Using peer support workers to support the recovery of people with mental illness can add significant value to mental health services, sometimes at no extra cost, according to new research published today.
This paper sets out the spectrum for peer support in mental health services, which can range from naturally occurring through to formal employment of people with lived experience of mental ill-health.
5. Peer Support Workers: Theory and Practice
Julie Repper with contributions from Becky Aldridge, Sharon Gilfoyle, Steve Gillard, Rachel Perkins and Jane Rennison
INTRODUCTION
Peer support is “offering and receiving help, based on shared understanding, respect and mutual empowerment between people in similar situations”. In this paper we will examine the concepts and principles of peer support and present examples from organisations which now have peers in their workforce.
The ImROC programme has recommended the use of peer workers to drive recovery-focused organisational change. ImROC recognises the value of a range of different roles for peers in all types of mental health services. Whether they are paid or voluntary, working in public, private or independent services, peer workers have a valuable role to play.
We have concentrated on the contribution of peers working inside mental health services because of the multiple benefits that they can bring. Working together, ‘co-producing’ services alongside traditional mental health professionals, they can offer a truly comprehensive and integrated model of care.
We also have to be concerned with maximising ‘value for money’ and we believe that peers – properly selected, trained and supported – can improve the quality of services at no extra cost, possibly even with cost reductions. This would put the voice of those with lived experience truly at the centre of mental health services – which is where it belongs.
ACKNOWLEDGEMENTS
Advances in recovery-focused practice arise from collaborative partnerships between individuals and organisations. The ImROC briefing papers draw upon this work. Each paper in the series has been written by those members of the project team best placed to lead on the topic, together with contributions from other experts. In this case, we particularly wish to acknowledge the contribution of those whose work on the theory and practice of peer support has led the field and inspired others. They are listed on the front cover. Without these pioneers, and others like them, we would have nothing to write about. In order to illustrate many of the points in this paper, we will use quotes from the Nottingham peer support worker project, Final report for Closing the Gap, The Health Foundation, (2012).
BACKGROUND
Increasing numbers of mental health services are developing peer worker roles and are faced with similar questions and challenges. As a result, a number of reports and recommendations have appeared over the last few years (Davidson et al., 2012; Faulkner & Kalathil, 2012; Mead et al., 2001; Mental Health Foundation, 2012). We want to try to bring together the collective learning from these publications, to examine some of the basic concepts and principles underlying the practice of peer support workers in mental health services and present them together with illustrative examples from organisations who have begun to train and employ peers as part of their workforce. This paper is accompanied by a second publication (‘Developing peer support workers in your organisation’, in preparation) which will cover the practical details of implementation in more depth.
For as long as people have used mental health services they have provided each other with friendship, shared coping strategies and supported each other through dark times (Davidson et al., 2012). As the value of such mutual relationships have been recognised, so more formal peer roles have been created in mental health services across the western world. In the United States, 27 states have collaborated to create a scoping and guidance document for peer support (Daniels et al., 2010). Peer workers have also been employed in various different roles and settings in Australia (Franke et al., 2010), New Zealand (Scott et al., 2011) and various parts of Europe (Castelein et al., 2008). In the UK, peer support has long played a central role in voluntary sector and user-led services/groups (Scottish Recovery Network, 2011; Faulkner & Kalathil, 2012; Mental Health Foundation, 2012) but peer worker roles in statutory services have been slower to establish. The ImROC programme has specifically recommended the development of peer worker posts as a driver of recovery-focused organisational change (see Challenge 8 in Shepherd et al. 2010) and the growth of peer support of all kinds appears to have accelerated supported by a number of organisations. Prior to 2010, it would have been difficult to find a single peer support worker employed in mental health services in England, but in 2013 Nottinghamshire Healthcare NHS Trust employs 25 peer support workers, Cambridgeshire and Peterborough NHS Foundation Trust employs 32; Central and North West London NHS Foundation Trust employs 12. Many other trusts employ peers as trainers, in volunteer, bank and mentoring posts.
ImROC recognises the value of a range of different roles for peers in all types of mental health services. Whether they are paid or voluntary, working in public, private or independent services, peer workers have a valuable role to play. This is recognised in policy documents in England, Scotland and Wales. For example, in England the Department of Health papers on Health, Social Care and Volunteering all recognise the role that peer support can play in providing support, facilitating self-management, aiding prevention, improving public health and reducing health inequalities. They recognise the value of community based “peer support services, user-led self-help groups, mentoring and befriending, and time-banking schemes, which enable service users to be both providers and recipients of support” (DH, 2011, p.32) and recommend peer support as one of the “roles of mental health organisations in implementing the mental health strategy” (DH, 2012, p.51). The Joint Commissioning Panel for Mental Health also recommends the employment of peer mentors and patient experts to work on ‘self-management, advocacy, training and mentorship programmes in order to improve personal understanding and responsibility for wellbeing’ (JCPMH, 2012, p.9). The recent Schizophrenia Commission (2012, p.35) specifically recommends that “all mental health providers should review opportunities to develop specific roles for peer workers”.
WHAT IS PEER SUPPORT?
Peer support may be defined simply as “offering and receiving help, based on shared understanding, respect and mutual empowerment between people in similar situations” (Mead et al., 2001). Thus, it occurs when people share common concerns and draw on their own experiences to offer emotional and practical support to help each other move forwards. This is well articulated by peer support workers from Nottingham.
“…They know I’m not the expert, they know we’re just us, both trying to beat the same demons, and we’re trying to work things through together…. I said to her, ‘I’ve got my own experience of mental illness, I’ve been on the ward myself and so on,’ and with that she sort of jumped up and gave me this huge hug.”
Peer support encompasses a personal understanding of the frustrations experienced with the mental health system and serves to reframe recovery as making sense of what has happened and moving on, rather than identifying and eradicating symptoms and dysfunction (Bradstreet, 2006; Adams & Leitner, 2008). It is through this trusting relationship, which offers companionship, empathy and empowerment, that feelings of isolation and rejection can be replaced with hope, a sense of agency and belief in personal control.
“I wanted to be able to show people that however low you go down, there is a way up, and there is a way out… The thing I try to install is, no matter where you are, if you want to get somewhere else you can, there’s always a route to get to where you want to be.”
The shared experiences of peers in mental health settings are most commonly their mutual experiences of distress and surviving trauma. However, it is not always enough simply to share experiences related to mental health. Support is often most helpful if both parties have other things in common such as cultural background, religion, age, gender and personal values (Faulkner & Kalathil, 2012). For people who have experienced marginalisation and exclusion (such as those from minority ethnic groups) it can be important for the support to come from someone who shares these experiences of oppression and/or of facing structural barriers so that they can ‘speak the same language’.
Relationships with others who share your experience are unlikely to be helpful if they are overly prescriptive, burdensome, or felt to be unsafe (in terms of trust and confidentiality). The peers from user-led groups interviewed by Faulkner and Kalathil (2012) also found that relationships were more supportive if both people were willing both to provide and receive support and had gained some distance from their own situation so that they were able to help each other think through solutions, rather than simply give advice based on their own experiences. For these reasons, training, supervision and support are all essential for peer workers employed in services.
DIFFERENT FORMS OF PEER SUPPORT
We can draw distinctions between three broad types of peer support: (a) ‘informal’ (naturally occurring) support; (b) peers participating in consumer, or peer-run, programmes alongside formal mental health services; and (c) employing people with lived experience within statutory services, irrespective of whether they are employed by the statutory organisation or by independent sector agencies.
These different forms of peer support also vary along a number of (not necessarily linear) dimensions. These include: the number of people involved, the level of choice involved, the rules governing the relationship, and the extent to which peers are at the same stage in their journey of recovery. These dimensions are summarised in Box 1.
Box 1: Dimensions of peer support
- Group vs. individual: Some forms of peer support, like peer run support groups and courses, offer only group support, although members may form individual relationships as a result of meeting through the group. Other forms, like informal friendships, buddy systems, co-counselling or individual interactions between peer workers (paid or unpaid) in services, provide more individualised support.
- Extent to which both parties choose to enter the relationship: Informal networks and friendships are entirely elective. Someone joining an existing group, or enrolling on a self-management course chooses to do so, but does not have choice over the other participants or the peer trainers. Someone entering a hostel, crisis or day service (whether user-led or not) may have some degree of choice about whether they enter the service and about the workers (paid or unpaid) with whom they engage, but the individuals using the service have little choice over who is employed there (although peers may be involved in staff selection).
- The ways in which rules govern the relationship: No relationships are entirely without rules or boundaries. Sometimes these are implicit, as in ordinary friendships while others are more explicitly stated, as in codes of conduct, for example in buddy and befriending arrangements. The most formal ‘rules’ are those contained in Job Descriptions which are usually set in a number of other regulations which govern employees of the organisation. Ethical guidelines differ in a similar fashion. In informal friendships they are implicit; in other relationships (e.g. peer support groups) they may be agreed by consensus or, again, formalised in codes of conduct for employment. These formal rules apply to all paid staff.
- Extent to which the parties involved are in the same place in their recovery journey: Everyone’s recovery journey is different and each journey is usually far from linear. At different points in time one person may be further on, but then they experience a setback so reversing roles. Often in peer support groups there is a facilitator or organiser who may, at the time of fulfilling this role, have moved further in overcoming the challenges than those who are new to the group. Similarly, it might be assumed that peer trainers in self-management courses or paid workers in services will have moved beyond their most recent experience. Clearly these roles can change over time, but peer workers may experience setbacks and people currently attending services can and do move on to the role of trainers, co-ordinators and workers. Such is the dynamic nature of peer support.
DIFFERENT ROLES
There are many different ways in which peer workers can be employed within mental health services.
They may work in dedicated teams:
- responding to referrals for peer support from other teams (Repper & Watson, 2012)
- working across ‘transitions’, e.g. from specialist community teams to Community Mental Health Teams (CMHTs), or from inpatient wards to CMHT
- providing specialist consultancy advice regarding recovery-focussed practices such as WRAP (Wellbeing Recovery Action Plan), or other forms of Personal Recovery Planning
- providing service-wide functions, e.g. speaking at staff induction, reviewing policy documents, undertaking quality assurance exercises, providing mentorship for staff, etc.
Alternatively, they may be employed in addition to staff in existing teams (inpatient or community) to bring a specific focus on the needs of service users:
- Facilitating earlier discharge from inpatient wards, working across boundaries to engage with inpatients prior to discharge, spend time planning for life in the community and then supporting people after discharge by home visits, meetings with friends and community contacts, etc.
- Leading on personal recovery planning, using their own experience to help the person identify and prioritise goals, develop understanding, control and selfmanagement strategies and to ensure that all of this is communicated to the professional staff team.
- Improving the value of follow-up appointments (e.g. outpatient consultations) helping the service user think through questions and concerns prior to appointments and how best to convey these to professionals. This can specifically help to establish the culture of ‘shared decision making’ (e.g. regarding medication management).
- Supporting learning in Recovery Colleges (Perkins et al., 2012) working with staff to co-produce and co-deliver courses and facilitate productive engagement.
- Leading on social inclusion. As already indicated, peer workers often come from the same physical and cultural communities as the people they are supporting. They are therefore particularly well-placed to identify appropriate community resources and activities and to facilitate engagement by accompanying their peers until they are confident and comfortable to attend alone.
As will be evident from the above, the peer support role as an adjunct to existing staff roles has considerable overlap with nonpeer support roles (e.g. Support, time and recovery ‘STR’ workers) and with peer advocacy. The difference is that peer support workers are specifically employed to use their personal experience to support others. But they cannot be expected to achieve this if they are left to work alone. In Recovery Innovations in the U.S. over half the mental health workers employed by the service are trained peers (See META Services Arizona in Shepherd, Boardman & Slade, 2008); and in Nottinghamshire the aim is for at least two peer workers in every team (see Nottinghamshire Healthcare Trust Recovery Strategy 2009-12, 2013-16). Some examples of peer worker roles are given in Box 2.
Box 2: Examples of specialist peer worker roles
Nottinghamshire Partnership Mental Health Intensive Care Unit (MHICU): The team leader had one ‘Band 3’ vacancy and was keen to bring lived experience into the team to promote a more recovery-focused ethos. The post was therefore converted to a peer healthcare assistant and three part time peers were recruited. They had all previously spent time in inpatient settings. The staff team spent a whole day learning about peer support, expressing their hopes and fears, generating ideas about how the peers might best use their experiences. Three months later all the peers say they are very happy working at the unit and feel they can make every aspect of their work recovery-focused whether it is serving meals, escorting patients or simply talking to them. They feel able to talk about their own experiences when appropriate and have day-to-day support from the team leader who encourages them to bring their insights and ideas to all team meetings.
Cambridgeshire and Peterborough NHS Foundation Trust – Integrated Offender Management (IOM) Peer Workers: In May 2012, CPFT appointed 5 peer workers to their IOM teams based in Peterborough, Cambridge and Huntingdon police stations. The role was very new and a lot of work was done to ensure that the peers worked out their roles in relation to the nurses also employed by the Trust in the IOM teams and with the police and probation staff who form the main staff groups. The peers are working in partnership with the trained nurses on the recovery needs of prolific offenders with mental health problems. They work with a number of external organisations, including drug and alcohol services, housing and adult education and have a particular role in training staff from other agencies (e.g. police) in relation to mental health issues. Due to the nature of the new role, a higher banding was required so that the peer workers could be more autonomous.
THE CORE PRINCIPLES
Whatever the form of peer support or the nature of the role, there are a number of core principles that peer support workers should aim to maintain. These are summarised in Box 3. They include: mutuality, reciprocity, a ‘non-directive’ approach, being recovery-focused, strengths-based, inclusive, progressive and safe. These principles can be used to guide training and supervision and to maintain the integrity of the peer role wherever they are located and whoever employs them (see below).
Box 3: The core principles of peer support
1. Mutual. The experience of peers who give and gain support is never identical. However, peer workers in mental health settings share some of the experiences of the people they work with. They have an understanding of common mental health challenges, the meaning of being defined as a ‘mental patient’ in our society and the confusion, loneliness, fear and hopelessness that can ensue.
2. Reciprocal. Traditional relationships between mental health professionals and the people they support are founded on the assumption of an expert (professional) and a non-expert (patient/client). Peer relationships involve no claims to such special expertise, but a sharing and exploration of different world views and the generation of solutions together.
3. Non-directive. Because of their claims to special knowledge, mental health professionals often prescribe the ‘best’ course of action for those whom they serve. Peer support is not about introducing another set of experts to offer prescriptions based on their experience, e.g. “You should try this because it worked for me”. Instead, they help people to recognise their own resources and seek their own solutions. “Peer support is about being an expert in not being an expert and that takes a lot of expertise.” (Recovery Innovations training materials. For details see www.recoveryinnovations.org)
4. Recovery-focused. Peer support engages in recovery-focused relationships by:
- inspiring HOPE: they are in a position to say ‘I know you can do it’ and to help generate personal belief, energy and commitment with the person they are supporting
- supporting people to take back CONTROL of their personal challenges and define their own destiny
- facilitating access to OPPORTUNITIES that the person values, enabling them to participate in roles, relationships and activities in the communities of their choice.
5. Strengths-based. Peer support involves a relationship where the person providing support is not afraid of being with someone in their distress. But it is also about seeing within that distress the seeds of possibility and creating a fertile ground for those seeds to grow. It explores what a person has gained from their experience, seeks out their qualities and assets, identifies hidden achievements and celebrates what may seem like the smallest steps forward.
6. Inclusive. Being a ‘peer’ is not just about having experienced mental health challenges, it is also about understanding the meaning of such experiences within the communities of which the person is a part. This can be critical among those who feel marginalised and misunderstood by traditional services. Someone who knows the language, values and nuances of those communities obviously has a better understanding of the resources and the possibilities. This equips them to be more effective in helping others become a valued member of their community.
7. Progressive. Peer support is not a static friendship, but progressive mutual support in a shared journey of discovery. The peer is not just a ‘buddy’, but a travelling companion, with both travellers learning new skills, developing new resources and reframing challenges as opportunities for finding new solutions.
8. Safe. Supportive peer relationships involve the negotiation of what emotional safety means to both parties. This can be achieved by discovering what makes each other feel unsafe, sharing rules of confidentiality, demonstrating compassion, authenticity and a nonjudgemental attitude and acknowledging that neither has all the answers.
IMPACT OF PEER WORKERS
Although there has been relatively limited research into the effectiveness of peer support, the studies that have been published paint a positive picture of the benefits. These benefits can be considered from a number of different perspectives.
Benefits to the worker
Studies of the experiences of peer support workers report many challenges to the role which need to be identified and addressed (see below), but these are outweighed by the potential benefits. They feel empowered in their own recovery journey (Salzer & Shear, 2002) have greater confidence and selfesteem (Ratzlaff et al., 2006) and a more positive sense of identity, they feel less selfstigmatisation, have more skills, more money and feel more valued (Bracke et al., 2008). Being employed as a peer worker is generally seen as a positive and safe way to re-enter the job market and thus resume a key social role (Mowbray et al., 1998).
“I work hard to keep myself well now, I’ve got a reason to look after myself better… It’s made a real big difference to me, you know, contributing something to them. And hopefully changing their lives for the better”.
Benefits to the people being supported
“Peer workers have the time and flexibility to listen. They always take the time to talk, whereas other staff members may get called away”.
Research into the impact of peer support on the people being supported includes seven randomised controlled trials and many more observational, qualitative and naturalistic comparison studies (Davidson et al., 2012; Repper & Carter, 2010; Bradstreet, 2006). Overall, these indicate that if peer workers are well trained and supported and employed in a recovery focused service where peer to peer supervision is available, they have the potential to bring a range of benefits to those receiving support, including:
- increased self-esteem and confidence
- improved problem-solving skills
- increased sense of empowerment
- improved access to work and education
- more friends, better relationships, more confidence in social settings
- greater feelings of being accepted and understood (and liked)
- reduced self stigmatisation
- greater hopefulness about their own potential
- more positive feelings about the future.
