovery. Psychiatr Serv 2008;59:600-03.
174. Alakeson V, Perkins, R. ImROC Briefing Paper 2. Recovery, Personalisation and Personal Budgets. London: Centre for Mental Health 2012.
175. Hamilton S, Tew, J., Szymczynska, P., Clewett, N., Manthorpe, J., Larsen, J., Pinfold, V. Power, Choice and Control: How Do Personal Budgets Affect the Experiences of People with Mental Health Problems and Their Relationships with Social Workers and Other Practitioners? British Journal of Social Work 2016;46:719-36.
176. Pinfold V, Sweet, D., Porter, I., Quinn, C., Byng, R., Griffiths, C., Billsborough, J., Enki, D., Chandler, R., Webber, M., Larsen, J., Carpenter, J., Huxley, P. Improving community health networks for people with severe mental illness: a case study investigation. Health Services and Delivery Research 2015;3:1-236.
177. Topor A, Borg M, Mezzina R, et al. Others: The Role of Family, Friends, and Professionals in the Recovery Process. American Journal of Psychiatric Rehabilitation 2006;9:17-37.
178. Schön UK, Denhov A, Topor A. Social relationships as a decisive factor in recovering from severe mental illness. Int J Soc Psychiatry 2009;55:336-47.
179. Pinfold V, Sweet, D. Wellbeing networks and asset mapping. London: McPin Foundation 2015.
180. One Housing. A success story – Integration at Tile House. Available at http://www.onehousing.co.uk/work-withus/housing-care-and-support/workingwith-the-nhs. London: One Housing 2016.
181. Ly A, Latimer E. Housing First Impact on Costs and Associated Cost Offsets: A Review of the Literature. Canadian journal of psychiatry Revue canadienne de psychiatrie 2015;60(11):475-87. [published Online First: 2016/01/01]
182. City of Toronto. .What Housing First Means for People: Results of Streets to Homes 2007 Post-Occupancy Research. . Toronto: City of Toronto, Shelter and Housing Administration. 2007.
183. Bretherton J, Please N. Housing First in England. An Evaluation of Nine Services. York: University of York 2015.
184. Killaspy H, Priebe S, Bremner S, et al. Quality of life, autonomy, satisfaction, and costs associated with mental health supported accommodation services in England: a national survey. The lancet Psychiatry 2016;3(12):1129-37. doi: 10.1016/s2215-0366(16)30327-3 [published Online First: 2016/10/25]
185. Drake RE, Bond GR, Goldman HH, et al. Individual Placement And Support Services Boost Employment For People With Serious Mental Illnesses, But Funding Is Lacking. Health affairs (Project Hope) 2016;35(6):1098- 105. doi: 10.1377/hlthaff.2016.0001 [published Online First: 2016/06/09]
186. Hoffmann H, Jackel D, Glauser S, et al. Long-term effectiveness of supported employment: 5-year followup of a randomized controlled trial. The American journal of psychiatry 2014;171(11):1183-90. doi: 10.1176/ appi.ajp.2014.13070857 [published Online First: 2014/08/16]
187. Parsonage M, Grant C, Stubbs J. Priorities for mental health: Economic report for the NHS England Mental Health Taskforce. London: Centre for Mental Health 2016.
188. Knapp M, Patel A, Curran C, et al. Supported employment: costeffectiveness across six European sites. World psychiatry : official journal of the World Psychiatric Association 2013;12(1):60-8. doi: 10.1002/ wps.20017 [published Online First: 2013/03/09]
189. Yamaguchi S, Sato S, Horio N, et al. Cost-effectiveness of cognitive remediation and supported employment for people with mental illness: a randomized controlled trial. Psychol Med 2017;47(1):53-65. doi: 10.1017/ s0033291716002063 [published Online First: 2016/09/23]
190. Webber M, Treacy S, Carr S, et al. The effectiveness of personal budgets for people with mental health problems: A systematic review. Journal of Mental Health 2014;23(3):146-55.
191. Jones K, Forder J, Caiels J, et al. Personalization in the health care system: do personal health budgets have an impact on outcomes and cost? Journal of health services research & policy 2013;18(2 Suppl):59-67. doi: 10.1177/1355819613503152 [published Online First: 2013/09/21]
192. NHS England. Integrated Personal Commissioning (IPC). https://www. england.nhs.uk/ipc/2017.
193. Parsonage M. Welfare advice for people who use mental health services. London Centre for Mental Health 2013.
194. Acton R. The missing link. How tackling financial difficulty can boost recovery rates in IAPT. London: Money and Mental Health Institute 2016.
195. McDaid D, Park A-L, Knapp M. Commissioning Cost-Effective Services for Promotion of Mental Health and Wellbeing and Prevention of Mental Ill Health. London: Public Health England 2017.
Coproduction is a term we frequently hear and use. If we stop to examine the way we work in every interaction and every conversation, do we truly recognise everyone’s assets, engage in mutually respectful and beneficial relationships and actively endeavour to reduce traditional power imbalances? Co-production – Sharing Our Experiences, Reflecting on Our Learning is our way of contributing to the discussion on what coproduction is from our perspective. We have also outlined Top Ten Tips for Coproduction on page 19 to offer some practical points to keep in mind.
“As we collated narrative accounts, and reflected on our learning over the last 7 years, it became clear that new ideas, opportunities and passion arise consistently from experiences of co-production on the ground. At a time when services are very stretched and conventional problem-solving approaches are outdated, working together as equals becomes a powerful force for connection and improvement. It reignites hope and humanity, and embraces talents and energies that have previously been disregarded.” Anna Lewis, Lead Author & ImROC Senior Consultant.
Download 13. Co-production – Sharing Our Experiences, Reflecting on Our Learning
13. Co-production – Sharing Our Experiences, Reflecting on Our Learning
Anna Lewis, Toni King, Lesley Herbert and Julie Repper
INTRODUCTION
There can be little doubt that the term ‘coproduction’ has a growing profile in public services, and particularly within the mental health sector. Look at any conference programme, recent policy document, training event or even your Twitter feed, and it is likely that you will find mention of it. It features in the Five Year Forward View for Mental Health (2016), Prudent Health Care for Wales (Bradley & Willson 2014), the Scottish CoProduction Network and Learn to Lead in schools (Frost & Stenton 2010). The NHS is talking about it. Local Government is talking about it. Education is talking about it. Many have been working diligently and authentically to do it over many years. Others are just embarking on their journey and may feel overwhelmed by the challenges lying ahead.
So what is ‘it’ and why does it matter? Coproduction offers a unique approach through which to interpret and address the challenges faced in our communities. It opens up opportunities we haven’t yet spotted. It represents something fundamentally different in the way that relationships between services and communities are understood and developed. And yet this has not happened suddenly or dramatically. Slowly, people, communities, partnerships, groups are responding to shared challenges by evolving new ways of problem solving together.
The principles and values which have guided ImROC’s work from inception are built around recovery and co-production. In every aspect of our mission, we continue to amass experience and learning by working in partnerships that both facilitate and value the contribution that every individual makes. In this paper, we attempt to bring co-production to life through a series of case studies of collaborative work undertaken with ImROC. Our intention is to curate a space in which narrative accounts are shared. We do not seek to critique the experiences – they are recounted just as they were told to the authors of the paper. Instead we seek to draw out common themes and explore their relevance to others, so that we all learn and strengthen our efforts to work more effectively amongst our communities.
