People in forensic (or secure) mental health services should be offered support that helps them in their personal recovery journeys.
This paper finds that recovery for people in forensic services is in most ways the same as for those using other mental health services. Hope for the future, control over your life and illness, andopportunity for a life beyond illness are key for both. But people with offending histories also have to come to terms with what they have done. Forensic services can help them to recover by supporting them to ‘come to terms with themselves’.
Gerard Drennan and James Wooldridge together with Anne Aiyegbusi, Debbie Alred, Joe Ayres, Richard Barker, Sally Carr, Helen Eunson, Hilary Lomas, Estelle Moore, Debbie Stanton & Geoff Shepherd
To View the ImROC 4th Annual Conference Presentation (Realities and Possibilities for Recovery – focused Practice in Secure Settings) click here
10. Making Recovery a Reality in Forensic Settings
Gerard Drennan and James Wooldridge together with Anne Aiyegbusi, Debbie Alred, Joe Ayres, Richard Barker, Sally Carr, Helen Eunson, Hilary Lomas, Estelle Moore, Debbie Stanton & Geoff Shepherd
Introduction
Forensic settings are probably among the most difficult places to think of applying recovery principles. People in forensic services are doubly stigmatised with repeated or prolonged contact with the criminal justice system in addition to mental health problems. Many also often have a range of pre-existing social disadvantages – family problems, educational failure, poor work record, etc. – but the process of recovery is as important for them as it is for anyone else. Indeed, precisely because of their other disadvantages, recovery is, perhaps, even more important. Given all their difficulties, how can people with mental health problems and frequent contact with forensic services be expected to have positive hopes for the future? How can they achieve a sense of control over their lives and their symptoms when so many of their choices are so restricted? How they can build a life ‘beyond illness’ when faced with the toxic combination of stigma and low expectations of those around them? To some people these ambitions may seem desirable in theory, but unrealistic in practice. These are the issues which we hope to address in this paper.
Our aims are threefold. Firstly, we want to present a credible discussion of the challenges of applying the principles of recovery in forensic settings and describe how recovery values can be expressed in a meaningful, non-tokenistic, fashion. Secondly, we want to address the implications of these challenges for staff from all disciplines and at all levels in forensic services – front-line staff, support workers, middle managers, consultant psychiatrists and senior managers. We also want to engage and involve service users and carers. Finally, we will describe current best practice within forensic services, acknowledging that not all services have achieved this, but also point towards the horizons of progressive practice within the criminal justice system and non-forensic mental health services.
A note on authorship
Advances in recovery-focused practice arise from collaborative partnerships between the people who work in mental health services and the people who use them. The ImROC briefing papers have drawn upon this work. Where ideas are taken from published materials we cite them in the conventional form, but we also want to acknowledge the many unpublished discussions and conversations that have informed the creative development of the project as a whole over the last five years.
Each paper in this series has been written by those people best placed lead on the topic. In this case it comprised a ‘collective’, who have worked together over a period of more than two years to produce this document. They believed – and continue to believe – that recovery in forensic services is not unrealistic, nor too great a challenge to meet in a meaningful way. They were helped through a series of local workshops by colleagues and partners, and service users, from forensic services up and down the country.
At each workshop the question, “What helps and what hinders recovery?” was considered across the domains of risk and safety, meaningful occupation, meaningful working relationships, and recovery outcomes. The responses of all those attending to these questions form the basis of what we are reporting here. We would particularly like to thank James Wooldridge, whose personal experience of using forensic services, intelligent reflection and general good humour, have proved invaluable to the project.
Background
In 2008, the ImROC programme produced the first of a series of papers on recovery in adult mental health services (‘Making Recovery a Reality’, Shepherd, Boardman & Slade, 2008). This spelled out the principles of recovery for a UK audience, with particular emphasis on the ways in which organisations could change to support recovery in addition to changes in staff attitudes and behaviour.
In a subsequent publication we described the development of a methodology for achieving organisational change and ways in which this could be measured (Shepherd, Boardman and Burns, 2010). This methodology has now been tested in a major national project, ‘Implementing Recovery through Organisational Change’ (ImROC) funded by the Department of Health, and delivered by a partnership between Centre for Mental Health and the Mental Health Network of the NHS Confederation (NHS Confederation/Centre for Mental Health, 2012).
‘Recovery’ refers to the personal journey of people with mental health problems as they pursue their own, unique, life goals in the presence or absence of continuing symptoms. The role of mental health professionals – and mental health services – is to try and create the right kinds of support to help people achieve these goals. This means supporting certain key principles (see Box 1). Sometimes services are successful in doing this and sometimes they are not.
Often people find the most helpful supports in their recovery are not professionals, but friends, peers and families (Davies et al., 2012). Nevertheless, the primary focus of ImROC has been upon the application of recovery principles in mainstream adult mental health services. However, these principles apply just as strongly to other client groups and to other areas of service development. In this paper our focus is on forensic mental health services.