Of course, not all studies show all these benefits and it depends a lot on how well the peer support workers are selected, trained and supported and how well the organisation is prepared. Nevertheless, the potential benefits are certainly huge and it seems that peer support workers can make a significant contribution to enhancing the experience of care (subjective quality).
In this country, an area where experience of care has consistently been shown to be very poor has been acute inpatient admission (Mind, 2012; Care Quality Commission, 2009; SCMH, 1998). Thus, it is particularly important to evaluate the effects of adding peer support workers to acute inpatient teams. In the USA, Recovery Innovations have found that, over time, the addition of trained peers can improve the subjective quality of the service, reduce coercion and the use of physical restraints (Ashcraft & Anthony, 2008). By selectively reviewing the evidence on this topic we have found that adding peer support workers to the acute pathway can also shorten lengths of admission and reduce re-admission rates leading to significant cost savings (Trachtenberg et al., 2013). This is clearly an important area for further study.
Benefits to the teams in which they work
“I just stand back and watch him work his magic. Not just with the patients who come in here so frightened and hopeless, but with staff too. He can help them see things in a completely different way.”
The introduction of peer workers is a powerful way of driving forward a recovery-focused approach within a team. Just as peer workers provide hope and inspiration for others experiencing mental health problems, they challenge negative attitudes of staff and provide an inspiration for all members of the team. Peer workers also facilitate a better understanding between the people providing the service and those using it (Repper & Watson, 2012). As this team leader said:
“Peer workers have significantly changed the recovery focus of our team, they challenge the way we talk about people from a problem and diagnosis focus to one of strengths and possibilities” (Politt et al., 2012).
Benefits to the organisation
“The values and leadership of consumers are driving the shift from a system focused on symptom reduction and custodial care to self-directed recovery built on individual strengths…” (SAMSHA 2005).
Peer workers can also use their personal experience to influence organisational policies, procedures and behaviours. The fact that they have found ways of recovering a contributing role challenges some of the beliefs that underpin the system. For example, if an organisation is to employ peer workers, then human resources departments will need to reconsider general recruitment and selection policies and the use of Criminal Records Bureau (CRB) checks. Similarly, the recruitment of peer workers may highlight the need for occupational health procedures to be strengthened in relation to staff with health work problems arising from mental health issues. Thus, processes for supporting staff and improving wellbeing may be improved not just for peers, but for the whole workforce (Perkins, Rinaldi & Hardisty, 2010).
Where peer workers are active in decision-making bodies throughout the organisation they can challenge negative assumptions, counter risk-aversive behaviour and point out discriminating language and excluding practices. Finally, peer workers stand as a living testimony to the potential of everyone with mental health problems to recover and to contribute in a significant way to the services they receive. They demonstrate the role that services can play in this if they can make the right opportunities available. The employment of peer workers in itself therefore drives change towards more recovery-focused organisations.
MAINTAINING INTEGRITY
The ImROC programme has been particularly concerned with the establishment of peer support workers in paid posts within formal mental health services (e.g. in the NHS and other provider organisations). This is because of the multiple benefits to this approach described above. However, this approach has also been criticised for ‘professionalising’ the peer role, with risks of over-controlling the natural and spontaneous relationship that is at the heart of the helping process (Faulkner & Kalathil, 2012). This is clearly a danger. But there is also a danger in not formalising the role. When people are employed in large, bureaucratic organisations, there are perhaps even greater dangers of the role being blurred and people being exploited as ‘cheap labour’. The trappings of formality – job descriptions, managers, individual review – thus provide safeguards as well as risks.
The most effective way of retaining the essence of peer support is to identify its core values and ensure that these are upheld through recruitment, training and supervision. Of course, formal processes do not guarantee that the role will be allowed to develop in a creative and sensitive way, but they do provide a framework within which this is possible and within which distortions – should they occur – can be clearly identified.
A number of other organisational challenges have been identified which can potentially get in the way of peer support workers being able to make their maximum contribution. These include:
- engaging managers to support and understand the role
- treating peer workers as staff colleagues, not ‘patients’
- enabling peer workers to meet organisational demands such as administration and record keeping
- ensuring that peers take appropriate responsibility for their own wellbeing
- placing peers appropriately so that they are not put in positions which are too stressful or isolated
- allowing peers to work to their full potential by utilising both lived experience and life skills
- ensuring that peers have the support, skills and confidence to challenge poor practice in an appropriate manner
- ensuring that peer workers have the training and ongoing support to disclose personal information appropriately
- supporting peers to negotiate ‘reasonable adjustments’ in the workplace so that they can work to their full potential
- ensuring that all staff have access to the same support for their personal wellbeing as peers do.
This is a daunting list, but it reminds us that although the introduction of peer support workers can have enormous benefits for organisations, but it is also difficult and complex and easy to get wrong. The key to integrity remains the commitment to our core principles: mutuality, reciprocity, non-directive, recovery-focused, person-centred, strengths-based, community-facing and safe. It is these that we must aspire to maintain.
CONCLUSIONS
We have argued strongly for the value of establishing peer support roles to promote recovery in mental health organisations. Peers bring unique experience and a unique set of skills which can be deployed across a range of settings to provide hope, inspiration and influence for staff and service users alike. Their potential contribution is now recognised by policy makers and governments across the world. The research base is also growing and confirming that peers, appropriately recruited, trained and supported can have multiple benefits, for those providing the service, for those receiving it and for the organisations themselves. There is even beginning to be some evidence that peers, working alongside traditional professionals, can be highly cost effective and reduce demands on other services. However, we have also noted that the establishment of peer support roles is not without significant difficulties and it is easy to make mistakes. How can some of the practical difficulties of establishing peer support workers be addressed? This is the topic for the next paper, to be published this summer.
REFERENCES
Adams, A. L. & Leitner, L. M. (2008) Breaking out of the mainstream: The evolution of peer support alternatives to the Mental Health System. Ethical Human Psychology and Psychiatry, 10(3), 146-162.
Ashcroft, L. & Anthony, W. (2008) Eliminating Seclusion and Restraint in Recovery-Oriented Crisis Services. Psychiatric Services, 59, 1198- 1202.
Bracke, P., Christiaens, W. & Verhaeghe, M. (2008) Self-Esteem, Self-Efficacy, and the Balance of Peer Support Among Persons With Chronic Mental Health Problems. Journal of Applied Social Psychology, 38(2), pp.436-459.
Bradstreet, S. (2006) Harnessing the ‘lived experience’. Formalising peer support approaches to promote recovery. Mental Health Review, 11, 2-6.
Care Quality Commission (2009) Mental health acute inpatient services survey. Available from: http://archive.cqc.org.uk/aboutcqc/howwedoit/involvingpeoplewhouseservices/patientsurveys/mentalhealthservices.cfm
Castelein, S., Bruggeman, R. J., van Busschbach, J. T., van der Gaag, M., Stant, A. D., Knegtering, H. & Wiersma, D. (2008) The effectiveness of peer support groups in psychosis: a randomized controlled trial. Acta Psychiatrica Scandinavica, 118, 64-72.
Daniels, A., Grant, E., Filson, N., Powell, I., Fricks, L., & Goodale, L. (2010) Pillars of Peer Support: Transforming Mental Health systems of Care through Peer Support Services. Available from: www.pillarsofpeersupport.org
Davidson, L., Bellamy, C., Guy, K. & Miller, R. (2012) Peer support among persons with severe mental illnesses: a review of evidence and experience. World Psychiatry, 11, 123-128.
Department of Health (2010) Putting People First: Planning together – peer support and self directed support. London: Department of Health.
Department of Health (2011) No Health without Mental Health: A cross-government mental health outcomes strategy for people of all ages. London: Department of Health.
Department of Health (2012) No Health without Mental Health: Implementation Framework. London: Department of Health.
Faulkner, A. & Kalathil, K. (2012) The freedom to be, the chance to dream: Preserving user-led peer support in mental health. Together: London.
Franke, C., Paton, B. & Gassner, L.(2010) Implementing mental health peer support: a South Australian experience. Australian Journal Primary Health. 16(2):179–86.
Joint Commissioning Panel for Mental Health (2012) Guidance for commissioners of primary mental health care services. London: Royal College of Psychiatrists.
Mead, S., Hilton, D. & Curtis, L. (2001) Peer support: A theoretical perspective. Psychiatric Rehabilitation Journal, 25(2), 134-141.
Mental Health Foundation (2012) Peer Support in mental health and learning disability. London: Mental Health Foundation, Need 2 Know publications.
Mind (2012) Listening to Experience: An Independent Inquiry into Acute and Crisis Care. London: Mind Publications.
Mowbray, C., Moxley, D. & Colllins, M. (1998) Consumer as mental health providers: first person accounts of benefits and limitations. The Journal of Behavioural Health Services & Research, 25(4), 397-411.
Perkins, R., Rinaldi, M. & Hardisty, J. (2010) Harnessing the expertise of experience: increasing access to employment within mental health services for people who have themselves experienced mental health problems, Diversity in Health and Care; 7, 13-21
Perkins, R., Repper, J., Rinaldi, M. & Brown, H. (2012) Recovery Colleges. London: Centre for Mental Health.
Pollitt, A., Winpenney, E., Newbould, J., Celia, C., Ling, T. & Scraggs, E. (2012) Evaluation of the peer worker programme of Cambridge and Peterborough NHS Foundation Trust. Rand Europe.
Ratzlaff, S., McDiarmid, D., Marty, D. & Rapp, C. (2006) ‘The Kansas consumer as provider program: measuring the effects of a supported education initiative’, Psychiatric Rehabilitation Journal, 29(3), 174-182.
Repper, J. & Carter, T. (2010) Using personal experience to support others with similar difficulties: A review of the literature on peer support in mental health services. London: Together/University of Nottingham/NSUN.
Repper, J. & Watson, E. (2012) A year of peer support in Nottingham: lessons learned. The Journal of Mental Health Training, Education and Practice, 7(2), pp.70-78.
Salzer, M. & Shear, S. (2002) Identifying consumer-provider benefits in evaluations of consumer-delivered services. Psychiatric Rehabilitation Journal, 25(3), 281-288.
SAMHSA (2005) Building a foundation for Recovery. A Community Education guide on Establishing Medicaid funded Peer Support Services and a Peer Trained Workforce. Rockville, MD: Center for Mental Health Services, Substance Abuse and Mental Health Services Administration.
Sainsbury Centre for Mental Health (1998) Acute Problems. A survey of the Quality of Care in Acute Psychiatric Wards. London: Sainsbury Centre for Mental Health.
The Schizophrenia Commission (2012) The Abandoned Illness. London: The Schizophrenia Commission.
Scott, A., Doughty, C. & Kahi, H. (2011) Peer Support Practice in Aotearoa, New Zealand. Christchurch, New Zealand: University of Canterbury.
Scottish Recovery Network (2011) Experts by Experience: Guidelines to support the development of Peer Worker roles in the mental health sector. Available at: http://www.scottishrecovery.net
Shepherd, G., Boardman, J. & Slade, M. (2008) Making Recovery a Reality. London: Sainsbury Centre for Mental Health. Shepherd, G., Boardman, J. & Burns, M. (2010) Implementing Recovery – A methodology for organisational change. London: Sainsbury Centre for Mental Health.
Stroul, B. (1993) Rehabilitation in community support systems. In Flexer, R. & Solomon, P. (Eds) Psychiatric Rehabilitation in Practice. Boston: Andover Medical Publishers.
Trachtenberg, M., Parsonage, M., Shepherd, G. & Boardman, J. (2013) Peer support in mental health care: is it good value for money? London: Centre for Mental Health. In press.
University of Nottingham (unpublished) Evaluation of the Closing the Gap Peer Support Work project.
Peer support workers: theory and practice
This briefing paper has been produced for the Implementing Recovery through Organisational Change programme, a joint initiative from the Centre for Mental Health and the NHS Confederation’s Mental Health Network.
The pilot phase of ImROC ran from 2011-12 and was supported by the Department of Health, together with contributions from the participating services. The continuing work of ImROC is endorsed by the Department of Health and managed and supported by the Centre for Mental Health and Mental Health Network.
For more information on the current work of ImROC, please visit imroc.org.
ImROC, c/o Mental Health Network, NHS Confederation, 50 Broadway, London, SW1H 0DB
Tel: 020 7799 6666
imroc@nhsconfed.org
imroc.org
23. Building Community Partnerships to support people to Live Well: Creative Minds
Phil Waters – Strategic Lead for Creative Minds and Julie Repper – Director (Strategy, Innovation and Development), ImROC
Introduction
Dr Steven Michael OBE, ImROC Chair of Trustees
Throughout my career working in mental health services I have seen how helpful creative activity can be in supporting people (including myself) to stay well. These activities provide a sense of peace, creativity, purpose, achievement and connection for people who have lost confidence and a purpose and meaning in life. As CEO of South West Yorkshire Partnership NHS Foundation Trust our mission, informed and co-produced by local people, was to help people realise their potential and live well in their own communities.
Within these communities there are so many opportunities for people to join together in local groups and facilities to make art, poetry, film, to join knitting groups, craft circles, pottery workshops, choirs and music groups. For those who seek connection through more active pursuits there are walking, climbing, sailing, sports, cultural, political and faith groups.
I was fully aware of the limitations of health services in supporting people to rebuild their lives and wanted to find a way of linking all those using mental health services with communities of their choice. The seeds of this idea germinated in my own mind to become Creative Minds.
In practice the network (or movement) has been led and supported by hundreds of local people, some of them who use services, some work in services, but with the vast majority simply doing the things they enjoy doing in their communities. This paper describes the development of Creative Minds, how it works, who is involved, what difference it makes and how others might take these community focused innovations forward in their own localities. Creative Minds is developing a package of support to organisations who wish to follow a similar route of development with contacts on the final page of this paper.
Fundamentally all of our mental health is sustained by our connections with others. The Creative Minds approach has the power to enable, engage and empower these connections.
The Power of Community
Communities are an essential part of all of our lives. They include the neighbourhoods we live in, the groups that we connect with, the activities that we engage in, the people who we relate to. They include places, people, organisations, services, groups beliefs and interests. They are mobile, agile and, as shown so remarkably during the CoVID-19 pandemic, they can come together to overcome challenges and support each other. They have knowledge, skills, time, space, ideas and assets and they are essential for us all to live well. The Community Mental Health Framework for Adults and Older Adults (2019) recognises that communities are central to good mental health.
It aims ‘to enable healthcare providers and commissioners, STPs, ICSs, Primary Care Networks and people who use and have experience of services to work together to deliver a model that reinvigorates community provision and fully utilises the resources of the wider community’ with individuals ‘contributing to and participating in the communities that sustain them, to whatever extent is comfortable to them’. It recommends ‘strengthening relationships with local community groups and the VCSE to support the adoption of more rights-based care based on greater choice and engaging early with communities to address inequalities’; and ‘creating effective links with community assets to support and enable people to become more embedded within their community and to use these assets to support their mental health’.
Although the naturally occurring benefits of community engagement and development are rarely measured, there is increasing evidence of the potential that exists in communities. Pollard et al (2021, p.10) summarise the benefits of community power as:
• Improving individual health and wellbeing though people being active participants in all efforts to improve health and wellbeing.
• Strengthening community wellbeing and resilience as people are engaged in decision making and enabled (with resources and infrastructure support) to take action locally.
• Enhancing democratic participation and trust by coproducing decision making with local citizens and organisations at local level.
• Building community cohesion from the ground up by anchoring engagement and participatory approaches at a local level taking local history, strengths and challenges into account.
• Embedding and early intervention across all public services – education, transport, criminal justice as well as health and social care.
• Generating financial savings by reducing reliance on statutory services and enhancing confidence and capability at individual and community levels.
How can health and social care services work with communities for the benefit of local people?
The questions that remain for those health and social care providers that have increasingly – often inadvertently – tried to replace the role of communities through the provision of segregated spaces such as day centres or prescribe a role for communities as a step-down facility for those leaving services, is just how to support the central role of communities. How to access the power of communities and how to work collaboratively with the huge range of community assets and resources rather than exploiting, overpowering or ignoring the facilities, roles, relationships and activities that give life meaning and are central to living well. Or, as Russell summarises this challenge, how do we debunk the belief …’that institutions are the primary producers of what we need to live a good life of prosperity and well-being by repositioning and re-centring regular people and their communities and recognising them as the primary producers and contributors of those things that lead to increased well-being and health’ (Russell, 2023).
There already exist tried and tested approaches to realise or release the power of communities. ImROC has previously described the power of a local coproduction forum with local citizens, organisations and services as a means of sharing intelligence about what exists where, identifying gaps in provision and resources and fully participating in decisions about local community development. We have also demonstrated the benefits of employing peer support workers to enable people who are excluded, isolated and inactive to engage in activities, relationships and facilities of their choice; the power of social prescribing services to link people with local resources; and the impact of building competence and confidence of local communities’ resources to accommodate people with particular needs (Live Well paper 16. Developing Primary Care Networks and Community Focused Approaches: A Case Study – ImROC – Implementing Recovery through Organisational Change) (Repper et al 2019).
This paper describes a different approach to community engagement and development. One which facilitates the power and resources in local communities in order to improve opportunities for people with mental health challenges to both participate in and contribute to meaningful activities, relationships and facilities of their choice in their communities.
What is Creative Minds?
Creative Minds was set up in 2011 to support the development and delivery of creative arts, sports, recreation and leisure-based projects to improve the lives of people who use South West Yorkshire Partnership NHS Foundation Trust (SWYPFT) services. Creative Minds has developed into a charity hosted by SWYPFT with over 120 community partners developing over a 1000 community-based partnership projects across the footprint covering Barnsley, Calderdale, Kirklees and Wakefield. These projects offer opportunities for people who use/ have previously used SWYPFT physical and mental health services (including Yorkshire and Humber Forensic Secure Services) and build the confidence, competence and capacity of local communities.