The case studies are not unique, yet each represents something extraordinary and special and new for those involved in them. They illustrate the reality, the value, the challenges and the learning that we continue to gain in every aspect of our work. They allow us to explore the themes that characterise the work, and think about our aspirations for the future. They give us hope in turbulent times.
Intentionally, we have not examined at length the theoretical basis or principles for coproduction. That has been ably achieved by many before us, not least Cahn (2001), Ostrom (1996), NEF (Stephens, Ryan-Collins & Boyle 2008), NESTA (Boyle & Harris 2009) and more. Here we provide the theory only to the extent that is necessary to contextualise the case studies. We work on the basis that authentic co-production is something for which we strive, in which we make mistakes as well as strides. We hope that these real life examples will inspire others to try too.
The Wider Context
While the notion of co-production aligns so naturally with the strengths-based, lifeoriented ideas around personal recovery, its origins lie well beyond the mental health arena. Boyle, Slay & Stephens (2011) set out the wider context in which co-production has evolved, citing issues such as escalating demand for public services, advances in technology, and the changing nature of family networks, approaches to which are bound up in the mindset of the deficits-based welfare economy. The scope of these approaches to nurture health and wellbeing in communities is largely exhausted. Co-production seeks to re-imagine a future in which other resources, hitherto overlooked and untapped, are identified, valued and utilised.
The scope for this real change lies in the ‘core economy’ (Cahn 2001) of family, friends and neighbours – those individuals who make up each local community. It is this unseen & unrecognised context that determines the impact of every public service over time. The infinite talents and resources of those for whom public services exist are largely overlooked, diminished by the professional tendency to see what’s wrong, not what’s strong, alongside the unconscious willingness of participants to slip into a passive role as recipients of services. Yet it is likely that any future state-funded health and social care provision will rely on this hidden capacity and capability to thrive, and it will need to reframe its own role and relationship with this untapped and rich resource.
Some will feel pulled towards the valuesbased reasons for a vision for co-production. Others may feel pushed towards that vision because other more traditional options are rapidly rendered redundant. Whether an idealist or a pragmatist, there is something within co-production that offers hope and opportunity.
So What Does Co-Production Mean to Us in ImROC?
One of the difficulties that besets our field of work, and many others, is the ease with which accessible language and terminology can be picked up, used and abused. One person’s shorthand is another person’s source of confusion, disagreement or even indignation. Ideas borne out of mutual appreciation and belief in the potential and power of people have been overtaken by less laudable agendas, often driven by powerful players such as large organisations or government. We encounter this in relation to recovery. Whilst the appeal of co-production tends to grow when times are tough, it too easily becomes conflated with the politics of austerity and cuts (Bovaird, 2007). How easy it is to re-label an existing activity or approach, acquiring the new language and outward expression, yet missing the opportunity to reflect honestly upon its challenges and internalise a fundamentally different vision for the future.
Hence finding a single definition of coproduction to act as a benchmark for authenticity & fidelity feels less important than being able to articulate a set of principles that have common meaning, are easily accessible, and act as a guiding light for those treading the path of co-production. In turn, these principles are interpreted and brought to life by those most involved within the unique context of each activity, goal or set of assets. Like recovery, co-production is a personal experience and one best understood through the shared narrative that evolves when people find ways of working together towards new solutions.
Within ImROC we have come to this realisation over a period of time, as our understanding and experience have evolved and our willingness to test out new ideas has grown. We value this discovery as an important aspect of the process of our own co-production journey, and one we would not choose to leapfrog if we had our time again. Experiencing co-production first hand is at the heart of that process of internalisation and authenticity.
We first defined the principles which underpin our ImROC approach in our briefing paper The Team Recovery Implementation Plan: a framework for creating recovery-focused services (Repper and Perkins) in 2013. These are drawn from the literature, including Cahn (2001), Boyle et al. (2010), Slay et al (2013).
- We recognise people as having human assets, strengths, resources and networks that reach beyond the labels we use to describe their ‘position’ within a system or hierarchy.
- We build mutual and reciprocal relationships in which expertise is recognised amongst all parties, no longer the exclusive domain of the professional. Looking beyond these conventional labels, we strive to break down barriers, blur boundaries, share responsibility in both the design, delivery and improvement of services.
- We nurture and mobilise peer, personal and professional networks around a diverse community of interest, in order to share learning, build understanding, generate ideas and explore possibilities.
- We seek to catalyse change, and we have that vision for services too. We believe that it is for the individual to define and lead their journey, with services acting as supporters and facilitators of resources, expertise and networks that help both in the short and longer term.
Those core principles characterise transformative co-production across the globe, and bind us together with the efforts of thousands of others who have a vision for a fairer and more inclusive world in which all talents are valued and nurtured. Coproduction is appreciative, collaborative, respectful and active. It is based on a belief that every one of us has something to offer for the greater good. It goes hand in hand with the values of recovery by locating both problems and solutions within a shared rather than individual context, and it facilitates personal agency.
Power Play
These principles, brought to life through collaborative effort, form the foundations of coproduction. However, there is one more essential factor in relation to co-productive impact. That relates to power. More specifically, the re-distribution of decision-making power within the relationship between provider and consumer, professional and person with lived experience of mental health conditions, practitioner and client. Three levels of co-production have been identified (Needham & Carr, 2009) – descriptive, intermediate and transformative. It is the balance of power between professionals and patient (sic) that determines and defines each of these levels, and it is the transformative potential of co-production on which ImROC is focused. We return to the theme of power later in the paper.
Policy Vs Practice
So what of the practice in healthcare? Is this a passing fad? Is it really starting to happen?
The terminology is straightforward enough to adopt. The reality – changing the conversation, sharing power, recognising the limits of professional expertise, embracing diverse experiences and views, developing a shared narrative, and blurring the boundaries between those who provide and those who use services, and doing all of this through good times and bad – is as challenging as it is rewarding. Rarely does it slot harmoniously into well-established organisational practice and beliefs, which tend to be rooted in a deference towards professional status, knowledge and expertise, passivity and even gratitude. Rather, it unravels the order of things at a time of unpredictability and change when we all crave some kind of stability. Adding yet another layer of uncertainty, asking for some professional ‘letting go’ to happen when so much is already beyond our control feels as if it is too great a leap. Familiar chaos seems preferable to the unfamiliar, even if that does offer the possibility of something better. Despite ample good intention, co-production in public services, consistently, competently and committedly deployed to its full transformative potential, remains an aspiration for most of us.
Yet mental health communities across the UK and beyond are rising to this challenge and leading the way. The following case studies have been put together by people who are striving to co-produce in their local area, working within their local context. While we want to celebrate the good practice and commitment that the case studies represent, that is not our main aim in sharing them. Instead, we seek to illustrate the wide range of possibilities and challenges that co-production presents in real and living ways. The accounts that the authors share are about the realities of working differently, working against the prevailing norm, re-setting values and focus, unlearning and relearning. In current organisational language, being ‘disruptive’. As in recovery, there is no end point. We value the journey and what we have yet to discover. This spirit of adventure and curiosity is at the heart of any co-production effort.
The case studies are broadly grouped according to scale, ranging from team to system-wide levels. As you read them, it may be helpful to reflect on the scale of the impact that each is having, and in particular the extent to which power is distributed amongst the people involved.