Are ‘forensic patients’ different from other people when it comes to recovery?
Our first challenge is to examine the notion that ‘forensic patients’ have such special characteristics that recovery ideas simply cannot apply to them, e.g. “It all sounds very well, but it won’t work with these patients”. In order to examine this proposition we have created a fictional character (Jason) whose story is based on typical experiences of young men using forensic mental health services. Through the medium of Jason’s story, we aim to highlight the challenges and the opportunities for recovery. We also asked someone who has direct experience of using forensic mental health services themselves – a ‘service avoider’ (James Wooldridge) – to offer a commentary on Jason’s story.
Box 1: The key principles of Recovery (after Perkins & Repper, 2003)
- Hope – Maintaining a belief that it is still possible to pursue one’s chosen life goals. Hope is personal and relationships are central. The importance of personal meaning and understanding.
- Control – (Re)gaining a sense of control over one’s life and one’s symptoms. Having choice over the content of interventions and sources of help. Balancing evidence-based practice with personal preference.
- Opportunity – The need to build a life ‘beyond illness’. Being a part of the community (‘social inclusion’) not simply living in it. Having access to the same opportunities that exist for everyone else, e.g. with regard to housing, employment, etc.
Box 2: Jason’s story
Jason was 21 years old when he was convicted of the attempted murder of a stranger woman in an unprovoked knife attack. The attack occurred in a public place. Jason was street homeless at the time. He was arrested and, when interviewed by a psychiatrist, reported hearing voices. Jason also spoke to the doctor about being troubled by violent fantasies. He also reported abusing alcohol and self-harming and feeling, ‘completely mental’. Jason was assessed as suffering from schizo-affective disorder and an emotionally unstable personality disorder. He was not sentenced, but a transfer direction to a high secure hospital was made under a Section 37 Hospital Order (Mental Health Act, 1983) with an additional Section 41 Restriction Order. This criminal section of the Mental Health Act is imposed with no time limit, requires the approval of the Secretary of State for Justice for discharge and is imposed to protect the public from serious harm.
Jason’s story will be a familiar one to anyone who has followed media reports of high profile offences by people with a mental illness. Stranger attacks by people with mental illness are rare, but when they occur they often attract a great deal of public and media attention. For example, the case of Christopher Clunis’s fatal attack on Jonathan Zito on a Finsbury Park station platform in 1992 is considered by many to have been a watershed moment in the culture and development of forensic mental health services in England and Wales (Maden, 2007). The so-called ‘offender patient’ is usually well aware of their notoriety in local communities, even when the offences committed do not result in a death or similar such serious harm, and they are therefore faced not only with their personal struggle to come to terms with serious mental health problems and the impact of the offence, but also its social impact. In addition, they may live in fear of retribution in some form. Forensic mental health service users are therefore situated at a complex intersection of health, social and criminal justice systems.
In terms of their personal struggle, the ‘offender patient’ has a huge task to work through their personal guilt and to reconcile their ‘mental illness’ with their sense of personal responsibility (Dorkins & Adshead, 2011; Drennan & Alred, 2012; Moore & Drennan, 2013). Thus, the offending behaviour itself is often seen by the person as the greatest obstacle to their recovery. As one patient in a High Security hospital put it, “How do you recover from having killed someone?” Ideas of ‘empowerment’, ‘choice’, ‘self-determination’ and ‘participation’ can then be seen as impossible (Pouncey & Lukens, 2010). Even the promotion of hope can be seen as creating false expectation, a form of ‘double talk’ for which there is little or no evidence (Mezey & Eastman, 2009; Mezey et al., 2010).
Others have argued that, although recovery for the forensic service user has the added complications of personal guilt and social impact, nevertheless, it is still possible (Drennan & Alred, 2012). But there needs to be a focus on these complicating factors and an additional emphasis on the active tasks of finding a new identity, meaning and purpose (Ferrito et al., 2012; Simpson & Penney, 2011). In order to achieve this, the individual – and those attempting to support their recovery – need to understand as clearly as they can how the person’s life experiences brought them to the point of their offending behaviour. Returning to Jason’s story, ‘How did he get to where he was when he assaulted the unknown woman?’
Understanding the offender patient
Motivations for offending can be many and varied. Offences can be committed for psychotic, neurotic, and frankly criminal, reasons. Offences can have conscious and unconscious motivations, and usually some combination of both. People with mental illnesses and severe emotional disturbances who commit offences are also not always motivated to stop offending. Feelings of entitlement or sexual preferences can be very strong – “that’s just the way I am and no one is going to change me”. When supporting the recovery of non-forensic service users it would be strange to ask the question, “What motivated you to become ill?”, but for offenders the question of motivation is central. Taking responsibility for one’s illness thus includes an implicit acknowledgement of personal responsibility for the offence. This introduces complex scientific – as well as moral and ethical – questions for the person and the teams who work with them (Adshead, 2010; Dorkins & Adshead, 2011; Roberts, 2011; Ward, 2013). These are central to the challenges of applying recovery ideas in forensic settings.