We know that the context in which people live their lives is the most important determinant of life expectancy, and our ambition is to make sure that every person experiencing health issues using the local NHS organisation has the opportunity to engage with meaningful activities in their community and achieve their potential. Many people readily engage with NHS services – and Creative Minds activities are complementary to the service offer. However, for people who avoid using services, reject their diagnosis, and/or disagree with a medical approach, Creative Minds offers complementary and alternative approaches in the community. By having one foot in the NHS and one foot outside, Creative Minds can get alongside individuals who use services and support them to connect with meaningful activities in their communities and neighbourhoods that help individuals to regain, hope, meaning and fulfil their potential.
Creative Minds is the broker or the bridge between the SWYPFT and the communities it serves. It seeks to remove the barriers that inhibit partnership working. Traditionally, community organisations and groups have found it difficult to work directly with the Trust due to slow decision-making processes, difficult payment systems, risk averse attitudes and a culture that may not recognise the value of creative approaches. Creative Minds’ approach is very much based on community development principles and asset-based approaches and operates more like a social movement, that empowers local communities to be part of decision making and development.
A major aim of Creative Minds is to build a strong infrastructure of community and voluntary organisations, providing communitybased activities and relationships for all those who wish to engage with them, starting with those who access NHS services in the SWYPT footprint. Creative Minds works in partnership with individuals and groups in the community to coproduce opportunities for people to engage in activities that are meaningful and fulfilling to them. It supports the development of projects through mentorship and guidance to enable them to access external and Trust funds and to enhance both inclusivity and confidence to enable people with long term condition and challenges to fully participate. The passion and commitment to creative approaches that are held by the network of external champions helped bring Creative Minds to life. Champions also work within SWYPFT to support the development of projects, allocated according to their geographical locality and their areas of interest.
Inception of Creative Minds
Creative Minds grew out of a series of workshops that brought SWYPFT service users/carers staff and community partners together to gain a broader understanding of the needs of the population served by SWYPFT. Feedback stressed that engagement in creative activity can be invaluable in recovering a meaningful life, and that this was best provided in a safe, supportive environment. Participants felt that more creative projects would be initiated – and those already in existence would become more accessible – with support to set up and get started. And individuals currently using Trust services felt they could benefit from some initial practical and emotional support to engage in activities. However, there was agreement that projects would find ways of running independently in the longer term, just as participants would gain confidence over time. The workshop feedback generated an approach in which as participants engaged in activities they could begin to imagine a different life for themselves and move from the narrow confines and definitions of life as a receiver of healthcare towards new horizons as a contributing citizen. Creative engagement was also seen as an opportunity for people to partner as equals, to shift the power imbalance between care providers and the cared for, and for people to progress towards personal autonomy through developing a creative passion.
From these workshops in 2011, the Trust committed £200,000 funding to match fund community-based projects to improve inclusion and support for people with ongoing mental and physical health conditions.
Aims, objectives and values of Creative Minds
The agreed aim of Creative Minds is to develop access and take up of creative activities to improve the wellbeing of participants by increasing their self-esteem so they feel confident to try new things, develop social skills as they meet new people and feel a new sense of purpose and confidence as they engage in activity that they find meaningful and fulfilling.
Creative Minds’ objectives are to:
• Increase participation in creative activities for people who use Trust services.
• Coproduce quality creative practice and approaches within community based organisation.
• Increase inter-agency partnerships and bring in more funding for creativity and wellbeing.
• Develop a research/evidence base regarding creative approaches in relation to health, wellbeing and living well.
The values of Creative Minds are the guiding principles of all they do. Coproduction lies at the heart of their approach, from the way they developed to the way collective decision making continues to drive project development. Co-producing creative projects adds substantial value to the Trust’s overall service offer by exploring areas beyond its current provision and co-creating new and innovative solutions to the issues faced by individuals and communities. The approach builds and uses social capital to create and restore a community spirit that enables people to reach their potential and live well in their communities, which is the Trust’s coproduced Mission. Working and delivering services in partnership has large mutual benefit for all as people learn from each other: community organisations and groups have greater awareness of mental and physical health conditions and the Trust learns more about creative approaches and how community organisations operate. Creative Minds offers more opportunities for people who use services to join activities alongside people who don’t use services as equals. This reduces discrimination self-stigmatisation and builds confidence and capabilities for all.
Staffing of Creative Minds
The Creative Minds strategy was originally developed with the Trust’s Equality and Inclusion team who facilitated coproduction workshops to agree a strategy to drive the early initiatives. As projects grew in popularity it was clear that the approach was becoming an entity in its own right and in 2015 Creative Minds became a registered charity. The Trust supported a business case to create a separate staffing structure to manage and develop Creative Minds projects and to explore the potential to expand the approach and draw down new sources of funding. At this stage an independent staffing structure was agreed including: a Strategic Lead, four Development Coordinators and Project worker to support the development of Peer Led Projects. A growing number of volunteer Champions became involved through the strategy workshops and stayed with the development and decision-making process. These Champions included people using services and staff working in teams who had a passion for creative activities and helped to build strong pathways to connect with people using services and codeliver some of the projects. These now amount to 4-500 people who have a firm connection to support the work and can be described as a social movement. Additional funding allowed for two Creative Practitioners posts and four project worker posts.
How Creative Minds supports projects
In line with the organisation’s values and Equality and Inclusion roots, processes around development and decision making have always been inclusive. Collective decision-making groups were established in each of the Trust’s localities in Barnsley, Calderdale, Kirklees and Wakefield. The collectives continue to be made up of people with lived experience, carers, Trust Staff and community representatives and they manage the locality share of the funding. Young Foundations Community Development tool (Osbourne et al, 2021) is used to support project development which builds on strengths and targets support to any area’s weakness. The collectives continually identify and respond to gaps and needs in their local community and ensure that projects are targeted on those in the greatest need. The collectives are always open to new members to ensure strong pathways are created and any barriers to a project working are quickly identified and addressed.
Case Vignette 1: Partnership with Barnsley Football Clubs’ charity Reds in the Community
Barnsley FC wanted to make the club more dementia friendly, believing that if people with dementia could keep coming to the club it would be good for their wellbeing. They also felt the club’s historical archive would make a great basis for a memory group. The response from services was, “what do Barnsley football club know about dementia” our view was ‘ quite a bit!’. Through working with the club’s charity, we brokered a meeting and we persuaded services to get involved and Creative Minds matched the funding the club had raised and the work started. The initial project was a big success working with the Trust’s memory team and since then other approaches have developed including walking football and creative writing. The creative writing and poetry from the groups is now on permanent display at the club’s main entrance and forms part of their dementia awareness raising campaign and part of making the club more friendly to people with dementia. More recently we have developed Safety Nets a health and wellbeing programme that takes young people off the CAMHS waiting list. The coaches from the club provide physical activities combined with wellbeing session from CAMHS staff, the programme on average sees a 30-40% increase in the Shorter Warwick and Edinburgh Mental Wellbeing Scale. Barnsley CAMHS said;
“We get very positive outcomes and feedback resulting from delivery of these projects, many participants reporting life changing experiences and many young people want to stay on as volunteers and are less reliant on service”
How Creative Minds supports individuals
The projects developed and delivered through partners, complement and enhance the services that people receive from the NHS and support their recovery. They also offer an alternative for people who do not engage readily with statutory services. These are often people who suffer the most in terms of health inequalities. The loneliness and social isolation that people were feeling has been compounded by Covid 19 which exacerbated the challenges and issues that people have in managing their mental and physical health and wellbeing.
Case Vignette 2: “I would have ended up on the streets” – Babur’s story
In his late teens, Babur experienced anxiety and depression which ultimately led to him to being given medication and referred into the Calderdale insight team at the Trust. Working with the team, Creative Minds developed and funded a rock-climbing scheme that people who use services could access. Babur began his rock-climbing journey here, as part of his treatment, and hasn’t looked back since! Babur is now in full-time work and completed his rock-climbing instructor training. Babur wanted to give back to the service and Creative Minds so he now volunteers for the insight team and supports Creative Minds projects, including running weekly climbing groups and other outdoor pursuits. Babur gets to share his lived experience with people that use Trust services and share his recovery story with people whose shoes he was once in. Babur’s general health and fitness is also much improved as his diet and exercise are now designed to build upper body strength so he can climb better. Babur’s story is one of hundreds of examples of how Creative Minds has worked with the Trust to improve patient experience and outcomes. You can also hear from Babur on his personal experience through this film here.
Freedom to be agile and innovative
Although Creative Minds is hosted by the NHS, it is a charity in its own right. This brings a number of benefits. First bespoke relationships with community organisations can be developed, operating in a flexible and agile manner unencumbered by some of the bureaucracy that can stymie creativity in large statutory organisations. Second, being hosted by the NHS gives more influence within the local health care system than coming from an external position would offer.
Case Vignette 3: Extending Creativity into decision making processes
A number of Creative Minds’ partners tried to work with the Trust previously and the decision-making process to achieve matched funding for a project took 3-4 months. However, the funding was only available for a 1-month period which precluded the possibility of success. Creative Minds partnership agreements allow partners to become preferred suppliers and set up a process that enabled community organisations to plan project development. Projects are also more successful with support from staff champions, who hold a big influence on changing organisational culture more positively towards creative activities. This arrangement also included using Trust budgets in more creative ways when recruitment had been difficult, leading to more creative activities being delivered on inpatient wards.
Case Vignette 4: Innovation in Action
Creative Minds have been working with Public Health in Barnsley, to develop a community accreditation scheme to enable local sports and recreation clubs to become more mental health friendly and provide a more supportive environment for people who have mental health issues. Part of the scheme is to provide the clubs with mental health awareness and Mental Health First Aid training. The initiative has been promoted with a ‘Moving Mental Health Forward’ logo that has been adopted by Barnsley Council. Creative Minds are starting to build pathways for people from secondary Mental Health Services to enable a more guided route for people might struggle to engage with the clubs. Benefits of being active
Impact of Creative Minds
Creative Minds supports the development of projects that welcome people with ongoing mental and physical health challenges. In so doing the organisation believes Creative Minds reduces loneliness, social isolation and inactivity and the associated loss of confidence, poor self-esteem and feelings of negativity. Thus, these projects serve to build emotional resilience, providing healthy boundaries, supportive peers, self-awareness, and openness to change. Increased resilience keeps people well and able to cope with life challenges, reducing the risk of them needing NHS services. Creative Minds meet people every day who recount their own positive stories so are convinced of the benefits to their approach. However there is relatively little ‘gold standard’ research evidence to demonstrate the benefits of the approach.
A new means of evaluating creative activities has been embraced. A peer-led network of Community Reporters was trained to collect stories from participants of creative activities, to evaluate creative activities and provide new insights into why participants feel these activities are important to mental health recovery and wellbeing. This new approach to evaluation was to support people to tell and share stories of their experience of using creative approaches to recovery and/ or wellbeing through Community Reporting. Community Reporting is a storytelling movement that was started in 2007 by People’s Voice Media and it uses digital tools such as portable and pocket technologies (tablets, smart phones) to support people to tell their own stories in their own ways. Central to the approach is the belief that people telling authentic stories about their own lived experience offers a valuable understanding of their lives. Participants also complete a shortened version of the Warwick & Edinburgh Mental Wellbeing Scale and, on average, people engaging with Creative Minds demonstrate a 40% Improvement in their WemWebs score. (Give exact results).
Community Reporting has published summaries of peer led and collaborative evaluations of different Creative Minds projects https://communityreporter.net/ feature/sport-and-wellbeing-good-moodleague and https://communityreporter. net/story/soft-and-fluffy-friday-7-february2020-137pm.
These reports show how project groups establish healthy boundaries to focus on the activity, not an individual’s problems, participants share ground rules and develop social norms. Project groups increase participants confidence and their ability to make and maintain healthy relationships with their peers. It also gives them lived experience of relationships based on shared interest. Groups are a safe environment where participants can test out relationship building skills and establish social networks that support them. This creates a ‘healthy interdependence’ and begins to create and extend social networks. Participation in the creative groups raise aspirations and hope, people with higher aspirations achieve more and work to extend their abilities.
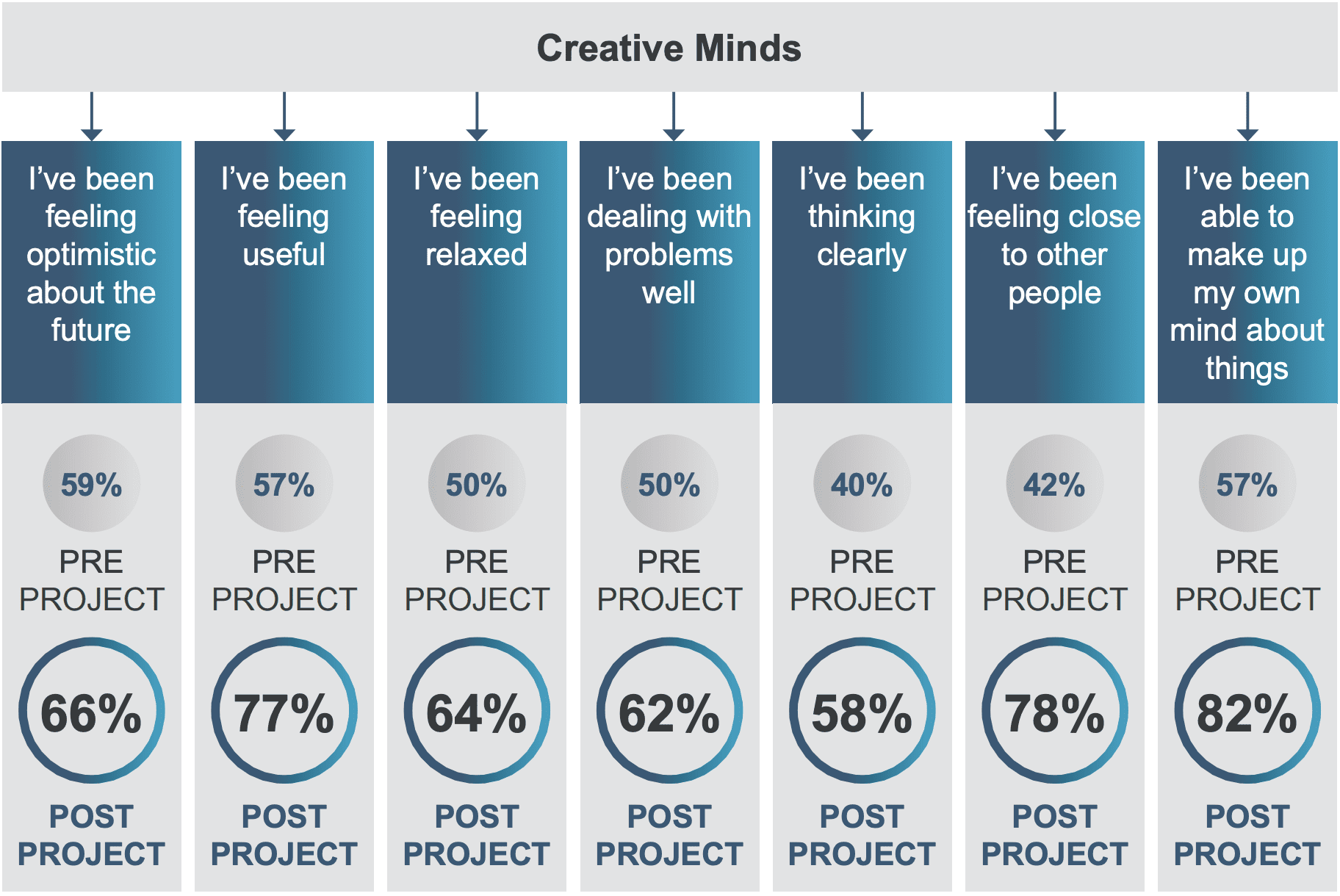
Creative Minds Evaluation Results 2017/18
Attendees of all Creative Minds projects are invited to rate their thoughts and feelings before a project commences and 3 months into the project or when it ends: (134 people completed the evaluation in 2017/18)
Attendees are asked to describe what has changed in their life since attending a project:
Peer led projects
The area of work that involves beneficiaries the most is in the peer led projects that are supported by Creative Minds. Peer led projects are a priority area for development; where participants from an existing programme who develop a passion for a particular activity can go on to develop their own groups. Together a safe process has been developed whereby peerled groups are supported to set up a simple constitution and community bank account to get started. Where possible these groups are hosted by one of the Creative Minds’ partners to give an extra level of support to get peer groups established.
What difference has Creative Minds made on culture and practice inside and outside local mental health services?
A major aim of Creative Minds was to build a strong infrastructure of community and voluntary organisations to work with to provide excellent creative projects for all who access NHS services. Therefore, to the conception and development of Creative Minds. It not only shows commitment, as an organisation, to having a creative approach to service delivery but also showcases passion for working in partnership with communities. Creative Minds has provided a way to not only build on existing good practice in NHS services, but also to work more closely with a wide range of community organisations enhancing service provision by delivering innovative, transformative and meaningful health and wellbeing projects. The passion and commitment of external champions to creative approaches has helped to bring Creative Minds to life. This infrastructure helps to embed this different way of working across all aspects of the organisation’s work.
Projects are offered that are suitable and targeted toward people who use SWYPFT services including those with a mental and or physical health diagnosis and people with a learning disability. The projects are generally open to all age groups, but there are some projects that are age and condition specific to ensure they are more suited to groups with particular needs. The group size is usually between 15-20 people, but some groups like the Art’s Café and the Good Mood Football league have up to a 100 people attending.
Within its health system, Creative Minds are creating a paradigm shift, from one that is about ‘doing to’, to one that is about creating the right conditions for individuals and collective groups and communities to do for themselves and each other. This requires a fundamental shift in power to people with lived experience and communities recognising them as equals in a relationship that creates value through meaning and hope. The principles and philosophy of Creative Minds seemed to strike a chord with many people in the NHS. It appears to have initiated a genuine social movement of which people want to be part, and for which people feel a sense of ownership.