We begin by exploring a contentious issue about the feasibility of co-production at an individual level.
Can you co-produce within individual work?
In the development of this paper, a debate emerged amongst the authors about whether co-production could take place within a therapeutic relationship between two people.
Many practitioners work in a person-centred and collaborative way during 1:1 sessions in their day to day practice. Those with recovery principles at the core of their work will be used to drawing on strengths, building hopes and shared solutions. Co-production may sound like business as usual. SCIE (2013) describes this as a descriptive level of coproduction. Here, at a minimum, there is a degree of collaboration in order to achieve an outcome for the person in receipt of the service, and at its most successful, individuals are engaged in an active role or leading their own recovery.
Yet in our own work we all experienced ‘co-production’ at an individual level as very different from co-production at a group level. This led us to ask – is this really co-production? There are three theoretical principles which highlight why this may be debated.
- Cahn’s original work identifies the development of social capital as a primary outcome of co-production. It creates a community in which “people are valued for their contributions and discover they can rely on one another” (Rowe 1997). In this way, the outcome of co-production is of benefit to more people than those directly involved.In comparison, it might be argued that in a typical therapeutic encounter, the goals will focus on resolving problems and generating solutions for the individual. Certainly, this would have been the case in traditional psychiatry services. However, in a recovery-focused relationship, aspirations are not limited to symptom reduction but to the development of contributing roles and valued relationships within communities – thus increasing social capital.
- The principle of reciprocity and mutuality is essential in co-production. All involved will learn and create something together which could not be discovered or achieved individually. The experience of sparking off one another, someone else’s viewpoint revealing new truths and options and this being equally shared regardless of status, health or training. It might be argued that the limited nature of a relationship involving only two parties can hinder this possibility. It could equally be the case that a recovery focused relationship, in which boundaries between helper and helpee are more permeable, shared experience and common humanity are recognised and decisions are made together, each contributing a very different kind of expertise, is co-produced. Indeed, mutuality and reciprocity are founding characteristics, and essential for the full benefits, of peer support.
- The corner stone of building on assets can be easily and visibly achieved as a group or team forms around a project. As the team witness others’ contributions being needed and valued, a transformational process begins. Identities shift and people experiment with sharing ideas, questioning assumptions and taking on tasks. It might be argued that this process cannot be emulated in a dyadic relationship. Alternatively, the more equal relationship that takes place in a recovery focused encounter, where both the helper and the helpee put forward ideas, draw on different kinds of evidence, and share personal views in an open and evolving conversation, then solutions can be developed, refined and shared in a coproductive manner.
So perhaps in individual work, there is potential for a descriptive level of coproduction to take place. However, we need to be sure to distinguish it as something more than a compassionate or fundamentally respectful human interaction. There is an active and generative quality to co-production which makes it distinct, recognisable and beneficial beyond those involved.
We are keen to stress that we see collaborative and shared decision making as key to any recovery-oriented therapeutic relationship. The question here is not whether there is value in working collaboratively, but rather whether work at this individual level is true to the nature of transformative co-production.
Case Study One: Co-Producing Within A Team – Developing a Training Package
Sue Barton, Deputy Director of Strategy and Change, South West Yorkshire Partnership NHS Foundation Trust
In South West Yorkshire Partnership NHS Foundation Trust (SWYPFT) we decided that we needed to really understand coproduction if we were going to establish our four Recovery Colleges with coproduction at their heart. So, we set out to co-design some co-production training that we could co-deliver to service users, carers and staff as part of our Recovery College curriculum.
We started by inviting a range of people to a workshop. This included service users, carers and staff (both from services and from our learning & development team). In the workshop we heard from colleagues who had been working co-productively for some time. They encouraged us to consider what strengths we each brought to the development of the training and how we might bring them together to help others understand what co-production was all about. We had some surprises when we identified our assets, and a sense of amazement at the wide range of skills and experience that we had at our disposal. We also lost our way a bit when we forgot to use all our talents, such as leadership and training design. A small group of people from the session volunteered to go away and pull together a plan for how the co-production training might look. We then invited the whole group back and delivered it to them, asking for comments and feedback which were incorporated into the training that went into the prospectuses. One key feature of this was that, as facilitators of the course (who were a combination of people with lived experience and people with professional experience), we removed our badges and asked the participants to do the same. We wanted people to bring all their assets to the learning, not just their expertise derived from living with a condition or professional training. Since then, we have delivered the training to both staff, students and partners within the Colleges. Each College has taken the training and developed it further as part of their overall offer.
We learnt a lot from this experience, including:
- We bring individual assets and some of these do not directly linked to our role e.g. a service user, as a teacher, had considerable experience of delivering training; a staff member had many creative ideas for how we might engage people even though this wasn’t part of their current job role.
- Co-production is very different from service user-led approaches and for it to be successful we need to respect all types of experience and expertise equally.
- There are so many resources in the room when we intentionally identify them and collect them together, and that makes this work exciting and stimulating and the end product much better.
Case Study Two: Co-Producing Within A Service Line – Establishing a Recovery College
Lesley Herbert, Consumer Advisor – Adult Mental Health & Southern Health NHS Foundation Trust
Anna Lewis, Senior ImROC Consultant
Co-producing the Recovery College in Hampshire was a natural next step in a journey that had begun several years previously. Building on solid foundations (such as co-facilitated WRAP training, service user involvement and development of a ‘consumer advisor’ role as part of the management team), we drew together disparate strands of activity and established the College. With a modest additional budget and a few months to achieve it, we designed and recruited the workforce to reflect both ‘lived’ and ‘professional’ experience, secured premises, co-designed the curriculum and all aspects of its operation. We gave the work a high profile within the Division and organisation, and put it at the centre of our recovery effort as one of the six national pilot sites for ImROC. A group of people with diverse professional and lived experience, crossing several layers of organisational hierarchy, worked in partnership to lead the process and modelled the values and principles they sought to inspire in others.
The work was underpinned by our commitment to recovery, which we had brought into the mainstream of our Division’s strategy and ethos. The longstanding passion and vision previously held by a small number of champions was now boosted by support from service leaders who had the authority to act. The sharing of power implicit within this new relationship was what made the possibility of co-production real. At every opportunity we spoke about our role in services in different ways. We used the language of strengths, assets, education, partnership and collaboration such that we reframed the concept of expertise to extend beyond the professional voice and the traditional treatment model. We began to redefine what it meant to provide good care.
We sought to ‘walk the talk’ in the College’s development, at the heart of which was the employment of peer trainers within the team. While there had been routine service user involvement in recovery training previously, offering substantive peer employment opportunities to individuals was a significant step forward. Where people had previously been invited to share their story within professionally led and oriented training, the role of lived experience was elevated. Peers became equal partners with professionals in the design, development, delivery and evaluation of courses. They were recognised and valued as members of staff, subject to the same expectations and responsibilities as each other. Everyone took a courageous step into the unknown.
This was our first attempt at real co-production both individually and organisationally, and unsurprisingly it wasn’t always easy. It was difficult to work in ways that were not the cultural norm, and it was hard work to reach a functional level of understanding of the goal amongst the organisation’s leaders and other key influencers. We struggled at times to find a good balance in the new relationships. We were trying to bring the very best of our collective expertise and wisdom to catalyse new relationships and better outcomes, but it took time for us to learn what that really meant in practice. Indirectly we were also breaking down traditional hierarchical boundaries between us by taking an inclusive and mutually respectful approach. The work acted as springboard for many other co-productive efforts that have been pursued since.