Box 3: Jason’s early life and care in secure services
Jason had behavioural problems from a young age and was seen by mental health professionals as a child. His difficulties were assessed as being connected to his mother’s depression, a poor bond with her child, and domestic violence in the home before his father left the family. An autistic spectrum disorder was considered by professionals, but never confirmed. Jason went on to truant and run away from home. He was taken into care and placed in institutional settings and foster homes, which frequently broke down. Jason was emotionally and physically abused in care, but no sexual abuse was ever confirmed. He began to use alcohol and drugs to cope and became involved in petty crimes of survival, spending some time in Young Offender Institutions as a result. He was homeless when in the community and afraid that he would be attacked. He said he took to carrying a knife for his own protection, although it was suspected that he had developed an obsession with knives. Professionals also worried that there was a sexual element to the attack, but Jason denied this. In fact, he denied having committed the offence for a long time in hospital. Jason’s symptoms of mental illness did not respond well to medication during the first few years in hospital. After a change in medication Jason improved but he remained vulnerable to symptoms re-appearing at times of stress. He continued to be preoccupied with violent fantasies, but was reluctant to engage in any of the group and individual treatments offered to him.
Treatment and control
Treatment in forensic settings, even with psychological therapies, is often seen by patients as more coercive than in other settings. This is because the quality of the recovery achieved by the service user is not simply a question of personal choice, it is part of the imperative to reduce risk and to fulfil the duty of the service to protect the public. In other settings it may be possible to support a service user to achieve a positive sense of self, a sense of purpose, and hopefulness about the future, without being too concerned about whether the symptoms of mental illness or trauma have entirely resolved. In forensic settings, because of the link between illness and offending behaviour, this is more difficult. Sometimes it means testing the resilience of the recovery process and challenging apparent compliance where this may not be rooted in sustainable change.
Of course, there is always a difficult balance to be struck between a healthy scepticism about apparent change and a demoralising lack of belief in the possibility of personal growth. A clear-eyed view of risk and the potential for harm, while holding hope for progress towards a safe and meaningful life, is not easily achieved or maintained. However, if the presence of symptoms or emotional disturbance increase the risk of future harm to self or others, then addressing any possible link between mental health difficulties and emotional issues is not an ‘optional extra’: it must be addressed. At the same time the person must retain some sense of hope for a better life in the future.
Similarly, even when it seems that these imperatives reduce service user choice, choice remains critically important. For offenders to turn away from a life of crime they must make a choice (Maruna, 2005). Paradoxically, compulsory treatment, whether medical or arising from restrictions of movement and access can create an environment of safety in which the first steps towards recovery become possible (Mezey, et al., 2010; Roberts et al., 2008). As one patient put it: “a secure hospital made me stop and let my life catch up with me”. These choices can be supported through cognitive change programmes, talking and expressive therapies. Narrative therapies can help people develop new meaning and a deeper understanding of themselves and, over time, “cover stories” can develop into an authentic account of the harm caused (Adshead, 2012a; 2012b). Hope for oneself and the future can thus be discovered (Hillbrand & Young, 2008).
‘Attachment’ and recovery
Issues of attachment are complex for forensic service users (Pfafflin & Adshead, 2004). Mainstream services may reject the importance of attachment to services and staff members for fear that it leads to unhealthy dependency and may even inhibit recovery. But many service users in secure care have personal histories of severely disrupted childhoods, through parental neglect, physical, emotional and sexual abuse, institutional care, unemployment, poverty and homelessness. These early traumatic experiences can damage people’s ability to form meaningful relationships later in life. For these reasons attachments can continue to be seen as dangerous to the self and to others and issues of ‘trust’ become central (see later on ‘relational security’). The achievement of secure and reliable attachments is therefore an on-going challenge for many people in forensic or secure care and their co-workers. It is also a central element in their recovery.
Box 4: Reflections on Jason – James Wooldridge
Reading what has been written about Jason is difficult. He has done many bad things. However, with the right support, I hope he would begin to realise that taking responsibility for his actions is a major part of his recovery. As far as I am concerned when a staff member first mentioned the word ‘recovery’ I wasn’t sure it applied to me. They said it wasn’t the same as being ‘cured’ but living the best life I can alongside my condition.
Jason had a difficult start to life and his early years were full of abuse. This has understandably left him with ‘trust issues’, making it harder to share his thoughts and feelings with professionals. If he can work with a new care team and feel that people really want to listen and to get to know the real Jason, then he will be encouraged. He needs to feel that he can influence how the assessment will read, using a language that he can understand. He also needs to review how he has often used violence to deal with stressful situations and to develop better coping strategies for dealing with stress.