This seems to resonate with people involved in Creative Minds and is evident from many more staff members becoming champions, but also people with lived experience wanting to get involved. This fits with theories being developed at the NHS Institute for Innovation and Improvement by Helen Bevan REF “The social movements perspective fundamentally challenges the ways that we have learnt to organise and lead change in the NHS. It advocates that healthcare improvement strategies need to extend beyond the topdown programme by programme approach to embrace a concept of citizen led change”
References
Bevan H (2011) Social Movement thinking: A set of ideas whose time has come? (accessed July 23)
NHSE (2019) The Community Mental Health Framework for Adults and Older Adults
Osbourne, L., Wallis, E., Stumbitz, B., Lyon, F. and Vickers, I. (2021) Pathways to good work: toolkit for community organisations. Case Study. Locality.
Pollard, G., Studdert, J. and Tiratelli L. (2021) Community Power: The Evidence. London: New Local.
Russell C. Understanding ground-up community development from a practice perspective. Lifestyle Med. 2022;e269.
https://doi.org/10.1002/lim2.69 Repper, J. (2019) Briefing Paper 17. The Live Well Model: Developing Primary Care Networks and Community focused approaches. ImROC: Nottingham
Snowden, D. and Boone, M. (2007). ‘A Leader’s Framework for Decision Making,’ Harvard Business Review, November 2007.
We strive to support organisations to co-produce their own pathways and training and become self-sufficient and successful in their Peer Support programmes.
ImROC provides many cost free resources to get you started in considering the multilevel preparation that might need to be considered when developing peer roles in your organisation. We know this includes:
- Recruitment, policy and HR prepared for the needs of lived experience folk
- Understanding how to run equitable recruitment, employment and development that reflects the demographic of the service reach
- Buy in from a strategic level
- Understanding of the peer role, how it thrives and what are the challenges.
- Team preparation for all teams welcoming peers
- Peer informed supervision
- A career path and progression for Peers
- Peer role descriptions reviewed for each team
- A critical mass of peers
- Designated people to run the peer programme, not just an add on
Influencing culture and practice to be more person centred and recovery focused is challenging. The ImROC team are here to offer you support to work through the unique hurdles and blocks each organisation could face.
Booking a free discovery call with one of our consultants and we can support you to explore what you might need to carry out your next steps.
Helpful Resources
Preparing for peers in organisations
The long-standing myth that mental health service providers, users and commissioners “can’t agree on what recovery is, nor offer any evidence for it” is finally laid to rest in this paper.
Supporting recovery in mental health services: quality and outcomes aims to help organisations in the mental health sector develop clear, empirically-informed statements about what constitutes high-quality services, and how these will lead to key recovery outcomes for service users. It also includes a series of recommendations for health and social care providers and commissioners, and for NHS England and the Government, that aim to support development of an evidence-based approach to commissioning mental health services.
Download 8. Supporting Recovery in Mental Health Services: Quality and Outcomes
8. Supporting Recovery in Mental Health Services: Quality and Outcomes
Geoff Shepherd, Jed Boardman, Miles Rinaldi and Glenn Roberts
INTRODUCTION
The development of mental health services which will support the recovery of those using them, their families, friends and carers is now a central theme in national and international policy (DH/HMG, 2011; Slade, 2009). In order to support these developments we need clear, empiricallyinformed statements of what constitutes high-quality services and how these will lead to key recovery outcomes. This is what the present paper aims to do.
We have had to be selective in terms of the evidence we have considered and, in many cases, we have had to make subjective judgements to come to simple recommendations. We understand that not everyone will agree with our conclusions. Nevertheless, we hope that, at the very least, they will provide a useful framework within which discussions about quality and outcome can take place at a local level in a more informed way. We therefore hope that the paper will be of value to both commissioners and providers.
A NOTE ON AUTHORSHIP
Advances in recovery-focused practice arise from new collaborative partnerships between the people who work in mental health services and the people who use them. The ImROC briefing papers draw upon this work. Where ideas are taken from published materials we cite them in the conventional form, but we also want to acknowledge the many unpublished discussions and conversations that have informed the creative development of the project as a whole over the last five years. Each paper in this series is written by those members of the project team best placed to lead on the topic, together with invited guest authors and contributions from other team members. On this occasion the authors would also like to acknowledge the contribution of Mike Slade and his colleagues in the REFOCUS group at the Institute of Psychiatry to this paper. Their careful research and generous willingness to share ideas has been invaluable to the thinking summarised here.
BACKGROUND
The ImROC programme (Implementing Recovery through Organisational Change) was established by the Department of Health in England in 2008 to help local services become more supportive of recovery for those using them and their carers (Shepherd et al., 2011). Arising from this work, we have described the basic principles of recovery (Shepherd, Boardman & Slade, 2008), presented a methodology for achieving organisational change in mental health services (Shepherd, Burns and Boardman, 2010), and described how key elements of more recovery-oriented services might be developed (Perkins et al., 2012; Alakheson & Perkins, 2012; Boardman & Friedli, 2012; Repper, 2013). Most recently, we have presented evidence for the potential cost effectiveness of services which employ formal, peer workers (Trachtenberg et al., 2013). However, we have not yet formally addressed the key issues of ‘quality’ and ‘outcomes’.
Quality indicators provide the key link between evidence-based practice and improved outcomes (McColl et al., 1998). Thus, if we can identify a set of indicators for which there is evidence that, if present in a service, they will lead to specific outcomes which support recovery then this gives us a way of assessing its quality as a ‘recoveryoriented’ service. This does not conflict with our fundamental belief that recovery belongs to the people who use mental health services and is embedded in their unique and individual lives. Judgements about ‘quality’ and ‘outcomes’ must therefore ultimately rest with them, but at the same time we recognise that clinicians and managers need information which will guide them to provide services to support recovery in the most effective and efficient ways. We recognise that this is an ambitious undertaking – quality in healthcare is always highly multi-facetted – nevertheless, we have attempted to describe a structure which will make these complicated ideas accessible to a non-specialist audience, as well as to mental health professionals, managers and commissioners.
Our primary focus has been on the experience of adults of working age using specialist mental health services. This should not be taken to imply that we are not interested in applying this thinking to services which support recovery in other groups, e.g. children, older people, those with mental health problems not in touch with specialist mental health services. Nor does our emphasis on quality and outcomes in formal services imply that we believe these are necessarily the most important sources of support for recovery. Often, these are friends, families, community groups, churches, etc. and this is evidenced repeatedly in the rich collections of life stories of people who are ‘in recovery’ (e.g. Davies et al., 2011). Their contribution should never be overlooked.
CURRENT ISSUES
As indicated above, the purpose of trying to identify valid quality indicators is to give commissioners and providers a basis for designing services that are most likely to produce certain outcomes. In the current climate this is becoming increasingly urgent as services in England struggle to categorise groups of patients with similar levels of need into different ‘clusters’ and then estimate the costs associated with effective care pathways for people who fall into these clusters. This system is known as Payment by Results (PBR) and it is intended that it will form the basis of new funding formulae for mental health services. Whether it will be successful or not is, at the moment, unclear. What is clear is that if recovery-supporting service developments are to be funded in the future, then recovery quality indicators need to be built into the care pathways in all the relevant clusters.
This in turn means that these indicators should have evidence for their association with outcomes comparable to those approaches described in the guidance for effective service provisions produced by the National Institute for Health and Care Excellence (NICE). This presents difficulties for recovery-oriented services because many of the elements are relatively new and the evidence base is therefore inherently limited (although not, as we shall see later, non-existent).
In addition to these attempts to specify quality indicators in the context of PBR cluster pathways, recent dramatic failures of care have given rise to a much greater emphasis on indicators which are not necessarily evidence-based, but reflect very basic criteria for compassionate and humane services (Francis, 2013). This renewed emphasis on the quality of supporting relationships is welcome and, as we shall see, it is highly consistent with recovery principles.
Given the complexity of the subject matter to be presented here, we have decided to take the unusual step of dividing the remainder of the paper into two. Part I contains a summary of the key indicators and recommendations for outcome measures. Part II contains a technical appendix which sets out additional detailed information to justify the quality and outcome measures recommended.
PART I. SUMMARY AND RECOMMENDATIONS
Quality indicators at an individual level
In terms of specifying quality indicators for recovery, it is useful to distinguish between service quality at the level of individual interactions and organisational level features. At an individual level, Slade and his colleagues in the REFOCUS group have made a further helpful distinction between ‘recovery-promoting relationships’ and ‘pro-recovery working practices’ (Bird et al., 2011). The former relates to the general quality of the therapeutic relationship and applies to all relationship-based interventions (this covers the kind of basic relationship factors referred to in the Francis Report (Francis, 2013)). The latter refers to a specific set of practices relating to the support of recovery. In addition to these, we can add a number of approaches which, although not necessarily derived directly from recovery ideas, are nevertheless highly consistent with supporting recovery for individuals. This set of individual level indicators is summarised in Box 1. The individual level quality indicators shown in Box 1 could easily be converted into a selfassessment tool for auditing services and could form part of the contract specification for providers.
Box 1: Quality indicators for supporting recovery at an individual level
Staff should aim to…
Facilitate recovery-promoting relationships
- establish shared values
- demonstrate good, basic relationships skills (empathy, warmth, respect)
- support personal hopes and aspirations
- promote a sense of control (‘agency’).
Use ‘pro-recovery working’ practices
- narrative accounts (recovery stories)
- a ‘strengths’ approach
- ‘coaching’ methods
- Personal Recovery Plans (WRAP, STAR)
- self-management
- shared decision-making
- person-centred ‘safety planning’.
Consider specific approaches which will support recovery not developed from a recovery perspective, e.g.
- Joint Crisis Plans (JCP)
- ‘Housing First’
- Individual Placement and Support (IPS)
- use of ‘personal budgets’ (social and health).
Recovery-promoting relationships
Relationships are at the heart of recovery. The creation of supportive relationships depends upon establishing shared values and demonstrating empathy, warmth, respect and a willingness to go the ‘extra mile’ (Borg & Kristiansen, 2004). These form the bedrock for all forms of care and, some would argue, have been undermined by the increasing ‘marketisation’ of healthcare with its emphasis on impersonal service transactions, rather than the relationships within which these transactions take place. Positive relationships are at the heart of basic, good care highlighted in the Francis Report (2013) and they also show considerable overlap with the NICE quality standards (NICE, 2011; 2013, see Technical Appendix). High quality, recovery-oriented services should also be consistent with the key recovery principles identified by Repper & Perkins (2003) – hope, control, and access to ‘opportunities to build a life beyond illness’.
Pro-recovery working practices
In terms of recovery-oriented practices, the starting point must be to encourage the person to tell their story. Narrative accounts are the oldest – and probably the most powerful – ways in which we make sense of the world and build relationships. Everyone has a story to tell and the process of storytelling is almost always experienced as positive and validating. Narratives are inherently meaningful and are expressed in a form and language that is accessible to everyone (Greenhalgh & Hurwitz, 1999). They also provide a source of information and explanation which is complementary to a conventional ‘evidence-based medicine’ approach (Roberts, 2000). We should therefore give the use of narrative accounts the central place in the practice of recovery that it deserves, both in helping people formulate goals and in monitoring outcomes (see below).
A second important practice is the consistent use of a ‘strengths’ approach (Rapp & Goscha, 2006). This seeks to identify the person’s competencies and their environmental resources (friends, neighbours, local opportunities) which might be used to further their personal life goals. The strengths assessment is often based on simply encouraging the person to tell their story as this can provide important clues to activities and interests that were pursued in the past which could be used again in the future. The ‘strengths approach’ therefore offers an important contrast to the ‘deficits model’ which has tended to dominate mental health practice up to now.
Another recovery-supporting practice, which has been developed in the last few years, is the ‘coaching’ model (Bora et al., 2010). This uses many of the same techniques as the strengths approach, e.g. an emphasis on the service user taking the lead, the importance of identifying personally-relevant goals, a focus on strengths and natural supports. However, there is greater emphasis on the importance of staff behaviour as a ‘coach’, or learning partner (‘on tap, not on top’) and on the service user’s responsibilities to make a commitment to action. Although there is good evidence for the effectiveness of coaching in relation to the management of long-term health conditions (O’Connor, Stacey & Legere, 2008) there is little evidence as yet regarding its specific effectiveness in relation to supporting recovery in mental health.
The use of narratives, building on strengths and a coaching approach can then form the starting point for the development of Personal Recovery Plans. These may be based on formal tools such as the ‘Wellness Recovery Action Plan’ (WRAP) (Copeland, 1997) or the Recovery STAR (McKeith & Burns, 2010) or simply developed from the person’s narratives or an analysis of their strengths. Whatever their derivation, Personal Recovery Plans should contain an identification of the person’s internal and external resources and a plan for how they can use these to take control of their life and achieve their chosen goals (Perkins & Rinaldi, 2007). The person should not necessarily have to share their recovery plan with staff: they belong to them. They are therefore not the same as ‘care plans’, although it is clearly desirable if there is as much overlap as possible between the two (Rinaldi & Watkeys, in press).
WRAP is a framework for developing a personal plan to cope with distressing symptoms, prevent relapse, manage crises and stay ‘well’. It was designed by a service user for service users. WRAP has been widely used in England and there are some good practical examples of the difficulties and benefits of implementation (Hill, Roberts & Igbrude, 2010). The Recovery STAR is also currently very popular. It contains ten ‘domains’ of recovery and the service user and staff member work together to rate each domain area on a ten point scale. The results are then presented visually on a Star diagram. This is an attractive, easy-to-understand, format and most service users seem to find the ten domains helpful for identifying personal goals, although some report that it needs to be more personalised. Both WRAP and the STAR are therefore useful methods for engaging people and assisting with personal recovery planning and monitoring individual progress. They are less useful as outcome measures (see below).
As indicated earlier, an important theme in most people’s recovery is the struggle to achieve a greater sense of control over their symptoms and their life in general. Thus, improving the person’s capacity for self-management is critically important. Self-management can refer to a wide variety of methods from simply handing out leaflets, to personal support through telephone monitoring, goal-setting, coaching and structured education. There is strong evidence, mainly from studies in the physical healthcare field, that supporting self-management can be extremely helpful in terms of ameliorating symptoms, improving quality of life, and reducing dependency on formal health care interventions (Foster et al., 2007; De Silva, 2011). Approaches which include full and active involvement of the person, rather than the passive provision of information, are also likely to be most effective. Thus, De Silva recommends, “a fundamental transformation of the patient-caregiver relationship into a collaborative partnership” (p.vi).
Mueser and his colleagues in the U.S. have developed a comprehensive educational and self-management package designed to provide people with severe mental illness with the information and skills necessary to manage their symptoms more effectively and work towards achieving personal recovery (Mueser et al., 2002). This has become popular in the U.S. and has attracted some interest in Europe. The ‘Illness Management and Recovery Programme’ (IMR) consists of five components:
- ‘psycho-education’ regarding severe mental illness
- the provision of information on medication and side effects, using a ‘motivational interviewing’ approach
- a relapse prevention programme
- training in coping skills and problem-solving
- a cognitive-behavioural approach to symptom management.
Preliminary findings have been published regarding its implementation in small samples in the U.S. and Australia (Mueser, et al., 2006; Salyers, 2006) and a randomized controlled trial found that service users appeared to have increased their knowledge of illness, coping skills, personal goal identification and attainment (Hasson-Ohayon et al., 2007). There was weaker evidence of improvements regarding hope and no significant gains regarding social support or help from others. Salyers et al. (2009) also evaluated a statewide implementation of IMR and found evidence of increased hope, but not satisfaction. Systematised programmes like IMR provide a good summary of basic information and give general tips on self-management but, viewed in the context of the De Silva (2011) review, IMR cannot be said to be an example of ‘co-production’. In our view, this is a vital missing ingredient.
Alongside self-management approaches, there has also been increasing interest in ‘shared-decision making’. This brings together two sources of expertise – the knowledge, skills and experience of health and social care professionals and the individual’s own knowledge and expertise of their own condition. Both forms of expertise are key to making good decisions. Used together they enable the person to make choices regarding treatment and management options that are most consistent with research evidence and with their own preferences and priorities. ‘Shared decision-making’ is therefore the basis of truly informed consent. There are a number of examples of the value of this approach in the physical healthcare field (e.g. Simon et al., 2009) and they are now beginning to be applied in mental health, particularly in relation to medication management (Deegan & Drake, 2008; Torrey & Drake, 2009; SAMSHA, 2011). A helpful article recently appeared ‘coproduced’ by service users, carers and professionals which sets these approaches clearly within the framework of recovery-oriented practice (Baker et al., 2014).
As a result of negative coverage in the media and perceived external pressures, the assessment and management of risk has become a prominent issue in mental health services. Many staff have become highly ‘risk averse’ and are reluctant to engage in what might have been seen in the past as ‘positive’ risk taking, i.e. working with service users to help them identify risk management strategies which are necessary in order to take pursue reasonable and realistic life goals. This has happened despite clear government guidance to the contrary (Department of Health, 2007). However, in the past few years recovery-oriented professionals have developed new approaches to managing risk which are based on working with the person to examine what risks may prevent them from pursuing their chosen life goals and then involving them fully in the development of a plan to support the pursuit of these goals in ways that are safe for them and those around them. This is known as person-centred ‘safety planning’ and will be the subject of a forthcoming Briefing paper (Boardman & Roberts, in press).
Approaches which support recovery not developed from a recovery perspective
In addition to these general ‘pro-recovery’ working practices, staff should also be trying to offer a number of specific approaches to help people in their recovery which have not been developed from a recovery perspective.
For most people their Personal Recovery Plan will involve them avoiding unnecessary admissions to hospital, particularly if these are compulsory under the Mental Health Act. The Joint Crisis Plan (JCP) is a relatively new invention which has been specifically developed to achieve these aims and is based on a process of co-production (Henderson et al., 2004). The JCP is formulated by the service user, together with peer support if available and the key mental health staff involved in their care, including the treating psychiatrist. It is therefore similar to an ‘advance statement ’, or the kind of crisis plan contained in WRAP, but with the crucial inclusion of the clinical staff and the treating psychiatrist in the formulation of the plan. In an initial randomised controlled trial, people who were discharged with a Joint Crisis Plan were shown subsequently to have significantly fewer compulsory admissions compared with controls (Henderson et al., 2004). Qualitative data also suggested that the JCP group felt more ‘in control’ of their mental health problems (Henderson et al., 2008). A second study produced less impressive results, but the authors acknowledge that this was mainly due to practical difficulties in ensuring that the joint planning meetings always occurred and were effectively facilitated (Thornicroft et al., 2013). The addition of peer support workers to inpatient teams may be one way of ensuring that JCPs are routinely offered.