We learnt so many things about ourselves and our services along the way. Here are three of them:
- Be ready to learn things about yourself and others that you could never anticipate. There are predictable challenges, and then there are subtleties about the dynamics in human relationships, intentionally constrained by the divides between ‘professional’ and ‘patient’, that are new, real, raw yet ultimately rewarding. This has a very real impact on the pace at which you can achieve cultural change. Making mistakes is part of the experience.
- Feeling OK that co-production doesn’t equate to consensus, and that differences of views need to be accommodated just as in any other aspect of life. Having to make and be accountable for difficult decisions in ways which don’t rely on falling back on positional power and honour the essence of co-production is way beyond the comfort zone of NHS convention and skill.
- We noticed that sometimes we were at risk of replacing one dominant power structure with another. Professionals took too many steps back initially and risked tipping the balance in the other direction. We learnt through experience that it is much harder to find equality in the relationship than it is for one to dominate the other.
Case Study Three: Co-Producing Within A System – Redesigning A Pathway of Care
Becky Aldridge, Chief Executive, Dorset Mental Health Forum & Kath Florey-Saunders, Head of Mental Health and Learning Disabilities, Dorset CCG
In Dorset people had made us very aware that changes are needed within our mental health acute care pathway and we were keen to address this. Dorset has a mixed urban and rural population of approximately 750,000, with a diverse range of need. We wanted to approach the review of the current acute care pathway differently, and at every stage to co-produce options for a new model of care that would improve experience and equity of outcomes across the county.
The project, facilitated by ImROC and NDTi, started with co-production at its heart, by working with people with lived experience and other partners to design the first stage engagement plan and materials. Previous engagement work to gather views around mental health service provision had not been based on co-production principles. Co-producing the engagement process ensured that we would be able to connect with people in a way that was meaningful and resonated with them. Our engagement on this occasion was very successful and delivered over 3000 views from over 750 people. These views informed the work of the co-production modelling groups and the objectives that any new models of service needed to meet.
The co-production modelling groups included people with lived experience, their carers, statutory partner organisations and local NGOs, all working together sharing their knowledge, experience and expertise to build options that might address everyone’s issues as far as possible within the financial constraints. The groups recognised the differences in experience and knowledge, without focusing on people’s specific roles, ensuring together that there was an innovative and supportive environment for people to start sharing their power and taking responsibility as a collective group, for developing ideas that might work across Dorset.
During the modelling stage, the groups have looked at innovation across the world, considered significant issues in rural and urban areas and listened to challenges from both people who deliver services and people who access services.
This approach has helped everyone to learn and understand the whole picture in Dorset together, including experienced clinicians and people who have been accessing services for a long time. The co-production process has enabled people to consider and accept different viewpoints and to understand the broader picture and challenges.
During the process of co-producing options, people have become more confident in the commissioning process, provider organisations have been able to propose how they could deliver potential models of care and people who access services and their families have become active stakeholders in the design of future services in Dorset.
We have a long way to go, but co-production will be central to all mental health service reviews in Dorset moving forward. We are enriched as a result of this process and we will continue with this ethos and approach well beyond the end of this project.
We are continuing to learn throughout this experience. These are our reflections so far:
- Be willing to take more time at the beginning than you might think necessary. The foundation work with everyone who wants to get involved is essential to define what co-production is, what we want from it, and what skills we need to achieve it. This includes finding a common language in which everyone can participate.
- Establish a common understanding of the process, and the ‘give and take’ that it is bound to involve. This isn’t about a single agenda triumphing over others. It’s about working together, using the best of each other’s talents, to find a constructive solution, and one that you probably can’t envisage at the outset.
- It’s empowering to work with empowered people! Sharing power can feel uncomfortable and unfamiliar, but it can also be liberating and hugely rewarding.
Case Study Four: Co-Producing Beyond Service Delivery – Audit & Evaluation at Sussex Recovery College
Louise Patmore, Patient Lead to Clinical Strategy SPFT
Senior Peer Trainer Sussex Recovery College & Sara Meddings, Psychology and Psychological Therapies Consultant Lead for Recovery and Wellbeing
At Sussex Recovery College we have developed a process for co-producing research, audit and evaluation. During the early development of the College, service users were keen that we demonstrate its effectiveness, so we asked how we would know if the college was successful. We drew together suggestions from people using mental health services, professionals and managers. We formed a task group to take this forward. Psychologists and researchers scoped methods of measuring what had been suggested. Service users then looked at the measures and advised about what to use drawing on their expertise about how people might experience them. One peer used her wider network to advise about language and readability. Having agreed the measures, we organised a workshop with student reps, peer trainers, professionals and administrators to decide what processes and systems to use. We decided to integrate the evaluation with the Individual Learning Plans so that the process was intrinsically useful rather than an additional task.
As the group and College expanded, pressures for efficiency increased. The coproduction process slipped. This resulted in reduced engagement and incomplete audits. In response, we created a monthly meeting of students, peer trainers, professionals, researchers and College managers to focus on research and evaluation. We decide together what research projects to suggest and what we would like to audit and evaluate. This group then oversees the research process. For example, students, commissioners and managers were keen that we look at whether attending the College reduced service use. A trainee psychologist is currently analysing this. They attend the co-production meetings, are guided by peers on how to go about evaluation sensitively, by researchers on robust statistics and methodologies, and by staff and managers on capacity and what is possible. The researchers gain supervision from the group and in turn provide what the stakeholders require.
We are not there yet but here are the lessons we are learning:
- We need to prioritise, critically review and strive to improve co-production. In a busy environment with multiple pressures, co-production and teamwork can slide. We have experienced this and the quality of what we have done has suffered.
- We need to invest adequate time in co-production and an infrastructure to support it. When we allow space, build relationships and invest time listening and including people, utilising everyone’s assets, we have better suggestions for evaluation, achieve higher quality, shared ownership and increased participation.
- We need to acknowledge differences in power, try to build equality and redress the power imbalance. Genuinely appreciating the assets people bring is a start. We need to be prepared to accept decisions that leads do not initially want. Reasonable adjustments may be needed for equal participation. We need to be flexible, accessible and thoughtful about participants’ experience of co-productive efforts so that we continually strive to improve it.
Case Study Five: Co-producing Throughout An Organisation – Developing Training for Central & North West London Corporate Services
Valerie Morrow, Recovery Programme Lead & Interim Head Occupational Therapist for Offender Care & Veronica Kamerling, Experienced Carer/Trainer
As part of CNWL’s commitment to creating and sustaining a context of more equal ‘partnerships in care’ with our service users and carers, the Trust’s Recovery Programme Lead worked together with a carer Peer Trainer to co-produce and codeliver workshops for corporate colleagues entitled ‘Redefining “user involvement”; co-production and partnership working’.
Initial thoughts around what might be included emerged from discussions in an ImROC-led ‘What is co-production?’ workshop. This led the facilitators to draw on further literature, in order that the workshop would enable a discussion focusing on strategic co-production within and external to the Trust.
The workshop aims were:
- To reach an understanding of what is meant by co-production, the challenges & the benefits.
- To adopt an approach which differs from more traditional involvement and engagement.
- To identify the processes & the structures that are needed to support co-production.
- To outline action plans which achieve effective shared decision-making.
We scoped the corporate services we wished to target. Time was one of the main challenges. We worked with managers and their teams to understand their constraints, as well as emphasise the importance of the workshop, and we were flexible about how and when it was delivered to maximise participation.
A range of corporate services were included: Human Resource Managers & Recruitment Team, Occupational Health, Quality & Audit; including the Patient Support Service, Communications & Marketing, Programme Management Team, Trust Employment Services, Information Governance and the Serious Incidents Investigation Team.
Services were encouraged to identify areas already underpinned by “service user and/or carer involvement” before thinking together about how co-production could create new possibilities.
Participants were given an opportunity to identify the challenges of this way of working and how these concerns should be taken seriously. The inclusion of an action plan enabled participants to have clarity regarding the task they considered would be best co-produced and what skills and expertise they would be looking for in those who would co-produce. Teams were also invited to think about how peers would be recruited, selected, prepared, rewarded and supported.
Once this project gained momentum, requests for bespoke workshops started to emerge from operational, clinical and corporate teams across the Trust.
Lessons we have learned:
- Roll with resistance, try not to judge, and prepare to be surprised!
One of the most positive outcomes of this project was a greater understanding of how some individuals working in corporate services often feel far removed from the service users and families/carers we all seek to serve. The workshops offered staff a safe place to explore some of their own attitudes and prejudices about mental health issues and there was the sense of a new conversation beginning to emerge. This included honest conversations about concerns and anxieties, for example reliability of service users to engage consistently, confidentiality, and accountability for decision-making. Challenge and self-expression are vital for transformative co-production, as is broad engagement from a diverse range of people.
- Lay the groundwork, ensure “buy in” from senior management and invest realistic time in training and follow up.
We had not anticipated how difficult it would be for some services to come together for two hours. Investing time with Team Managers in an attempt to secure their “buy in” for the workshops paid dividends in some services. If the Team Manager was not perceived to be engaged and committed, staff members voted with their feet. It was essential to have the support of the Trust Recovery Lead and the Chief Operating Officer in engaging with senior managers and prioritising the training.
- Carers and families back on the agenda.
Co-delivering the workshops with a carer proved to be a very effective way of putting families and carers back into the consciousness of both corporate services and clinical teams. Veronica encouraged an open and frank discussion about the challenges of working with carers through her non-defensive delivery and excellent sense of humour. This facilitated teams to acknowledge how they often struggle to work with families and carers and seemed to inspire them to try a different approach. Through providing a space for a genuinely collaborative approach, participants were able to see that carers and service users bring a new perspective and may offer new ways of working.
Case Study Six: (Re) Building Lives in Rushcliffe – Co-Producing a system wide response to a key challenge in primary care
Julie Repper, ImROC Director and Liz Walker, Peer Support Lead, Nottinghamshire Healthcare NHS Foundation Trust
This project began when we were approached by a commissioner and a GP/psychiatrist from a local primary care Vanguard site to consider ways of supporting people with ‘chronic’ depression to rebuild their lives in their communities. We responded by turning to the local community for solutions. We arranged a meeting with more than 30 people representing different local community groups, services, mainstream resources, ambulance service, police, churches, carers …. We presented the challenge to the group and everyone volunteered some way in which they could help by drawing on their own expertise, resources and experience. We built on this by presenting some innovative service delivery models that had been shown effective in research on community development (social prescribing, community cafes, asset based community development, peer navigators, sports hubs…) and participants discussed each of these, then fed back ideas of how they might work in the local community. By the end of the meeting we had coproduced a ‘framework’ that everyone from the local community volunteering service, to dementia friendly communities, the Baptist church and the local fire brigade could sign up to: they could see a role for themselves and could imagine it working. This entailed peer workers employed within GP surgeries to link people with roles, relationships and activities in their communities; and the development of community cafes (funded by the church and staffed largely by volunteers) as a central hub for self management workshops, peer meetings, activities and mental health advice to take place.
This plan was successfully submitted for pilot funding and is now in the early stages of implementation. The model is strongly supported by the co-production group who are now meeting fortnightly to oversee the ongoing development, implementation and evaluation of the service. Numbers of participants are ever increasing as local communities see the benefits for individuals and for their overall community capital. This really is a triumph of coproduction that demonstrates the huge rewards of working together. However, the challenges facing us as we all move forward together include:
- Inequality in contributions and rewards. Some participants give voluntarily and generously of their time and others receive payment (either working on the project as part of their salaried employment, or directly paid out of the project). Whilst successful co-production depends on contributions from all parts of our communities, paid and unpaid, rewarded and unrewarded, this does not make it acceptable or right. As our project progresses we will bring this topic up for careful consideration and debate by the co-production group.
- Sustainability. For as long as there is funding available then someone can be held accountable for co-ordination of the project, trouble shooting, ensuring proper governance, supervision and consistency of service. If funding ceases, then despite the majority of the service being provided voluntarily, it will not be viable. Evaluation of the service will need to focus clearly on cost effectiveness and return on investment to justify funding beyond the pilot stage.
Case Study Seven: Co-producing A New Urgent Care Pathway, West London Collaborative
Jane McGrath, Chief Executive, West London Collaborative
West London Collaborative (WLC) is an independent Community Interest Company (CIC) that uses authentic co-production to create and sustain meaningful working partnerships between the providers and commissioners of health & social care services, academic institutions and the communities they serve. Our partnerships utilise authentic co-production and disruptive innovation in operational and strategic areas of transformational change. In our work, all stakeholders learn how to share power and responsibility to solve difficult problems together. We use an assets-based community development model with the broader ambition that communities will become more healthy and empowered through becoming active citizens. WLC acts as a consultancy rather than a service provider, providing tools and frameworks that support local relationship building and networking. We expect our partners to be true partners – accepting mutual responsibility for ideas, solutions, success and failure. WLC was formed by service users, carers and staff of West London Mental Health NHS Trust after an event hosted by ImROC in 2013 – “From Service Users to Coproducers”.
We work with the Trust both operationally and strategically. Projects are wideranging, examples including supported decision making in medication, through to local services transformation.
We have coproduced the urgent care pathway across three London boroughs, using social media to really reach out to the community and to staff that could not get to our event because of shift work. We used Twitter and built a micro-website ‘Test My Story’ where the whole community built complex scenarios to test the proposed urgent care model. We then hosted a forum theatre event where we live replayed the coproduced scenarios using digital technology and voted collectively on preferred responses. Police, ambulance, commissioners, liaison psychiatrists, GPs, front line staff, three NHS trusts and the wider community, attended the event. The day was broken into sections and stories so that busy staff could attend the sessions that interested them and we have since won an NHS England community grant to make a short film about the work.
We have identified some key learning since we set up. A horizontal model can be tricky in a vertical hierarchical organisation. The two models can butt up against each other and we can get stuck or meet pockets of resistance. Yet the value we bring beyond solving the complex problem is the process itself – reflective space, time to pause and new thinking and techniques for problem solving. As much as we meet resistance, we also meet amazing, passionate staff who are refreshed and encouraged by this new way of working. When in full flow and at its best, co-production is joyful. At its most challenging, there is pain and tears. As coproducers we strive to work collaboratively, moving away from ‘them and us’ positions, we use critical reflection, appreciative inquiry, dialogue and Argyris’s Ladder of Inference (1990) to debunk assumptions. However, the fine line between critique and challenge is easily crossed, sometimes leading to conflict. People bring baggage. People want to challenge what is hurting them, much of which is happening in the context of austerity.