Housing, employment and money are then the key building blocks in most people’s recovery and it is therefore important to ensure that effective methods for achieving these goals are available for everyone attending mental health services.
The ‘Housing First’ initiative was developed in the U.S. to meet the needs of homeless people with complex mental health and substance misuse problems. It prioritises the identification of suitable housing, based on personal preference, and then delivers other supportive services to the person once they are housed, without a pre-requisite that their substance misuse must cease first. The use of permanent housing options and the commitment to floating support means that the resident does not have to make continual moves between different types of accommodation as their support needs change. A four-year longitudinal study compared the ‘Housing First’ model with traditional ‘treatment first’ approach and found a significantly higher rate of retention for residents in the Housing First model (88% v. 47%, Padgett, Gulcur & Tsemberis, 2006). Despite there being no requirement for the Housing First group to abstain from substance misuse there was actually no significant difference between the two groups regarding their levels of drug and alcohol use. However, the annual per capita costs of the Housing First programme were around half those of ‘treatment first’ programmes. This approach is now being tried in England (Shelter, 2008) but is not widespread, often because of the lack of available housing alternatives.
The ‘Individual Placement and Support’ (IPS) approach has been designed to help people with severe mental health problems gain and retain paid employment. It has a number of similarities with the Housing First method. Thus, it is also based on placing the person in a work position of their choice as quickly as possible and then providing them and with an integrated package of vocational and clinical support in situ (Becker, Drake & Concord, 1994). There is now very strong evidence, both nationally and internationally, that IPS consistently achieves employment rates two to three times better than traditional alternatives such as pre-vocational training and sheltered workshops (Burns et al., 2007; Bond, Becker & Drake, 2008; Sainsbury Centre for Mental Health, 2009a). The one study where IPS failed to produce such impressive results was where it was not implemented with good fidelity to the research model (Howard et al., 2010; Latimer, 2010). Longer term follow-up studies of people placed through IPS suggest that the higher rates of employment are maintained and have positive impact on non-vocational outcomes – e.g. improved confidence and wellbeing, reduced sense of stigma. In addition, they are associated with reduced use of mental health services, leading to reduced costs (Sainsbury Centre for Mental Health, 2009b).
Finally, we should note the importance of money in the lives of people with mental heath problems (Parsonage, 2013). Personal budgets may be a source of supplementary income to help with specific social and vocational goals. There are still practical problems around the implementation of these personal budgets, mainly regarding their availability, bureaucracy involved and ensuring that resources are effectively targeted on those in greatest need, but the principle of providing someone with resources that they can choose to spend on what they think will help them must be correct. The use of personal budgets to support recovery is discussed in detail in Alakeson & Perkins (2012).
Quality indicators at an organisational level
The quality of support for individuals to pursue their recovery goals ultimately depends on the quality of care provided by individual staff in their everyday interactions. However, in order for these recovery-supporting relationships to be maintained, the organisation also needs to demonstrate its commitment to recovery principles and to creating a ‘recovery-supportive’ culture. How might this be measured?
Burgess et al. (2011) reported a systematic review of 11 instruments aimed at assessing the ‘recovery-orientation’ of organisations. They examined each measure in terms of its ease of use, whether or not it satisfactorily reflected a ‘consumer’ perspective and its psychometric properties. They ended by recommending just four:
- Recovery-Oriented Systems Indicators (ROSI)
- Recovery Self Assessment (RSA) tool
- Recovery-Oriented Practices Index (ROPI) (adapted for use in a British context as the ‘Scottish Recovery Indicator’)
- Recovery Promotion Fidelity Scale (RPFS).
(For details of these measures see the Technical Appendix).
All these instruments have advantages and disadvantages. All were developed in the U.S. or Australia and hence there are problems with cross-cultural application of specific items (Slade & Hayward, 2007). Most are also rather long and laborious to use. Some have reasonable inter-rater reliability and concurrent validity, but the test-retest reliability has generally not been thoroughly investigated. This is a key limitation in tools designed to measure change as it makes it impossible to assess what constitutes ‘real’ change and what is simply measurement error. In addition, most of the measures give no information about sensitivity to change.
A similar review of organisational measures by Williams et al. (2012) also included the ‘Recovery Enhancing Environments Measure’ which is well known in its English version DREEM (Dinniss et al., 2007). Like Burgess et al. they concluded that, ‘none of the measures identified can be recommended for use outside their country of origin without further testing. Further psychometric testing, particularly in terms of reliability and sensitivity to change, would provide further evidence of the accuracy and utility of the measures’ (p.1834, op cit).
The ImROC ‘10 key challenges’
Given all these problems, it seems safest at this stage to concentrate on attempts to assess organisational recovery-orientation which are primarily designed to support service development, rather than trying to provide a formal measure of quality. This is what the ImROC ’10 key challenges’ framework was designed to do.
It was developed specifically to help organisations work together to review their current state of development regarding the provision of recovery-oriented services. The framework then assists the groups to set specific targets for service change (Shepherd, Boardman & Burns, 2010). It was not designed as a psychometric instrument and its test-retest or inter-rater reliability have never been explored. However, it does appear to have good content validity if one compares it with the areas identified by Le Boutillier et al. (2011) in their international review of recovery-oriented practice. It has also now been used widely to support the development of more recovery-oriented services by a range of different groups – staff, service users and carers, clinicians, managers – from both statutory and independent sector agencies (NHS Confederation/Centre for Mental Health, 2011; Shepherd, 2013) and has proved a useful heuristic.
As we have gained more experience in using the ’10 key challenges’ four specific elements have emerged as being particularly important in terms of high-quality, recovery-oriented services. These are: (a) the establishment of Recovery Colleges; (b) selecting, training and supporting Peer Support workers; (c) the move from professionally determined risk assessment and management to personcentred ‘safety planning’; and (d) the application of recovery principles to improve the quality of care and safety on inpatient units. All these elements are underpinned by a process of development which depends on ‘co-production’ between people using these services and professionals.
The concept of the ‘Recovery Colleges’ was described in an earlier briefing paper (Perkins et al., 2012). It is based on an ‘educational’ model and uses co-production to develop and deliver courses to students who are a mixture of service users and staff (co-learning). The emphasis is on providing an environment where people can develop their own understanding of mental health issues and how best to manage them. Recovery Colleges are very popular with service users and can often engage people who find traditional services unacceptable. Preliminary (uncontrolled) evidence suggests that two-thirds of those attending at least 70% of the sessions felt more hopeful about the future and were more likely to have developed their own recovery plans. They also showed more engagement in volunteering, education and paid employment (Rinaldi, Wybourn & Clenehan, 2012).
Support from peers in mental health services has been present for a long time, but formally employed Peer Support workers are relatively new. They have been shown to produce a range of improved outcomes including greater optimism about the future, increased selfesteem, a greater sense of empowerment and reduced self-stigmatisation (Repper & Carter, 2010; Repper, 2013a). They also give benefits to those providing the service and help change the organisational culture to one where the contribution of service users is more highly valued and where expectations are raised. A selective review of the effects of adding peer support workers to acute inpatient and crisis teams further suggests that they can also be highly cost effective (Trachtenberg et al., 2013). If Peer Support workers are to have the greatest possible impact then their integrity must be maintained. This means that the whole organisation needs to be prepared to support their introduction and ensure that their key working principles are upheld through careful attention to the processes of recruitment, training, monitoring and supervision (Repper, 2013b).
The move from professionally determined risk assessment and management to person-centered ‘safety planning’ was mentioned earlier in the context of recovery-supporting practices. Minimisation of harm and preservation of safety remain clear aims of mental health services, but risk must be understood as inherent in everyday living and ‘positive risk-taking’ is a valuable route to the development of skills, confidence and resilience which may underpin the recovery process.
The application of recovery principles to improve the quality of inpatient care and reduce the use of physical restraints has been pioneered in the U.S. by Recovery Innovations (Ashcraft, Bloss & Anthony, 2012). ImROC sites in England (e.g. Merseycare) have developed a package, based on the ‘No Force First’ model, consisting of:
- an emphasis on the importance of basic, staff relationship skills (listening, respect, compassion)
- development of co-produced, individual ‘safety plans’ to replace traditional risk assessment and management methods
- avoidance of rigid interpretation of rules, encouraging flexibility
- using peer support workers to provide training and routine ‘de-briefing’ for staff following incidents
- introducing ‘advance directives’ or ‘Joint Crisis Plans’ to ensure that strategies for managing people in crisis accord with their wishes
- clear definitions for incidents, combined with systematic recording and feedback on frequency
- regular ‘Learning the Lessons’ events for staff and service users.
Because they are very new, these combined approaches do not have an extensive evidence base, however the preliminary results are very encouraging (King et al., 2013).
To summarise, a framework of quality indicators for supporting recovery at an organisational level is shown in Box 2.
Box 2: Quality indicators for supporting recovery at an organisational level
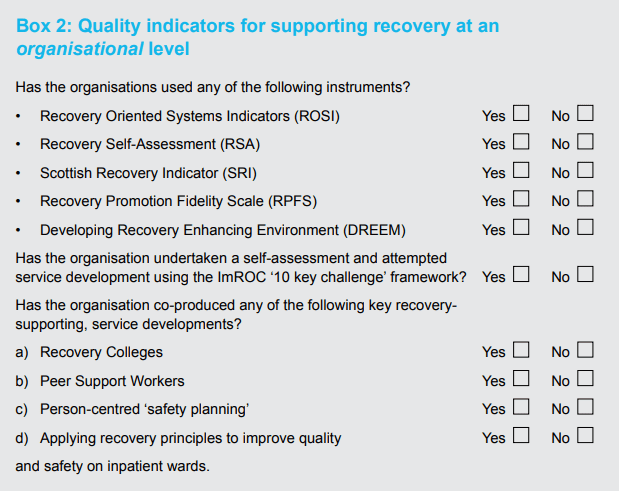
Outcomes
Good quality services should produce good outcomes. How to measure these? When considering outcome measures for recovery, we must first agree what constitute the key areas for measurement (‘domains’). In this we were considerably assisted by a series of meetings with a specially convened expert group who were asked to determine if there was a consensus regarding these key domains1,2. The results of these discussions are summarised in Box 3. For the first four domains there was a strong consensus regarding their importance as outcome measures; for the remaining two, the consensus was less strong.
Box 3: Summary recommendations for recovery outcomes measures
Definite
RECOVERY OUTCOME DOMAIN 1 – Quality of recovery-supporting care
To what extent do service users feel that staff in services are trying to help them in their recovery?
Recommended measure: INSPIRE
RECOVERY OUTCOME DOMAIN 2 – Achievement of individual recovery goals
To what extent have goals, as defined by the individual, been attained over time?
Recommended measures: Goal Attainment Scaling (GAS), narrative accounts
RECOVERY OUTCOME DOMAIN 3 – Subjective measures of personal recovery
To what extent do individuals feel that their hopes, sense of control and opportunities for building a life beyond illness have improved as a result of their contact with services?
Recommended measure: Questionnaire on the Process of Recovery (QPR)
RECOVERY OUTCOME DOMAIN 4 – Achievement of socially valued goals
Has the person’s status on indicators of social roles improved as a result of their contact with services?
Recommended measures: Relevant items from Adult Social Care Outcomes Framework (2013b), Social inclusion web.
Possible
RECOVERY OUTCOME DOMAIN 5 – Quality of life and well-being
Has the person’s quality of life and well-being improved?
Recommended measures: MANSA, WEMWBS
RECOVERY OUTCOME DOMAIN 6 – Service use
As a result of their recovery being supported, has the person made an appropriate reduction in their use of formal mental health services?
Recommended measures: Relevant items from the NHS Outcomes framework, and the Mental Health Minimum Data Set (but beware!).
RECOVERY OUTCOME DOMAIN 1 – Quality of recovery-supporting care
The first domain is not actually a measure of individual outcomes: it is really a measure of process. However, it is clear that if services are to be successful in supporting recovery outcomes, then they should be providing a different experience for the people using them. Improving patients’ experience of care figures prominently in both the NHS and Adult social care outcome frameworks (Department of Health 2013a; 2013b). The expert group agreed that quality of experience constituted an important recovery outcome in its own right.
Many services already use a range of survey methods – often ‘home-grown’ – to assess experience of care as part of local quality initiatives3. These are useful, but sometimes the methods used are not very sophisticated and the way in which samples have been constructed means that the results are not reliable. A more formal survey, using a standardised, self-report, postal questionnaire and a consistent random sampling method is provided by the ‘National Patient Survey’ (NPS) (www.nhssurveys.org/). The questionnaire was designed with considerable input from service users and several of the items are directly relevant to recovery issues. Despite the limitations of a postal questionnaire in terms of the relatively low response rate (approximately 30%) the data from the NPS do provide useful information which could be used as a ‘snapshot’ of outcomes regarding perceived quality of care, especially in terms of charting progress within a single service over time. The NPS could be improved if the sampling was targeted on specific clinical areas (including inpatient care) and the questionnaire data were supplemented by individual interviewing or focus groups4.
In our view, probably the best method for assessing perceived quality of care in relation to support for recovery is a new tool developed by the REFOCUS group at the Institute of Psychiatry in London known as INSPIRE (Williams et al., 2011). This tries to assess whether particular types of recovery support are important to the service user (hope, understanding, building on strengths, etc.) and whether she/he feels these are provided by their current mental health worker. It also asks questions about the general quality of the helping relationship. INSPIRE is relatively quick and easy to use (10 minutes to complete) and appears to have good face validity. There is some evidence that key areas may be missing – notably physical fitness, work and medication (Rinaldi, 2013) but, in general, the content validity is good. It is being used successfully by several sites in the ImROC programme (e.g. Newman-Taylor et al., in press). There is also a short, five item, version of INSPIRE5 now available (Slade, personal communication, 2013). This could form the basis of a quick and easy method for routine evaluation of service quality.
RECOVERY OUTCOME DOMAIN 2 – Achievement of individual recovery goals
Recovery is, of course, a unique and individual process. This poses particular challenges for attempts to measure outcomes since most measurement tools prescribe a particular set of outcomes and are designed to summarise effects between groups (e.g. in controlled trials). Thus, instruments like the STAR suggest a set of outcome domains in advance which may – or may not – be relevant to every individual. The STAR is also psychometrically weak with little evidence regarding its internal validity (Dickens et al., 2012) and even less regarding its test-retest reliability or external validity (Burgess et al., 2011; Hampson et al., 2011).
Probably the best known, truly individually-based, measure is the ‘Goal Attainment Scale’ (GAS), (Kirusek & Sherman, 1968). In this a specific outcome is agreed between the person and their care worker, together with different ‘levels’ of this outcome which might be achieved within a specific time period (e.g. ‘Most likely’, ‘More than expected’, ‘Much more than expected’, ‘Less than expected’ and ‘Much Less than expected’). Each level can be assigned a numerical score and different scores can also be weighted. The GAS has been widely used in mental health services and there is relatively good evidence for its inter-rater reliability and construct validity. It also shows good sensitivity to change (Hurn et al., 2006) and is almost completely flexible: it can reflect more-or-less any aspiration in terms of personal life goals. In many respects, it is therefore an ideal measure for individual recovery goals. However, the data are difficult to aggregate across individuals and it is therefore difficult to compare effects across groups.
If one is not interested in aggregating results across individuals, then it is worth considering narrative accounts (recovery stories) as outcome measures. These are highly personal and individualised and can capture outcomes in a very vivid, easy-to-understand form. These stories can be very powerful indicators of the effects of recovery-supporting services and, despite their simplicity, can provide compelling evidence for the effectiveness of particular kinds of support.
RECOVERY OUTCOME DOMAIN 3 – Subjective measures of personal recovery
The INSPIRE measure tries to measure the extent to which the person feels that the service is trying to support them along key recovery dimensions, but this is not the same as the person actually feeling more hopeful, more in control, more supported to build a life beyond illness, as a result. There are a number of examples in the literature of attempts to measure these kinds of outcomes with simple, Likert scales, e.g. ‘I feel more hopeful for the future as a result of the course’, Strongly agree > Agree > Neither agree nor disagree > Disagree > Strongly disagree’. These kinds of scales are quick and easy to use, with good face validity, but they are psychometrically weak, with unknown test-retest reliability, sensitivity to change, or social desirability bias.
In terms of standardised measures for subjective recovery, these were also covered in the Burgess et al. (2011) review cited earlier. Using the same criteria they employed to evaluate organisational recovery-orientation they examined 22 instruments and ended up (again) with just four possible candidates.
- Recovery Assessment Scale (RAS)
- Illness Management and Recovery Scales (IMR)
- Stages of Recovery Instrument (STORI)
- Recovery Process Inventory (RPI).
(Details of these instruments are given in the Technical Appendix).
As with the organisational tools, all these instruments have their strengths and weaknesses,and the problems of cross-cultural applicability still apply. They would therefore require further development and testing for routine use in an English context (or other countries). A useful measure which was not considered by Burgess et al., but which was developed specifically for use in a Britain with people with a diagnosis of psychosis, is the Questionnaire about Process of Recovery (QPR), (Neil et al, 2009). This has good coverage of the key recovery dimensions – hope, control, opportunity – and excellent psychometric properties (Shanks et al. 2013). It also closely maps onto the CHIME framework – Connectedness, Hope, Identity, Meaning and Empowerment – developed by Leamy et al. (2011) and has been used as the primary outcome measure in the REFOCUS study. We would therefore recommend it as the best standardised measure of personal recovery currently available for use in a British context.