Challenging questions about poor data and unreliable evidence is uncomfortable. Before we can truly coproduce we need transparency and trust and to collectively distinguish signal from noise. This aspiration is still a work in progress for the NHS.
Co-production work often happens in disjointed silos, and behind doors in selected phases. Local landscapes are vast and the systems complex, and staff churn at all levels is a recurring problem. To counter this, WLC now aspire to stay coproducing through the life cycle of a project, from the very first conversation where we establish what question we are exploring together, to the potential co-delivery of the service. We collectively accept when things were not perfect (for whatever reason) – but we absolutely name what could have been better… and we also celebrate our success loudly, making films, poems and hosting community events. It is progress we seek, not perfection.
Discussion/Themes
The case studies illustrate well our broader ImROC experience of co-production in mental health improvement work. What might these individual experiences, each encountered in their own unique context, offer us in terms of thematic learning that might be applied elsewhere? We now attempt to draw out an answer to this question, building on the principles of co-production outlined above. It is not our intention to advocate a ‘lift and shift’ approach to such learning. In other words, the learning is there to inspire, be thought-provoking and give rise to new conversations in your own unique setting and circumstances. It is not offered as any kind of short circuit or quick fix to the application or experience of co-production. The notion of a ‘journey’, while much overused, is nevertheless an essential metaphor in the understanding and experience of co-production. Making mistakes is part of the experience, and in the long term has the potential to strengthen and mature relationships and their effectiveness.
Every co-production journey begins with a leap into the unknown. While our case study authors may not explicitly articulate this, there can be little doubt that each entailed a courageous step into something unfamiliar, unexperienced, and untested, working against the well-established norms in the culture of the organisation and its ways of working. These steps were taken in times of significant pressure, in which the scope to make a mistake or fail is very limited for organisations and therefore their workforce. This requires a kind of leadership that is underpinned by a set of values and beliefs that are not typically nurtured in a professionallydominated culture. Often that leadership departs from the hierarchical definition and comes from the grassroots. The pioneers of this work show courage, tenacity and resilience on a daily basis, spurred on by a belief that working in equal partnership is at the heart of any recovery-oriented mental health service. Living with the discomfort of ambiguity and uncertainty is a necessity.
“ Challenging questions about poor data and unreliable evidence is uncomfortable. Before we can truly coproduce we need transparency and trust and to collectively distinguish signal from noise.”
“ Living with the discomfort of ambiguity and uncertainty is a necessity.”
Thus ‘holding the space’ for effective coproduction to take place, safely and without fear of reprisals, within an environment or culture which unknowingly can work against it, is a vital responsibility for the leaders of the work. There is value in having a leader or ally who can build the bridge between the prevailing and desired cultural norms, in ways which seek to include others in that task. For example, if someone brings positional power in aid of a more distributed vision for leadership, then that is their asset to value and nurture in the co-productive relationship.
“ Learning through co-production complemented the notion of learning or improvement in the end result”
On a related theme, the process of coproduction is strengths-based. The values and techniques are appreciative, inclusive, assets based, and ambitious. They recognise the unique contribution and worth of every individual. They give voice and focus to ideas, creativity and passion that have traditionally been excluded. Yet as our case studies illustrate, this is not always an easy path to tread. The baggage gets in the way, causes pain and conflict, and can leave people feeling anything but appreciative. This is the cue not to desert the approach but to reinforce it. The way in which the space is shaped is vital to the resilience of the effort to do something better. So the process of co-production is at least as valuable as the outcomes it delivers or problems it solves.
Time is a recurring theme. In highly pressured working environments, in which it is faster, and arguably more predictable, to do what you have always done than it is to try something new, carving out the time and space is difficult. Permission to do so may also be difficult to achieve when the desire for rapid results is pressing from above. The fast pace requirement for ‘delivery’, amongst multiple competing demands, creates an impatience which is understandable yet not conducive to innovation. Developing new skills, forming new habits and testing out new approaches take time and are exposed to threats from the daily grind and very wellentrenched ways of thinking and working. Co-producers identify time, and implicit within that a tolerance for making reasonable mistakes and needing to repeat stages of an improvement process, as key to their progress and impact.
“ The preparedness to share power and responsibility, or even to nurture the environment in which power can be taken, is requisite in every coproduction experience.”
Breaking down barriers between providers and consumers of services, which have served all kinds of purposes in the past, is an essential endeavour within co-production. The preparedness to share power and responsibility, or even to nurture the environment in which power can be taken, is requisite in every co-production experience. It can be particularly challenging in the early stages when the new relationship and patterns of behaviour have not yet matured. This is a common experience through ImROC’s work. Dedicated professionals, confronted with the realisation that aspects of their training, practice and culture have been at odds with a more inclusive and appreciative approach, may ‘back off’, feel invalidated and even become apologetic for their role. The latent holding of power in a relationship may in itself be difficult to identify and then confront in oneself, especially when intentions are honest and come from a place of care and compassion. Intellectually the professional may have that ‘light bulb moment’ but the emergence of new behaviours, attitudes and practice comes as a result of a series of trial and error, success and failure, unlearning and relearning over time. This reinforces the importance of safe space in which people can explore their journey together and individually, in ways which enhance and validate the new practices, rather than work against them.
“ Leadership that is underpinned by a set of values and beliefs that are not typically nurtured in a professionally-dominated culture”
For those with lived experience, there may also be challenges in engaging in this new kind of relationship. The vivid and intensely personal story of each individual has the power to engender change for the better, and it is an act of courageous generosity to share it. That is not to say that the story alone will make the difference. Co-production is not about swapping one dominant power base (that of the professional) for another (that of the person with lived experience), although we see this in our work as a common misconception. While of course there is a place for user-led services, this negates the value of equal partnership that comes about when diverse experience gained through professional training and through life is respected, pooled and put to work. This notion of collective wisdom, underpinned by a shared humility and humanity, and with it collective responsibility for outcomes, provide the foundation for co-production.
In a similar vein, the basis on which coproducers engage with each other needs to be fair, honest and transparent. In seeking equality, it is important to generate a shared understanding of individual contributions, and avoid drawing distinctions on the basis of traditional labels of ‘professional’ and ‘patient’. It is incumbent upon all concerned to hold each other to account for the contributions expected and made, making ‘reasonable adjustments’ without straying into ‘making allowances’. Implicit within co-production is the avoidance of ‘othering’ – labelling difference between individuals as a legitimate basis for exclusion, separation or special treatment. Each person, regardless of their label or status, is treated equally. That means taking the rough with the smooth. To do otherwise simply reinforces the othering that divides and labels people on the basis of deficits rather than assets. In short, we have mutual expectations and we hold each other to account for those in the pursuit of fair and equal partnership.
The shifting dynamics in a co-productive relationship may feel harder to achieve when there is an established relationship akin to traditional engagement or involvement of service users, that has long been popular in mental health services. While the track record of user involvement may offer a useful building block for a more sophisticated relationship between different constituencies within services, co-production represents a step change in the way we work together and should not be perceived as anything less. The legacy of traditional engagement can be a barrier as much as an enabler.
“To stay coproducing through the life cycle of a project, from the very first conversation where we establish what question we are exploring together, to the potential co-delivery of the service.”