RECOVERY OUTCOME DOMAIN 4 – Achievement of socially valued goals
Most people’s recovery story contains reference to the importance of quite objective, valued, social goals – ‘somewhere to live, something to do and someone to love’ (Perkins, 2012). These ‘objective’ indicators are relatively simple to define and, in principle, should be relatively straightforward to measure. For example, they are reflected in items from the NHS Outcomes Framework (Department of Health, 2013a) and the Adult Social Care Outcome Framework (Department of Health, 2013b). A list of possible indicators is suggested below:
- Engaged in whole or part-time paid employment of their choice
- Accessing volunteering
- Accessing education or training
- Participating in local community activities
- Reporting increased social network
- Living in settled accommodation of their choice where they feel safe and secure.
The problem with these ‘objective’ outcomes lies in ensuring that they are defined unambiguously and then in setting up systems for routine data collection. Given the enormous problems with large scale information systems, this is probably best achieved by small scale, local initiatives.
Regarding these kinds of social goals, the ‘Social Inclusion Web’ (Hacking & Bates, 2008) provides a practical resource to help individuals (or groups) chart and then monitor their progress regarding increasing community inclusion. It covers eight domains of social contact – employment, education, volunteering, arts & culture, faith and meaning, family and neighbourhood, physical activity and services – and assesses the number of people in the person’s social network and the number of places that matter to them. The information is intended to be produced by a joint discussion between the person and their key worker and the results are presented in an easy-to-understand, ‘clock’ diagram. Data from 150 service users in Liverpool demonstrated good sensitivity to change and good content validity.
The final two domains are important, but received less consensus support from our stakeholder group.
RECOVERY OUTCOME DOMAIN 5 – Quality of life and well-being
Intuitively, supporting people to pursue their recovery should result in an increased ‘quality of life’. There are a number of quality of life measures available, but probably the best – and most practical – for routine use is the ‘Manchester Short Assessment of Quality of Life’ (MANSA) (Priebe et al., 1999). This has been specifically developed for use in a British context. It has good psychometric properties and has been used extensively to evaluate changes following the introduction of various service developments. It measures both objective aspects of quality of life (work, finances, social support, accommodation, safety, leisure, family, physical and mental health) and subjective satisfaction with these aspects of social adjustment. It is a very good instrument, but it does take time to administer and is probably best viewed as a research tool, rather than as a routine outcome measure. Notwithstanding, with the right kind of electronic support, it could be introduced as part of routine reviews.
The other measure which is related to ‘quality of life’ and is becoming increasingly popular is the ‘Warwick and Edinburgh Mental WellBeing Scale’ (WEMWBS) (Tennant et al., 2007). This was designed as a measure of positive mental health primarily for use in population surveys. It consists of 14 items, each rated on a 5 point scale, referring to the person’s experience over the last two weeks. It has good test-retest reliability and shows sensitivity to change. It also has high internal consistency and low social desirability bias. The WEMWBS is a good measure, but it was not developed as a measure of ‘recovery’ and the items are therefore not phrased using recovery language. They are also very similar to items contained in general measures of psychological distress and the WEMWBS correlates quite highly with these kinds of instruments (e.g. +0.53 with the GHQ-12).
‘Well-being’ should also not be assumed to be the same as ‘quality of life’. Connell et al. (2012) in an important paper based on a synthesis of qualitative research on quality of life for people with mental health problems concluded that it includes ‘well-being’, but this was only one element in the construct. A number of other dimensions were also important including: subjective sense of control (particularly regarding distressing symptoms), feelings of autonomy and choice, a positive self-image, a sense of belonging, engagement in meaningful and enjoyable activities and feelings of hope. There are obvious similarities between these dimensions and basic recovery principles (hope, control, opportunity).
RECOVERY OUTCOME DOMAIN 6 – Service use
Finally, we come to the controversial question of whether reduced use of mental health services can be used as an indicator of ‘recovery’. The focus of recovery is on building a meaningful and satisfactory life and it can be argued that this is going to be difficult if the person is heavily dependent on mental health services (e.g. in hospital for long periods). However, simply reducing use of services cannot be justified as an indicator of facilitating recovery. Of course, use of ineffective or unnecessary services should be reduced, but it depends on the individual just how important formal services are to their recovery. Reduced use of services may therefore be an indicator of recovery for some people, but it must be a consequence, not a cause. It also cannot be used on its own and should only be interpreted in the context of the other kinds of measures we have been discussing here.
In terms of measuring these service-related indicators, most are covered in the NHS Outcomes Framework (Department of Health, 2010), and the Mental Health Minimum Data Set (Health & Social Care Information Centre, 2013). Relevant items might be:
- number of inpatient admissions
- average length of stay
- time detained under MHA in hospital
- subject to Supervised Community Treatment Order (CTO)
- number of face-to-face community contacts with psychiatrists
- number of face-to-face community contacts with CPN or care coordinator
- number of face-to-face community contacts with other health professionals.
Outcomes for staff
There is another set of outcomes which may result from adopting more recovery-oriented approaches to mental health services. These concern the potential health benefits for staff. It is estimated that mental health problems among staff account for more than a third of sickness absence in the NHS (Health Service Journal, 2013a) and, given the overall cost of sickness and absence in 2012/13 was £1.55 billion (NHS Employers, 2013), this amounts to approximately half a billion pounds (£500,000,000) lost to the NHS as a whole through mental health issues in the workforce. If progress towards more recovery-oriented services could reduce these figures then there are clearly huge potential benefits in terms of improved health for staff and reduced costs. Is this feasible?
At the moment we simply don’t know. There is little formal research specifically relating to the impact of more recovery-oriented services. However, anecdotal evidence suggests that staff frequently report how much they like working in ways to support recovery – it allows them to do the things they came into the job to do: ‘it just feels right.’ Our impression is therefore that working in recovery-focused ways can reduce sickness and absence and improve job satisfaction for staff (e.g. see Health Service Journal, 2013b).
Recovery-oriented organisations should also apply the same principles to support those employed to deliver the services as they do to those using them. We are currently building a repertoire of Human Resources, Occupational Health and workforce approaches based on recovery principles and aimed at increasing job satisfaction and reducing work-stress related sickness. These approaches will be the subject of a forthcoming briefing paper. In the meantime, the potential benefits for staff – and for organisations – from adopting recovery-oriented principles need further systematic investigation.
Conclusions
Recovery is a complex construct and measuring quality and outcomes is therefore bound to be a complex process. This has to be acknowledged. It cannot be reduced to a single measure or practice just because this is convenient. At the heart of recovery outcomes must be the experience of the person themselves and their unique hopes and dreams for the future. In terms of measurement, this is probably still the most difficult area.
Having said this, considerable progress has been made. We are now in a position to describe in reasonable detail what constitutes an effective, ‘recovery-oriented’ service, at both an individual and an organisational level and we can support many of our conclusions with good quality evidence. The notion that, ‘Recovery sounds alright, but it’s too difficult to define and it’s not evidence-based’ is therefore not sustainable. How services may more effectively support recovery is definable. Our problem – as in many other areas of mental health services – therefore lies in implementing what we know to be important, rather than not knowing what this is.
Similarly, despite all the methodological problems, we can agree on a simple framework for recovery outcomes. This includes an improved experience of care, support for individual and socially-valued goals and enhanced feelings of hope and control. What we now need to do is to agree on the details of these broad domains and develop practical systems for routinely collecting the necessary information to monitor these outcomes.
There are also arguments for considering attempts to measure ‘quality of life’ and ‘well-being’, but these are less strong. We must also be clear that they are not the same thing. Comprehensive measures of quality of life are likely to have a strong relationship with subjective measures of recovery, but narrow measures of well-being will not. Measures of recovery outcomes based on service use also have some value, but only taken in the context of other measures. We should surely be aiming for people to be less dependent on services, but we should be aiming to do this by supporting their choices, not by forcing ‘choices’ upon them.
So, much remains to be done. In the current climate we will undoubtedly continue to suffer the familiar round of changes to the structure and functions of different parts of health and social care – ‘stirring the pot’ in a different direction – combined with severe overall restrictions on funding which now look likely to persist into the foreseeable future. We therefore need to think of how we are going to pursue the goals of establishing more ‘recovery-supporting’ services using methods which go beyond simply ‘salami slicing’ existing services. We may need to start to consider reforms, including in relation to the workforce and the balance between ‘peer support’ staff and traditional mental health professionals. Questions about outcomes and cost-effectiveness will be central to these debates.
Recommendations
- For health and social care providers
- Acknowledge that defining ‘quality’ in services to support recovery for people with mental health problems is not simple or one-dimensional.
- Recognise that recovery is based on simple, human needs: to have hope for the future, to feel somewhat in control of your life and to be able to have access to the ordinary things that make life meaningful – somewhere to live, something to do, someone to care about you, and a feeling that you are a part of society, not excluded from it.
- Ensure that all staff are managed not just in terms of their technical competence in delivering ‘evidence-based’ interventions which will support these goals, but also their ability to form honest and respectful relationships with the people using services.
- Give consistent messages to staff that support for recovery is a priority and that this can be achieved without significant additional costs.
- Encourage staff to think beyond the traditional roles of ‘expert professionals’ and ‘passive patients’ and work together with the people who use services to ‘co-produce’ services which support recovery outcomes.
- Encourage boards to ensure that recovery-focused outcomes are given priority throughout their organisations.
- Using the outcome framework described in this paper, agree specific measures with service users and carers to be used locally which adequately reflect recoveryoriented outcomes and establish practical systems for routinely collecting this information.
- For health and social care commissioners
- Recognise that supporting recovery is complex and cannot be reduced to a single quality or outcome measure, no matter how superficially attractive this might appear.
- Look for evidence that providers place emphasis on improving the process of care (quality of experience) in addition to the delivery of evidence-based interventions aimed at securing specific outcomes.
- Notwithstanding 2.2 above, look for evidence that local providers are offering a number of key service developments – peer support workers, recovery colleges, shared decision-making, supported self-management, Individual Placement and Support (IPS), ‘No Force First’ – which are likely to lead to desirable, recovery-focused outcomes.
- Recognise that the application of key recovery principles – ‘expert patient’, personalisation, choice, importance of self-management and shared decisionmaking – are common to the effective management of long-term conditions in both mental and physical health services.
- Recognise that these ‘long-term condition management’ models require an emphasis on supporting people to achieve social (life) goals in addition to symptom management.
- Using the outcome framework described in this paper, agree specific measures to be used locally with providers, service users and carers which adequately reflect recovery-oriented outcomes and establish practical systems for routinely collecting this information.
- For government and NHS England
- Ensure that ‘transactional models’ of health care delivery (e.g. PBR) support the central importance of the provision of effective relationships in healthcare.
- Ensure that central, regulatory bodies such as the Care Quality Commission embed a framework for delivering highquality, recovery-oriented services and recovery-focused outcomes into their mental health inspection methodology.
- Within an agreed framework for quality and outcomes for mental health services which will support recovery, encourage local commissioners and providers – and user and carer groups – to work together to agree on systems for routinely collecting and feeding back relevant information to monitor performance.
PART II. TECHNICAL APPENDIX
In this section we will present detailed technical support for a number of the conclusions and recommendations cited above. The structure replicates Part I.
Quality indicators at an individual level – Recovery-promoting relationships
Box A: NICE Quality Standards for service user experience in adult mental health (QS14 Issued December 2011)
http://publications.nice.org.uk/quality-standard-for-service-userexperience-in-adult-mental-health-qs14
Statement 1. People using mental health services, and their families or carers, feel optimistic that care will be effective.
Statement 2. People using mental health services, and their families or carers, feel they are treated with empathy, dignity and respect.
Statement 3. People using mental health services are actively involved in shared decision-making and supported in self-management.
Statement 4. People using community mental health services are normally supported by staff from a single, multidisciplinary community team, familiar to them and with whom they have a continuous relationship.
Statement 5. People using mental health services feel confident that the views of service users are used to monitor and improve the performance of services.
Statement 6. People can access mental health services when they need them.
Statement 7. People using mental health services understand the assessment process, their diagnosis and treatment options, and receive emotional support for any sensitive issues.
Statement 8. People using mental health services jointly develop a care plan with mental health and social care professionals, and are given a copy with an agreed date to review it.
Statement 9. People using mental health services who may be at risk of crisis are offered a crisis plan.
Statement 10. People accessing crisis support have a comprehensive assessment, undertaken by a professional competent in crisis working.
Statement 11. People in hospital for mental health care, including service users formally detained under the Mental Health Act, are routinely involved in shared decision-making.
Statement 12. People in hospital for mental health care have daily one-to-one contact with mental healthcare professionals known to the service user and regularly see other members of the multidisciplinary mental healthcare team.
Statement 13. People in hospital for mental health care can access meaningful and culturally appropriate activities seven days a week, not restricted to 9am to 5pm.
Statement 14. People in hospital for mental health care are confident that control and restraint, and compulsory treatment including rapid tranquillisation, will be used competently, safely and only as a last resort with minimum force.
Statement 15. People using mental health services feel less stigmatised in the community and NHS, including within mental health services.
Specific approaches
Housing First (Shelter, 2008)
Key features:
- Offers immediate (or relatively immediate) permanent accommodation for people is provided to service users directly from the streets, without the requirement of assessed housing ‘readiness’.
- There are no preconditions of treatment access or prior engagement with health services (‘housing first, not treatment first’).
- A harm-reduction approach is taken to dependency issues, abstinence is not required.
- There is a separation of access to housing from engagement with services to address health, social care and other support needs.
- Comprehensive support services are offered and brought to the service user. Typically, these include multi-disciplinary specialists, including physical and mental health workers; drug and alcohol treatment workers, employment support workers and peer workers. These are either employed within the housing agency, or brokered from communitybased services.
- Promotes consumer choice regarding engagement with services, including the right to refuse. The programme only demands that service users pay rent, abide by the tenancy conditions and agree to a visit by a support worker (usually) once a week.
- Support can ‘float away’ or return as needs arise and the housing is maintained even if the resident leaves the programme (for example through imprisonment or hospital admission).
Individual Placement with Support (IPS)
Key principles (after Becker, Drake & Concord, 1994):
- Competitive employment is the goal (whole or part-time).
- No selection criteria are used beyond expressed motivation to obtain employment, i.e. it is accessible to all those who want to work.
- There is a focus on consumer preference – ‘fitting the job to the person, not the person to the job’.
- It is based on rapid job search and placement. Thus, it minimises preemployment assessment and training (‘place-then-train’, not ‘train-then-place’).
- Relies on close working between employment specialists (ES) and clinical teams. The ES is embedded in the clinical team and takes a full-part in all its activities (attending assessment meetings, contributing to clinical reviews, recording in notes, etc.).
- Provides individualised, long-term support with continuity.
- Includes access to expert benefits (pensions) advice.
Quality indicators at an organisational level
Burgess et al. (2011) recommended measures to assess the quality of recovery-oriented organisations:
- Recovery-Oriented Systems Indicators (ROSI) – This is a 65 item questionnaire consisting of two sections: (a) the Adult Consumer Self-report Survey (n=42 items) and the Administrative Data Profile (n=23 items). It is psychometrically quite sound, but it is also long and laborious and not well suited for routine use.
- Recovery Self Assessment (RSA) – This was developed on the basis of an extensive review undertaken by service users and providers. It comprises five factors: (a) ‘Is the service focused on user-defined life goals’?; (b) ‘Does it involve service users in the development and provision of programmes?’; (c) ‘Does it offer a diversity of treatment options?’; (d) ‘Are service users’ choices respected by staff and is coercive treatment avoided?’; and (e) ‘Are services individually-tailored to different cultures and interests and are active attempts are made to connect with the local community?’ The instrument has good internal consistency and face validity, but there are some doubts regarding its cross-cultural applicability.
- Recovery-Oriented Practices Index (ROPI) – This was developed by Mancini & Finnerty (2005) in New York but has been adapted for use in a British context as the ‘Scottish Recovery Indicator’. It consists of eight dimensions, each containing a number of specific items which are rated on a five-point scale from ‘absence’ to ‘full adherence’. The ratings are made by mixed groups of staff and service users working together to arrive at a consensus. The SRI contains areas which are clearly linked to achieving a more recovery-oriented service, but also contains dimensions which simply reflect basic good practice. There is little evidence regarding its psychometric properties.
- Recovery Promotion Fidelity Scale (RPFS) – This was developed specifically to assess the degree to which mental health agencies incorporate key recovery principles and practices into their services and operations. The development involved a series of focus groups consisting of service users, carers, managers and clinicians. The final analysis produced 12 items, organised into five domains, each corresponding to a different area of recovery practice. The instrument is intended to guide self-assessments of recovery practice in community agencies and the authors acknowledge that further research is now required to investigate the relationship between the items and recovery outcomes.
The ImROC ‘10 key challenges’ – content validity
Le Boutillier et al. (2011) reviewed 30 international documents offering guidance for recovery-oriented practice and found four key domains. These were:
- Working relationships – Practitioners demonstrate a genuine desire to support individuals and their families to fulfil their potential and to shape their own future. A therapeutic relationship is essential in supporting recovery where partnership working and hope is promoted.
- Supporting personally defined recovery – Practitioners focus on personally defined recovery and view recovery at the heart of practice and not as an additional task. Individuals are supported to define their own needs, goals, dreams and plans for the future to shape the content of care. Individuality, informed choice, peer support, strengths focus, and holistic approach are contained in this practice domain.
- Organisational commitment – Organisations that support recovery demonstrate a commitment to ensure that the work environment and service structure is conducive to promoting recovery-oriented practice. The organisational culture gives primacy to recovery, focuses on, and adapts to, the needs of people rather than those of services. Recovery vision, workplace support structures, quality improvement, care pathway and workforce planning sit within this practice domain.
- Promoting citizenship – The core aim of services is to support people who live with mental illness to reintegrate into society and to live as equal citizens. Citizenship is central to supporting recovery, where the right to a meaningful life for people living with sever and enduring mental illness is advocated. Seeing beyond service user rights, social inclusion and meaningful occupation are grouped in this practice domain.
These domains map onto the ‘10 key challenges’ as shown in Box B.
Box B: ImROC ‘10 key challenges’ and Le Boutillier et al’s key domains of recovery-supportive practice
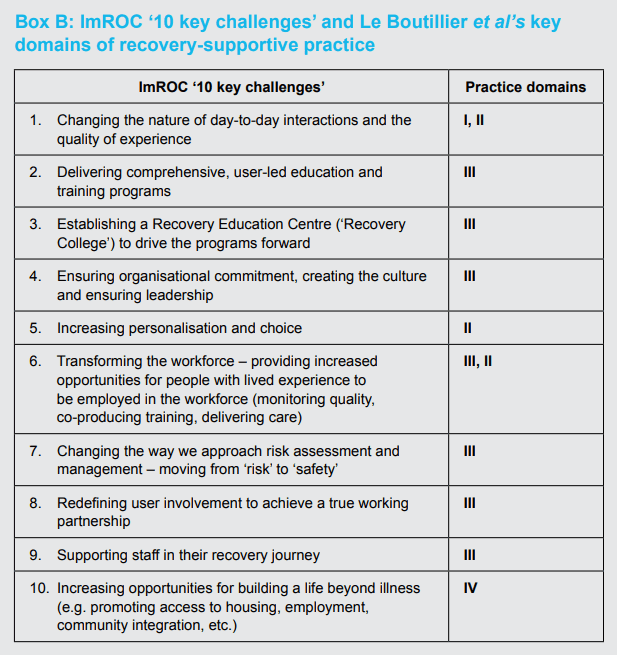
Outcomes
DOMAIN 1 – Quality of recovery-supporting care – INSPIRE (Williams et al., 2011)
21 items with two sub-scales ‘Support’ and ‘Relationships’. The former tries to assess whether particular types of recovery support are important to the service user (hope, understanding, building on strengths, etc.) and whether she/he feels these are provided by their current mental health worker. The latter asks questions about the general quality of the helping relationship (feels listened to, respect, positive belief in recovery.
Although INSPIRE is already quite a short instrument, discussions with Professor Slade suggest that it could be amended to an even shorter form using the ‘CHIME’ conceptual framework for recovery – Connectedness, Hope, Identity, Meaning and Empowerment – derived by Leamy et al. (2011) based on a systematic literature review and narrative synthesis. This is shown in Box C below. Further information is available from: www.researchintorecovery.com/inspire
Box C: Suggestions for a short version of the INSPIRE scale using the CHIME dimensions (Leamy et al., 2011)
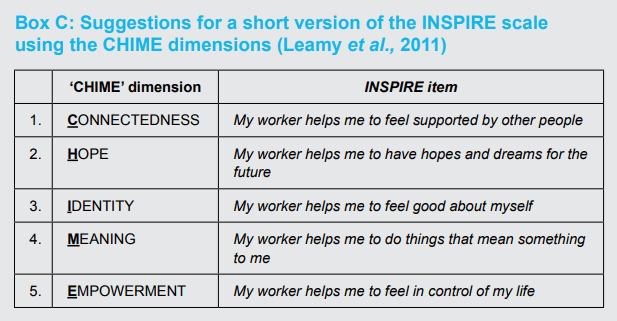
DOMAIN 2 – Achievement of individual recovery goals – ‘Goal Attainment Scaling’ (GAS) developed by Kirusek & Sherman (1968)
A worked example is given in Box D.
Box D: An example of Goal Attainment Scaling
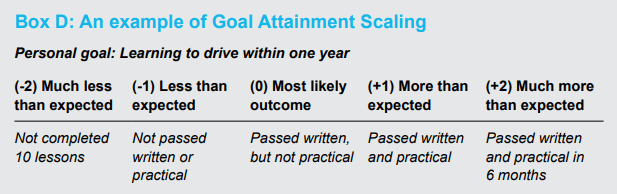
DOMAIN 3 – Subjective measures of personal recovery
Burgess et al. (2011) recommended measures to assess the subjective recovery outcomes.
- Recovery Assessment Scale (RAS) – assesses hope, willingness to ask for help, illness management, goal-orientation and self-determination (24 items).
- Illness Management and Recovery Scales (IMR) – assesses knowledge about illness, medication and side-effects, coping strategies and relapse prevention, symptom management (15 items).
- Stages of Recovery Instrument (STORI) – based on characterising the person’s a ‘stage’ of recovery using a model comprising ‘moratorium’, ‘awareness’, ‘preparation’, ‘rebuilding’ and ‘growth’ (50 items).
- Recovery Process Inventory (RPI) – assesses anguish, connectedness to others, confidence/purpose, living situation, care/help from others, hopefulness/help for self (22 items).
We would add for consideration:
The Questionnaire about Process of Recovery (QPR) (Neil et al, 2009) consists of 22 items, each rated on a five-point scale, which break down into two factors ‘intrapersonal’ (n=17 items) covering such items as “I feel that my life has a purpose” and “I can take charge of my life”; and ‘interpersonal’ (n= 5 items) covering items such as: “Meeting people who have had similar experiences makes me feel better” and “My recovery has helped challenge other peoples’ views about getting better”.
REFERENCES
Alakeson, V. & Perkins, R. (2012) Personalisation and Personal Budgets. ImROC Briefing paper 2. London: Centre for Mental Health.
Ashcraft, L., Bloss, M. & Anthony, W.A. (2012). The Development and Implementation of “No Force First” as a Best Practice. Psychiatric Services, 63, 415 – 417.
Baker, E., Fee, J., Bovingdon, L., Campbell, T., Hewis, E., Lewis, D., Mahoney, L. & Roberts, G. (2013) From taking to using medication: recovery-focussed prescribing and medication management. Advances in Psychiatric Treatment, 19, 2-10.
Becker, D.R., Drake, R.E. & Concord, N.H. (1994) Individual placement and support: a community mental health center approach to vocational rehabilitation. Community Mental Health Journal, 30, 193-206.
Bird, V., Leamy, M., Le Boutillier, C., Williams, J., & Slade, M. (2011) REFOCUS: Promoting recovery in community mental health services. London: RETHINK.
Boardman, J. & Friedli, L. (2012) Recovery, Public Mental Health and Wellbeing. ImROC Briefing paper 3. London: Centre for Mental Health.
Boardman, J., Slade, M. & Shepherd, G. (2013) Assessing recovery – seeking agreement about key domains. Unpublished report for the Department of Health. London: Centre for Mental Health, 134-138 Borough High Street, SE1 1LB.
Boardman, J. & Roberts, G. (in press) Risk, Safety and Recovery. ImROC Briefing paper. London: Centre for Mental Health, NHS Confederation.
Bond, G.R., Drake, R.E. & Becker, D. (2008) An update on randomized controlled trials of evidence-based supported employment. Psychiatric Rehabilitation Journal, 31, 280-290.
Bora, R., Leaning, S., Moores, A. & Roberts, G. (2010) Life coaching for mental health recovery: the emerging practice of recovery coaching. Advances in Psychiatric Treatment, 16, 459-467.
Borg, M. & Kristiansen, K. (2004) Recoveryoriented professionals: Helping relationships in mental health services. Journal of Mental Health, 13, 493-505.
Burns, T., Catty, J., Becker, T., Drake, R., Fioritti, A., Knapp, M., Lauber, C., Tomov, T., Busschbach, J. v., White, S. & Wiersma, D. (2007) The effectiveness of supported employment for people with severe mental illness: a randomised controlled trial. The Lancet, 370, 1146-1152.
Burgess, P., Pirkis, J., Coombs, T. & Rosen, A. (2011) Assessing the value of existing recovery measures for routine use in Australian mental health services. Australian and New Zealand Journal of Psychiatry, 45, 267-280.
Connell, J., Brazier, J.E., O’Cathain, A., Lloyd-Jones, M. and Paisley S. (2012) Quality of life of people with mental health problems: a synthesis of qualitative research. Health and Quality of Life Outcomes, 10:138. DOI: 10.1186/1477-7525-10-138. URL: http://www.hqlo.com/content/10/1/138
Copeland, M.E. (2011) Wellness Recovery Action Plan (WRAP). http://mentalhealthrecovery.com/store/wrap.html
Davies, S., Wakely, E., Morgan, S. & Carson, J. (2012) Mental health recovery heroes past and present. A handbook for mental health care staff, service users and carers. Brighton: Pavilion Press.
Deegan, P.E. & Drake, R.E. (2006) Shared Decision Making and Medication Management in the Recovery Process. Psychiatric Services, 57, 1636-1639.
Department of Health (2007) Independence, choice and risk: a guide to best practice in supported decision-making. http://webarchive.nationalarchives.gov.uk/ 20130107105354/http://www.dh.gov.uk/en/ Publicationsandstatistics/Publications/ PublicationsPolicyAndGuidance/DH_074773
Department of Health/HMG (2011) No health without mental health: a cross-government mental health outcomes strategy for people of all ages. London: Department of Health. http://www.dh.gov.uk/mentalhealthstrategy
Department of Health (2013a) The NHS Outcomes Framework 2014-15. London: Department of Health. https://www.gov.uk/ government/publications/nhs-outcomes-framework-2014-to-2015
Department of Health (2013b) The 2014/2015 Adult Social Care Outcomes Framework. London: Department of Health. https://www. gov.uk/government/publications/adult-socialcare-outcomes-framework-2014-to-2015
De Silva, D. (2011) Helping people help themselves. London: The Health Foundation. http://www.health.org.uk/publications/ evidence-helping-people-help-themselves/
Dickens, G., Weleminsky, J., Onifade, Y. & Sugarman, P. (2012) Recovery Star: validating user recovery. The Psychiatrist, 36, 45-50.
Dinnis, S., Roberts, G., Hubbard, C., Hounsell, J. & Webb, R. (2007) User-led assessment of a recovery service using DREEM. Psychiatric Bulletin, 31, 124-127.
Foster, G., Taylor, S.J.C., Eldridge, S., Ransay, J. & Griffiths, C.J. (2007) Selfmanagement education programmes by lay leaders for people with chronic conditions. Cochrane database of Systematic Reviews Issue 4. Art. No.: CD005108.
Francis, R. (2013) The Mid Staffordshire NHS Foundation Trust Public Inquiry Final report. http://www.midstaffspublicinquiry.com/report
Goldberg, D. & Williams, P. (1988) A users guide to the General Health Questionnaire. Slough: NFER-Nelson.
Greenhalgh, T. & Hurwitz, M. (1999) Narrative based medicine: Why study narratives? British Medical Journal, 318, 48-50.
Hacking, S. & Bates, P. (2008). The Inclusion Web as a tool for person-centred planning and service evaluation. Mental Health Review Journal: Research, Policy and Practice, 13, 4-15.
Hampson, M., Killaspy, H., Mynors-Wallis, L. & Meier, R. (2011) Outcome measures recommended for use in adult psychiatry, Royal College of Psychiatry Op 78, June 2011.
Hasson-Ohayon, I., Roe, D. & Kravetz, S. (2007) A Randomized Controlled Trial of the Effectiveness of the Illness Management and Recovery Program. Psychiatric Services, 58, 1461-1466.
Health & Social Care Information Centre (2013) Mental Health Minimum Dataset (MHMDS) Specifications and Guidance v4.1. http://www.hscic.gov.uk/mhmds/spec
Health Services Journal (2013a) Why It’s Time to Help the Helpers. Mental Health Supplement, 6 December, 2-3.
Health Services Journal (2013b) Spelling It Out Loud And Clear. Mental Health Supplement, 6 December, 4-5.
Henderson, C., Flood, C., Leese, M., Thornicroft, G., Sutherby, K. & Szmukler, G. (2004) Effect of joint crisis plans on use of compulsory treatment in psychiatry: a single blind randomised controlled trial. British Medical Journal, 329, 136-138.
Henderson, C., Flood, C., Leese, M., Thornicroft, G., Sutherby, K. & Szmukler, G. (2008) Views of service users and providers on joint crisis plans. Social Psychiatry Psychiatric Epidemiology. Published online 4 October 2008. DOI 10.1007/s00127-008- 0442-x.
Howard, L.M., Heslin, M., Leese, M., McCrone, P., Rice, C., Jarrett, M. & Spokes, T. (2010) Supported employment: randomised controlled trial. British Journal of Psychiatry, 196, 404-411.
Hill, L., Roberts, G. & Igbrude, W. (2010) Experience of support time and recovery workers in promoting WRAP. The Psychiatrist, 34, 279-284.
Hurn, J., Kneebone, I. & Cropley, M. (2006) Goal setting as an outcome measure: a systematic review. Clinical Rehabilitation, 20, 756-772.
King, L., Robb, J., Riley, D., Benson, I. & Tyrer, K. (2013) NO FORCE FIRST – Changing the culture to create coercion-free environments. Presentation to ImROC Learning Set, 11/12/13, Manchester. London: www.ImROC.org
Kirusek, T.J. & Sherman, R.E. (1968) Goal Attainment Scaling: A General Method for Evaluating Comprehensive Community Mental Health Programs. Community Mental Health Journal, 4, 443-453.
Latimer, E. (2010) An effective intervention delivered at sub-therapeutic does becomes an ineffective intervention. British Journal of Psychiatry, 196, 341-342.
Leamy, M., Bird, V., Le Boutillier, C., Williams, J. & Slade, M. (2011) Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. British Journal of Psychiatry, 199, 445-462.
Le Boutillier, C., Leamy, M., Bird, V., Davidson, L., Williams, J. & Slade, M. (2011). What does recovery mean in practice? A qualitative analysis of international recovery-oriented practice. Psychiatric Services, 62, 1470-1476.
McColl, A., Roderick, P., Gabbay, J. et al. (1998) Performance Indicators for primary care groups: an evidence based approach. British Medical Journal, 317, 1354-1360.
McKeith, J. & Burns, S. (2010) The Recovery Star: User Guide (Second Edition). London: Mental Health Providers Forum. www.mhpf.org.uk
Mueser, K.T., Corrigan, P.W., Hilton, D.W., Tanzman, B., Schaub, A., Gingerich, S., Essock, S.M., Tarrier, N., Morey, B., VogelScibilia, S. & Herz, M.I. (2002) Illness, Management and Recovery: A Review of the Research. Psychiatric Services, 53, 1272-1284.
Mueser K.T., Meyer, P., S., Penn, D., L., Clancy, R., Clancy, D.M., & Salyers, M. (2006) The Illness, Management and Recovery Program: Rationale, Development, and Preliminary Findings. Schizophrenia Bulletin, 32 (suppl 1), S32 – S43.
Neil, S.T., Kilbride, M., Pitt, L., Nothard, S., Welford, W., Sellwood, W., Morrison, A.P. (2009) The questionnaire about the process of recovery (QPR): A measurement tool developed in collaboration with service users. Psychosis, 1, 145-155.
Newman-Taylor, K., Herbert, L. & Woodfine, C. (in press) Are we Delivering RecoveryBased Healthcare? Psychology Academic Unit, University of Southampton, SO17 1BJ. knt@soton.ac.uk
NHS Confederation/Centre for Mental Health (2012) Supporting Recovery in mental health, Briefing paper, Issue 244. London: NHS Confederation.
NHS Employers (2013) 2012-2013 NHS Sickness and absence figures. http://www.nhsemployers.org/ HealthyWorkplaces/LatestNews/Pages/ StaffSicknessFiguresReleased.aspx
NICE (2011) Quality standard for service user experience in adult mental health. Issued December 2011. http://publications.nice.org.uk/ quality-standard-for-service-user-experience-inadult-mental-health-qs14/list-of-statements
NICE (2013) Service user experience in adult mental health services overview. http://pathways.nice.org.uk/pathways/serviceuser-experience-in-adult-mental-healthservices
O’Connor, A.M., Stacey, D. & Legere, F. (2008) Coaching to support patients in making decisions. British Medical Journal, 336, 288.
Padgett, D., Gulcur, L., & Tsemberis, S. (2006) Housing first services for people who are homeless with co-concurring serious mental illness and substance abuse’. Research on Social Work Practice, 16, 74-83.
Parsonage, M. (2013) Welfare advice for people who use mental health services. London: Centre for Mental Health.
Perkins, R. (2012) UK mental health policy development: a counter-argument deriving from users’ experiences, in P. Phillips, T. Sandford & C. Johnston, C. (Eds), Working in Mental Health: Practice and Policy in a Changing Environment. Oxford: Routledge
Perkins, R. & Rinaldi, M. (2007) Taking back control: A guide to planning your recovery. London: Southwest London & St. George’s Mental Health NHS Trust, Trust Headquarters, Springfield University Hospital, 61 Glenburnie Road, London SW17 7DJ.
Perkins, R., Repper, J., Rinaldi, M. & Brown, H. (2012) Recovery Colleges, ImROC, Briefing 1. London: Centre for Mental Health.
Priebe, S., Huxley, P., Knight, S. & Evans, S. (1999) Application and results of the Manchester short assessment of quality of life (MANSA). International Journal of Social Psychiatry, 45, 7-12.
Rapp, C. & Goscha, R.J. (2006) The Strengths Model: Case Management With People With Psychiatric Disabilities, 2nd Edition. New York: Oxford University Press.
Repper, J. (2013a) Peer Support Workers: Theory and Practice, ImROC Briefing Paper 5. London: Centre for Mental Health and Mental Health Network, NHS Confederation.
Repper, J. (2013b) Peer Support Workers: A Practical Guide to Implementation, ImROC Briefing Paper 7. London: Centre for Mental Health and Mental Health Network, NHS Confederation.
Repper, J. & Carter, T. (2011) A review of the literature on peer support in mental health services. Journal of Mental Health, 20, 392- 411.
Repper, J. & Perkins, R. (2003) Social Inclusion and Recovery. London: Baillière Tindall.
Rinaldi, M., Wybourn, S. & Clenehan, M. (2012) The development, piloting and outcomes from a Recovery College in England. London: Southwest London & St. George’s Mental Health NHS Trust, Trust Headquarters, Springfield University Hospital, 61 Glenburnie Road, London SW17 7DJ.
Roberts, G. (2000) Narrative and severe mental illness: what place do stories have in an evidence-based world? Advances in Psychiatric Treatment, 6, 432-441.