A common hindrance to this sense of equality is the differential terms and conditions, and particularly remuneration, that remain amongst those traditionally distinct cohorts of contributors. The differences in remuneration between ‘professional’ and ‘patient’, and sometimes the difference in contractual employment status or tenure, do not speak to an equal valuing of expertise. This is a barrier that is likely to take some time to resolve, as lived experience grows its prominence in the mainstream workforce.
“Co-production doesn’t equate to consensus, and that differences of views need to be accommodated just as in any other aspect of life. Making mistakes is part of the experience”
The process of co-production is a voyage of discovery and thus is embarked upon in a spirit of adventure. While people come together around a common intent, the nature of the journey you will take, and even the destination you may reach, are yet to be discovered. It is an emergent process full of possibilities, guided not by a highly-specified goal but by a willingness and commitment to try something different in the interests of a common desire. The process is revelatory, drawing out strengths and resources we didn’t know we had or couldn’t recognise in ourselves. It helps us to understand our individual and collective contributions with much greater clarity and purpose. This feels quite distinct from the more conventional means by which we pursue goals or activities in services.
All of the case studies featured examples that involved doing something new or innovative, in which the notion of learning through co-production complemented the notion of learning or improvement in the end result – such as developing a Recovery College or redesigning a care pathway. In other words, the idea that we can achieve something better together wasn’t limited to the design of a new initiative, but it carried on through into implementation, delivery and evaluation.
These ripple effects are often described in the process of cultural transformation that we witness in ImROC. Contrast this, however, with a common frustration that scaling up the impact can be very difficult to achieve.
As well as the many positives illustrated by our case studies, they show equally that our aspirations are not yet fulfilled. ImROC’s work has been grounded, purposefully and intentionally, within the realms of mental health service delivery in large organisations. Recovery Colleges, in particular, have been at the heart of our co-production work. Over the last couple of years, we have been taking deliberate steps to broaden our focus. Cahn’s ‘core economy’ includes families, friends, neighbours and local communities – all assets which are not universally visible in the activity that the case studies describe. That is not to say that what we are witnessing is not co-production, rather it is an acknowledgement of the potential scope for strengthening our community impact, moving beyond a service to a community focus, as WLC has done from the outset – from seeing people as defined by their relationship to services to seeing them as citizens first. Just as co-production is a journey of exploration and discovery, so ImROC as a community of practice reflects this. It is timely that we consider our role and contribution and that we increase our focus ever more on supporting people to have lives rather than services. In order to achieve this, we are actively developing new partnerships and stepping beyond health and social care into citizen spaces.
Other Observations In ImROC’s Co-Production Work
Co-production can achieve outcomes that spread beyond the core brief of a project or other effort. It creates and taps into communities of engaged and active participants. Boyle (2006) identified ‘clear links between involvement in time banks and reduced levels of medication and hospitalisation’ and (in 2010) suggested “savings of up to six times the investment made in new approaches”. People attending Recovery Colleges form peer support networks and become more active community participants. The extent to which these individual benefits can be measured and aggregated across groups, and then attributed in terms of cause and effect is problematic, however. As such, the scope to predict and quantify outcomes is limited, at least within the prevailing narrative that revolves around narrow commissioning briefs and funding flows which fail to capture the rich and diverse ways in which lives are improved. Making the co-production case to sceptics is made more difficult as a result. ImROC is supporting RECOLLECT, a three-site study in 2017 investigating key components and change processes supported by Recovery Colleges, and understanding who uses them. Co-production is emerging as a central and influential component of Recovery Colleges. More information on the RECOLLECT Study is at researchintorecovery.com/recollect.
Retaining fidelity to the principles of coproduction while embedding or scaling up co-productive efforts is a common challenge. It can become a victim of its own success, rendering itself invisible through its normalisation and business as usual. At the outset of the journey, there is a deliberate and mindful focus on this new way of working, accompanied by an understanding that it takes investment of time and attention to succeed. As it becomes less new and more familiar, it is easy to assume that it will take care of itself. Instead it becomes vulnerable to an unconscious neglect and degradation. In our experience, this is felt as a loss of enthusiasm, direction, priority or connection. Being able to pre-empt this risk, or at least identify it quickly, is key to limiting its negative impact. Co-production is all about relationships, and so like any other, it requires nurturing attention to remain healthy and effective.
It is also the case that many decision-makers will actively choose to hold specific coproduced projects on the safe periphery of an organisation’s operations, pursuing low key efforts that have no major consequence if they slip or fail, and that pose no great challenge to the prevailing power dynamics. There is no intention to allow this ethos any closer to mainstream ways of working or organisational beliefs and value systems. Whilst we advocate starting small and working with what you have (which may well mean something around the edges initially), we see this as a tactical approach which creates a springboard into more substantial and transformative change that confronts traditional hierarchical power bases, rather than a glass ceiling of possibility. Co-production is neither a ‘task and finish’ endeavour, nor a fair weather pursuit. It should not be attempted in a ‘start/stop’ style. Its full potential is realised only through an absolute commitment to its principles and practice throughout an organisation, group or community, which means that it is there at every single stage of a project’s life. That commitment is unlikely to emerge at the outset and champions on the ground shouldn’t feel the need to wait for it, but it should be the goal and focus for any strategic effort, in order to reach into and discover the transformative realms of possibility that co-production offers.
Finally, there is a celebratory sense about co-production. The value achieved through co-production, to the individual, the team and ultimately to a community, brings hope and pride rarely seen in more traditional approaches to improvement. The ‘feel good factor’ associated with working through challenges, making errors and resolving them together using an assets-based mentality is energising for disillusioned professionals and people with lived experience of mental health conditions. Yes, it can be messy, frustrating, and exhausting. Yet the experience is ultimately validating, enriching and life-affirming. It offers opportunity for personal growth. The sense of discovery, helping each other to find out what we are really good at and then using that towards a common hope, energises us for the more testing aspects of co-production. To quote WLC, ‘we seek progress, not perfection’.
Top ten tips for co-production
- Gather the right people for the job. Identify key stakeholders for an initial meeting to discuss the challenge and use this group to generate a network of peer, family member, personal and professional expertise offering a diverse co-production group with relevant skills, knowledge and experience. Identify all of the assets in the room (not only those related to their role). Be prepared to invite new individuals and/or ask for advice and contributions from other relevant groups. Allow free movement so that people can choose to join after it has started or choose to leave if they feel it is not for them. Make this an inclusive experience. It’s important to avoid the perception of cliques often associated with conventional methods of ‘involvement’.
- Just get started and build momentum around your shared purpose. Don’t wait for the perfect moment, or the perfect set of people but build momentum and expertise around your shared purpose and understanding of the process. This will act as an anchor when things get tough.
- Spend time agreeing the structure and the values of meetings. This may involve assigning a leader or facilitator; discussing the rights and responsibilities of members and considering how everyone can both ‘give’ or contribute to the task as well as ‘take’ or benefit from their engagement. Ensure that everyone understands what decision making power lies within the group.
- Support every member to contribute to their full potential. Nurture, support, offer learning opportunities, make necessary adjustments and enable everyone’s voice to be heard. Take an even-handed approach across the group, adapting according to need, not label – avoid the temptation to ‘other’ those who may be less experienced or confident in the setting.
- Tackle the challenge in small steps. This process will create new ideas, present new challenges, suggest new solutions which require further exploration. Test lots of ideas. Make it safe to fail. It is not possible to work to a predefined set of outcomes in a predetermined time frame.