Sainsbury Centre for Mental Health (2009a) Doing what Works: Individual placement and support. Briefing paper 37. London: Sainsbury Centre for Mental Health.
Sainsbury Centre for Mental Health (2009b) Commissioning what Works: The economic and financial case for supported employment. Briefing paper 41. London: Sainsbury Centre for Mental Health.
Salyers, M.P., Godfrey, J.L., McGuire, A.B., Gearhart, T., Rollins, A.L. & Boyle, C. (2009) Implementing the Illness Management and Recovery Program for Consumers with Severe Mental Illness. Psychiatric Services, 60, 483-491.
SAMSHA (2010) Shared Decision-Making in Mental Health Care: Practice. Research and Future Directions. HHS Publication No. SMA-09-4371, Rockville, MD: Centre for Mental Health Services , Substance Abuse and Mental Health Services Administration. http://store.samhsa.gov/product/SharedDecision-Making-in-Mental-Health-Care/ SMA09-4371
Shanks, V., Williams, J., Leamy, M., Bird, V.J., Le Boutillier, C., & Slade, M. (2013) Measures of personal recovery: a systematic review. Psychiatric Services, 64, 974-980.
Shepherd, G., Boardman, J. & Slade, M. (2008) Making Recovery a Reality. London: Sainsbury Centre for Mental Health.
Shepherd, G., Boardman, J., & Burns, M. (2010). Implementing recovery: A methodology for organisational change. London: Centre for Mental Health.
Shelter (2008) Housing First. www.shelter.org.uk/goodpracticebriefings
Simon, D., Willis, C.E. & Harter, M. (2009) Shared decision-making in mental health. In A. Edwards & G. Elwyn (Eds.) Shared decision-making in health care: Achieving evidence-based patient choice (2nd edition pp.269-276). Oxford: Oxford University Press.
Slade, M. (2009) Personal Recovery and Mental Illness. Cambridge: Cambridge University Press.
Slade, M. & Hayward, M. (2007) Recovery, psychosis and psychiatry: research is better than rhetoric. Acta Psychiatrica Scandinavica, 116, 81-83.
Tennant, R., Hiller, L., Fishwick, R., Platt, P., Joseph, S., Weich, S., Parkinson, J., Secker, J., Stewart-Brown, S. (2007) The WarwickEdinburgh Mental Well-being Scale (WEMWBS): development and UK validation, Health and Quality of Life Outcomes, 5:63 doi:101186/1477-7252-5-63.
Thornicroft, G., Farrelly, S., Szmukler, G., Birchwood, M., Waheed, W. et al. (2013) Clinical outcomes of Joint Crisis Plans to reduce compulsory treatment for people with psychosis: a randomised controlled trial. British Journal of Psychiatry, 381, published online March 26, 2013. http://dx.doi.org/10.1016/S0140-6736(13)60105-1
Torrey, W., C. & Drake, R. (2009) Practicing Shared Decision Making in the Outpatient Psychiatric Care of Adults with Severe Mental Illnesses: Redesigning Care in the Future. Community Mental Health Journal. Published online: 08 November 2009. DOI 10.1007/ s10597-009-9265-9.
Trachtenberg, M., Parsonage, M., Shepherd, G. & Boardman, J. (2013) Peer support in mental health care: is it good value for money? London: Centre for Mental Health.
Williams, J., Leamy, M., Bird, V., Harding, C., Larsen, J., Le Boutillier, C., Oades, L. & Slade, M. (2012) Measures of the recovery orientation of mental health services: a systematic review. Social Psychiatry Psychiatric Epidemiology, 47, 1827-1835. DOI 10.1007?s00127-012-0484-y.
1 Boardman, J., Slade, M., & Shepherd, G. (2013) Assessing recovery: seeking agreement about the key domains. Report prepared for the Department of Health, Centre for Mental Health: London.
2 For a full list of members see Appendix 1.
3 Patient (and carer) experience measures are already part of the NHS contract and as from April 2014 Trusts will be required to apply the ‘Family and Friends’ test.
4 We understand that the NPS survey is currently being revised.
5 www.researchintorecovery.com/INSPIRE#s3
APPENDIX 1: MEMBERS OF THE EXPERT GROUP CONVENED TO EXPLORE THE CONSENSUS REGARDING DOMAINS OF RECOVERY OUTCOMES (DEPARTMENT OF HEALTH, 2013)
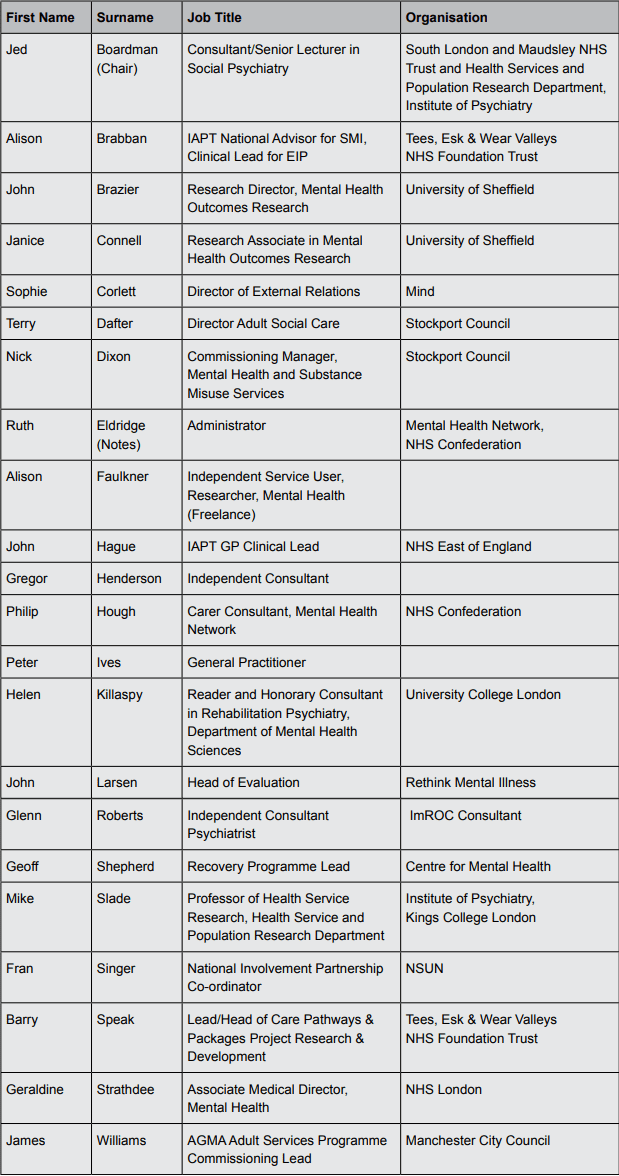
ABOUT THE AUTHORS
Geoff Shepherd
Geoff Shepherd trained originally as a clinical psychologist. He has worked most of his career in the NHS as a practitioner, manager and researcher and is currently leading the ImROC programme (Implementing Recovery through Organisational Change) based at the Centre for Mental Health and the NHS Confederation. Geoff also has a particular interest in employment issues for people with mental health problems. He holds a visiting chair at the Institute of Psychiatry and continues to be active in mental health services research.
Jed Boardman
Jed Boardman is Consultant and Senior Lecturer in Social Psychiatry at the South London and Maudsley NHS Foundation Trust and the Institute of Psychiatry. He is Senior Policy Advisor to the Centre for Mental Health and Lead for Social Inclusion at the Royal College of Psychiatrists. He has worked in community-based mental health services for most of his career. He has published widely in social and community psychiatry and helped to establish the Recovery projects at the Centre for Mental Health. Jed has been a member of the ImROC project team since its inception.
Miles Rinaldi
Miles Rinaldi is the Head of Recovery and Social Inclusion at South West London & St George’s Mental Health NHS Trust. He has been working to implement recovery-focused practice across the organisation, including setting up evidence-based employment services and opening the first Recovery College in England. Miles has worked in the voluntary sector, local authorities, and also within government on mental health policy. He has also conducted service evaluations and research with over 20 peer reviewed journal publications and book chapters. Miles has been a member of the ImROC project team since its inception.
Glenn Roberts
Glenn Roberts has worked for over 30 years as an NHS psychiatrist. He is a past academic secretary of the RCPsych Faculty of Rehabilitation and Social Psychiatry and Lead on Recovery. He has published extensively on aspects of working with people who experience psychosis and the value of narrative and stories. Glenn has a particular interest in working out how to apply recovery principles in psychiatric practice and has been a member of the ImROC project team since its inception. He continues to work for ImROC as a senior consultant.
Supporting recovery in mental health services: Quality and Outcomes
This briefing paper has been produced for the Implementing Recovery through Organisational Change programme, a joint initiative from the Centre for Mental Health and the NHS Confederation’s Mental Health Network.
The pilot phase of ImROC ran from 2011-12 and was supported by the Department of Health, together with contributions from the participating services. The continuing work of ImROC is endorsed by the Department of Health and managed and supported by the Centre for Mental Health and Mental Health Network.
For more information on the current work of ImROC, please visit imroc.org.
ImROC, c/o Mental Health Network, NHS Confederation, 50 Broadway, London, SW1H 0DB
Tel: 020 7799 6666
imroc@nhsconfed.org
imroc.org
ImROC Training Prospectus 2024
Peer workforce strategies, frameworks and resources from Victoria Department of Health
Social Story For Peer Support Visions Of Opportunity For 2030
1. How can we influence policy makers, commissioners and managers so that far more PSWs are commissioned and employed across all sectors in the system?
Steve Shrubb and Julian Eve
Scribe – Kath Florey-Saunders Marlborough Theatre
2. Disrupting hierarchies in formal peer support what can we learn from the voices and experiences of diverse and historically marginalised wisdom?
Aman Ahluwalia Hinrichs
Scribe – Lisa Archibald Maynard Theatre A
3. Peer led visions for transformation: exploring the importance of spirituality frameworks for understanding and supporting people through challenging times
Katie Mottram and Ronan Benson
Scribe – Debbie Connellan Maynard Theatre B
4. Beyond Mental Health: exploring where other opportunities lie in order to increase the reach of peer support
Liz Walker and Jane Rennison
Scribe – Michael Ryan Maxwell Room
5. Do we need a peer support body that can represent Peer Support Workers; develop occupational standards, rights and protection in the same way as other ‘professions’?
Mel Ball and Emma Watson
Scribe – Emma Watson Marlborough Room 3
6. How can organisations better support Peer Support Worker employees?
Danny Bowyer and Deb Owen
Scribe – Sandra Hutton President’s Room
| 9:00 | Registration |
| 9:30 | Performance Danny Bowyer, Training Lead of ImROC |
| 9:40 | Welcome Julian Eve, Executive Director of ImROC, Business, People and Communications |
| 9:45 | How can we influence Mental Health Executive leaders to recognise and support peer support? Sean Duggan, CEO, Mental Health Network, NHS Confederation |
| 10:00 | What is peer support? Lisa Archibald, Co-Director of Intentional Peer Support |
| 10.15 | The current landscape of peer support and visions of possibility for the future Julie Repper, Executive Director of ImROC, Strategy, Innovation and Development |
| 10.30 | Developing the role, influence and status of peer support in Victoria, Australia Emma Cadogan, Manager, Lived Experience Policy, Mental Health and Wellbeing Division Department of Health, Victoria |
| 10.40 | A call for a national strategy Emma Watson, Peer Development Lead, Nottinghamshire Healthcare and Senior Peer Consultant of ImROC |
| 10.50 | How can we engage VCSE organisations providing peer support to influence the agenda and maintain grassroots expertise Kathy Roberts, Chief Executive of the Association of Mental Health Providers |
| 11:00 | Break |
| 11:40 | Employment models and roles of Peer Support Workers Peer Support Workers have many different roles depending on who they support and where they are located. This session offers three different perspectives on this subject
|
| 12:05 | Training, supervision and support We are all aware of HEE competency framework and funding for peer training. What training is on offer? Is this appropriate, adequate, and effective?
|
| 12.25 | The Art of the Possible: What can we do to drive forwards the development of an expanded and fully supported peer workforce? Claire Murdoch, CEO CNWL, National Director of Mental Health |
| 12:40 | Lunch |
| 13:30 | Workshops
|
| 15:30 | Break |
| 15:50 | Feedback from Workshops All six workshop facilitators to join a panel to feedback on the headlines and solutions discussed. |
| 16:00 | The vital importance of peer support working A personal view – from Danny Bowyer, Training Lead of ImROC |
| 16:10 | Next Steps and Future Plans Julie Repper, Executive Director of ImROC, Strategy, Innovation and Development |
| 16:30 | Close |
During the day there will be an opportunity to view posters prepared by delegates on diverse topics associated with Peer Support Working. These will be available in the The Garden Room.
Research posters
Dr Sam Robertson, Involvement Lead, Lead AIR (Approaches to Involvement and Recovery) Research Theme. Peer Research Fellow, Sussex Partnership NHS Foundation Trust and Don Robertson, Senior Peer Support Trainer with Sussex Partnership NHS Foundation Trust – Emotional Labour and Peer Support
Dr Laura Asher, Clinical Associate Professor in Public Health and Honorary Consultant in Public Health Medicine, Academic Unit of Lifespan and Population Health| School of Medicine
University of Nottingham – PRIZE peer support in South Africa
Emma Watson, Peer Development Lead, Nottinghamshire Healthcare NHS Foundation Trust (PhD) – Peer Support in an NHS Trust
Ashleigh Charles, ESRC PhD Candidate, School of Health Science, University of Nottingham – (PhD) – case study of peer support
Ruth Cooper, Research Associate, King’s College London and Una Foye, Research Associate, King’s College, London -Umbrella Review of peer support and PRU peer support research findings
Dr Simon Bradstreet, Principal Evaluation Consultant with Matter of Focus – information available about – Evaluation of ImROC peer support training
Posters describing the training offer from:
Heather Tattersall, Deputy CEO – The Cellar Trust courses and support
Daniel Chin, Paragon Client Relationship Manager – Apprenticeships
Poppy Repper and Danny Bowyer, ImROC Consultants – ImROC mental health PSW training pathway
Liz Walker and Jo Luck, ImROC Consultants – ImROC Autism PSW training
Emma Cadogan, Manager, Lived Experience Policy, Mental Health and Wellbeing Division, Department of Health – training PSWs in Victoria, Australia
Holly Harris and Sophie Soklaridis, Research Coordinators for the Collaborative Learning College (formerly CAMH Recovery College – Training PSWs in Toronto
Posters describing organisations offering peer advice/guidance
Becky Aldridge, Chief Executive and Sarah Rose, Director of Operations at the Dorset Mental Health Forum – Dorset Recovery Forum
Rachel Edgecombe Founder & Consultant, Lived Experience Leaders – LEAD (Lived Experience Advisory Directory
Katie Mottram, Trainer with ImROC and Founder of Emerging Proud
Aman Ahluwalia Hinrichs, Founder of Birthing Ourselves – Birthing Ourselves
Water (still and sparkling) will be available all day.
Tea and coffee will be served at break times.
Lunch will be served at 12.40 and will feature the following menu:
Braised beef and smoked mozzarella lasagne
Salmon venezia with capers, sultanas, pine nuts, tomato and oregano sauce (gf)
Cauliflower, kale, sweet potato pasticcio with sun-dried tomatoes (v)
Rosemary potatoes and garden vegetables (ve)
Salad Meditteraneo (ve)
Tomato, olive and rocket salad (v)
Fresh bread (v)
We’re keen for people attending our event to have a space where they can relax and take some time out. That’s why we are working with EventWell, a company which provides award winning flexible and pop-up quiet rooms and resilience hubs, focused on event welfare, neuroinclusion, and mental wellbeing. These have been meticulously designed to offer a serene mental escape within a safe, supervised, and accessible space. These spaces are specifically tailored to support and enhance the overall event experience for individuals.
Conferences and events are vibrant and dynamic environments, brimming with opportunities for learning and exploration. However, they can also be overwhelming, exhausting, and triggering for many individuals due to the constant stimulation and outward-facing nature. Our quiet rooms provide a sanctuary where attendees can retreat when they feel overwhelmed or overloaded by the sensory input of their surroundings. These spaces offer individuals the time and space they need to calm their sensory and nervous systems, allowing them to decompress and find respite.
The role of event welfare is to provide emotional and practical support to all event attendees, including the event team. Even the most experienced event organiser cannot predict when emotional or practical support will be required during an event. Our EventWell Hosts are highly skilled in creating a supportive environment and offering essential assistance whenever needed.
An EventWell space, with a trained and experienced host as its cornerstone, offers a comprehensive solution. It provides all attendees with a supervised and safe space where they can:
Catch up on emails, read, take a nap, meditate, listen to music, practice deep breathing, or simply rest and take a much-needed 10-minute ‘brain break’
Reduce stimulation and triggers, effectively manage and regulate any sensory overload, and find a sense of calm
Engage in a confidential and discreet conversation with a safe person about any emotions, experiences, or observations they may have encountered
These dedicated spaces and trained team ensure that everyone feels supported, valued, and able to fully engage in the event experience.
ImROC trained Peer Support Workers will also be on hand to assist in the Quiet Space.
For this event the space will be available in the Chris Ham room.
We have set aside a designated family room, should any of our delegates require a quiet space to look after infants or small children. The Family Room can be found in Maynard Room 3.
Also available on the day will be a prayer room for guests needing this facility.
For this event the space will be available in the Maynard Room 2.
Event Support Team
The event support team is here to help you with any questions or worried you may have. They can be identified by the mango T-shirts they are wearing. Any one of them can help you manage the day.
Welcome to the ImROC web site. This week we are finalising the planning for our event on 25 April. Peer Support: Visions of Opportunity for 2030. On Thursday we will have national and international experts coming together to look at the future of Peer Support Working and how we can embed what has already been achieved for future cohorts of Peer Support Workers and the people they engage with.
Get In Touch
We would love to hear more about your project. Please fill out this form and we will get back to you.
imroc@imroc.orgImROC Head Office PO Box 11115 Nottingham NG14 6UZ