- Listen, listen, listen. Co-production will only achieve its full potential if every member is prepared to listen and learn, see different perspectives, try new ways of thinking and consider new ideas. It is important for everyone’s voices to be heard, so members will need to gauge their input so that those who find it more difficult to speak up have that opportunity. However, the overall ‘culture’ of the group is one of valuing everyone’s contributions and genuinely exploring their utility in the given context.
- Back up decisions with evidence. One of the concerns about co-production is that any decisions will be based on personal experience rather than ‘hard evidence’. The challenge for the co-production group is to back up personal experience with research that demonstrates this goes far beyond one individual. This does not need to be large scale statistical research; accumulated personal narratives, qualitative research and routinely collected data that can be used to demonstrate a level of need or the efficacy of a suggested approach. It is also possible to increase authenticity and credibility by ‘sense checking’ certain aspects with a wider audience.
- Beware the comfort zone. Keep a watchful eye to avoid slipping back into old familiar ways, and be mindful of the triggers – such as challenging conversations, differences of opinion, or external pressure to deliver. Be willing to talk openly about this, and regroup around your shared purpose. This is a particular challenge when you increasing the scale of the project – this rarely happens easily or smoothly but needs careful attention.
- Look to the bigger picture. Consider how your project can influence behaviour, attitudes and outcomes in the wider system. Grasp opportunities to lead others. Even better, create them!
- Cherish what you create. Co-production comes from the heart. You are building a community like no other. Recognise and embrace its value, strength, wisdom, and potential. Nurture it, celebrate it, love it. It will reciprocate in spades.
Conclusion
Co-production, and the values and beliefs that underpin it, offers communities and individuals a sense of hope when many other sources of inspiration feel endlessly lacking. More than that, it offers real and achievable solutions to challenges which are increasingly proving too great for conventional means of problem-solving, orchestrated by and mobilised through professional expertise.
Our case studies cast a light on what is possible when people with diverse backgrounds and experiences come together with an open mind, and draw out expertise in each other towards a common vision or passion. The examples are easily accessible and we think anyone can give them a go. We have used tangible and routine outputs, like developing a training programme or evaluating a service, to frame a much more significant story of transformation. It is a story anchored in a belief that every person has something valuable to give, and that each derives value in return. This is the message that sets these stories apart from others. That is the ethos and expertise on which their success has been founded. We believe these stories are representative of a growing movement of grassroots change in communities around the UK and beyond. None of us believe this is a ‘job done’. In fact, it is a job just started.
As we develop our contribution to this movement through ImROC, our focus is moving beyond our origins in the mental health community, to embrace the wider world of community wellbeing. Improving mental health has a far greater reach than improving mental health services, and it is in this mission that we seek to unlock the full potential of co-production, as yet unknown and undiscovered by any of us.
Get In Touch
We hope this paper provokes conversations and we would love to hear what you think. If you would like to offer feedback, or would like to support us in our co-production journey, please email imroc@nottshc.nhs.uk or call 07392318188.
References & Resources
Alford 2002 Alford, J. (2009) Engaging public sector clients: From service-delivery to coproduction, Basingstoke: Palgrave Macmillan
Bovaird, T. (2007) Beyond Engagement and Participation: User and Community Coproduction of Public Services. Public Administration Review. Volume 67, (Issue 5) 846–860
Boyle, D. (2004) Is this How to end Public Service Failure? NewStatesman. Feb 23 2004 accessed at: http://www.newstatesman. com/node/194958 on 2 Nov 2016
Boyle, D. and Harris, M.( 2009) The challenge of co-production: How equal partnerships between professionals and the public are crucial to improving public services, London: National Endowment for Science, Technology and the Arts.
Boyle, D., Coote, A., Sherwood, C. and Slay, J. (2010) Right here, right now: Taking coproduction into the mainstream, London: National Endowment for Science Technology and the Arts.
Boyle, D., Slay, J. and Stephens, L. (2011) Public services inside out: Putting coproduction into practice, London: National Endowment for Science Technology and the Arts.
Bradley, P. & Willson, A. (2014) Achieving prudent healthcare in NHS Wales (revised). Cardiff: Public Health Wales
Cahn, E. (2001) No more throwaway people: the co-production imperative (Washington DC: Essential Books).
Frost, D. and Stenton, S. (2010) Learning to Lead: The story so far. Available at: http://www.learntolead.org.uk/wp-content/ uploads/2013/11/learning-to-lead-the-storysofar.pdf.
Mental Health Taskforce (2016) The Five Year Forward View for Mental Health. London: NHS England.
Needham, C. and Carr, S. (2009) SCIE Research Briefing 31: Co-production: An emerging evidence base for adult social care transformation, London: Social Care Institute for Excellence.
Ostrom, E. (1996) Crossing the Great Divide: Coproduction, Synergy, and Development. World Development, Vol. 24, No. 6, pp. 1073- 1087.1996
Repper, J and Perkins, R. (2013) The Team Recovery Implementation Plan: a framework for creating recovery-focused services ImROC Briefing Paper 6. London: Centre for Mental Health and Mental Health Network, NHS Confederation.
Rowe, J. (1997) Money with care built in YES!. A Journal Of Positive Futures Spring 20-25 accessed at http://www.yesmagazine. org/issues/money-print-your-own/the-basicfunction-of-money 5.6.15
SCIE’s Co-Production Strategy, accessed at http://www.scie.org.uk/coproductionnetwork
Scottish Co-Production Network, accessed at http://www.coproductionscotland.org.uk/ on 1 Nov 2016
Slay, J. & Stephens, L. (2013). Co-production in mental health: A literature review. London: new economics foundation
Social Care Institute for Excellence 2013. Co-production in social care:What it is and how to do it. Guide 51, London: SCIE
Stephens, L., Ryan-Collins, J. & Boyle, D. (2008) Co-production: A manifesto for growing the core economy, London: New Economics Foundation.
Authors & Acknowledgements
Anna Lewis is a Senior Consultant with ImROC and has a professional background in NHS mental health and social care management. She is particularly interested in the parallels between recovery, co-production, citizenship and leadership, and is inspired by the courage and tenacity of the people she meets through her work and in her local community.
Toni King is Trust Lead in Recovery & Peer Workers at Solent NHS Trust, Clinical Teaching Fellow at University of Southampton and an ImROC consultant. She is inspired to work in this area by the many people she knows who do difficult things and are brave enough to share their story. Some raise money, some raise hope, all have motivated her to keep learning and questioning her own practice and the systems in which she works.
Lesley Herbert has a track record of striving for the true essence of co-production within mental health, driven in no small part by her concurrent personal and professional relationship to services. She is continually struck by the parallels between her personal recovery and the processes of co-production. She would describe it thus: It’s a hard slog, but there are moments of beauty and wonder along the way that make the effort seem, even if briefly, more than worthwhile….
Thanks to all contributors for sharing their experiences so willingly, and to the fantastic ImROC team from whom we learn every day.
And to Ostrom and Cahn for giving us a language, a set of principles and concepts which are helping mental health services the world over bring their values to life in ways that have never before been thought possible.
Get In Touch
We would love to hear more about your project. Please fill out this form and we will get back to you.
imroc@imroc.orgImROC Head Office PO Box 11115 Nottingham NG14 6UZ