For Jason – and for many people in forensic services – one of the biggest parts of ‘recovery’ is hope. People struggle with this, they know that they can’t undo the past and wonder whether society will ever forgive their crime, not to mention the victim or the victim’s family. Forgiving yourself can be a starting point but is easier said than done. It is difficult if you are struggling with violent and frightening thoughts. There is no ‘magic pill’ or ‘magic person’ that will take these away. All you can do is hope that one day you’ll be able to leave this place and carry on with your life.
For many people, the only example that will really work is someone who has ‘been there’ and can say, from their experience, that it is possible to rebuild a life outside hospital. This is vital to hear. When you’ve been locked up for a long time you begin to lose faith that you will ever get out.
From what I understand about recovery, it’s not easy. It is often one step forward and three steps back. However, going backwards for a short while isn’t always such a bad thing if you are able to learn from your mistakes and make plans not to repeat them in the future. The principles of recovery make sense, but putting them into action requires effort and motivation. I have realised that my recovery is down to me and I also know that there will be setbacks. The staff I relate to best are those that treat me as a fellow human being. One way of repaying their faith in me is for us to work together and for me to regain some control over my life.
What are the implications of a recovery-oriented approach in secure care?
We will now consider five key areas of work that can contribute to the creation of an environment in which recovery processes can take root in the men and women who become ‘forensic patients’.
Key area I: Supporting recovery along the care pathway
The process of providing recovery-focused care in secure settings is complex. There are a host of national frameworks and guidance that must influence service provision, not least of which is the Mental Health Act (1983, amended 2007) and the Criminal Justice Act. In addition, policy documents such as the NHS England Service Specifications, NICE Guidelines, the Mental Health Strategy and Implementation Framework, and many more, all aim to shape the delivery of care. Within much of this guidance, the principles of supporting recovery have become the cornerstone of good practice. These principles include:
- The importance of maintaining safety and security
- Participation of patients in all aspects of their care
- Shared decision-making, with as much transparency as possible
- Informed choices, no matter how limited by circumstances
- Fostering enabling and supportive relationships with staff, peers, family and friends (relational security).
We will now illustrate the application of these principles at key points along the care pathway in terms of their potential for helping ideas of recovery to take root and develop.
Engagement and admission
The first stage prior to actual admission into secure care is a vital first step. We can imagine Jason prior to admission to a secure hospital, perhaps in prison, acutely distressed and frightened. His first contacts with mental health service providers are crucially important points at which the possibility of recovery and hope for the future can become real – or be dashed. As indicated earlier, this depends upon people like Jason feeling that staff understand his life-story and the circumstances that led to his offending. In this way, they can foster recovery-promoting partnerships from the beginning.
Once admitted into forensic settings care is typically organised around the processes of the Care Programme Approach (CPA). This means that large multi-professional teams are responsible for assessment, planning, review and co-ordination of a range of interventions. The processes of CPA can often seem impersonal and bureaucratic to staff and to service users (Rinaldi & Watkeys, 2014). More personalised approaches such as the WRAP (Copeland, 2011), ‘My Shared Pathway’ (Ayub, Callaghan, Haque, & McCann, 2013) and the suite of toolkits in the Recovery Star (MacKeith, 2011) may be useful complements in helping the person to identify personal goals with a clear, structured approach.
Organisation of care
In terms of the organisation of care in inpatient settings, our workshops identified the following features as most important in building mutually trusting relationships and supporting recovery:
- Consistency in the delivery of supportive care – Instability and under-resourcing of clinical teams can lead to a loss of relational security, a sense of abandonment, and a reticence to engage with services. Service users are understandably upset when there are frequent changes in the care team, unsettling their progress. As one service user told us: “I’ve had five primary nurses in as many months, how does that help me?”.
- Service user participation in the design and delivery of intervention programmes – This can include participation in planning committees, co-facilitation of treatment groups, and organising unit-based activities. It can also include ward-based forums for service users and staff to discuss the daily life of a unit and the experiences of those that participate in it (such as Community Meetings, Reflective Groups, Daily Debrief Meetings).
- Service user participation in the development of policies and protocols – The design and decoration of treatment centres, catering arrangements, and a myriad other aspects of the life of the organisation are all areas where service user participation can have enormous benefits for the people whose recovery needs they seek to meet and for the safe and efficient running of the service itself (see Bowser, 2012, for a detailed description of service user participation at all levels of the organisation). Service users are now established in the Peer Review Teams for the Forensic Quality Network of the Royal College of Psychiatrists.
- Staff selection and appraisal – Increasingly service users are being included in staff selection, appraisal and performance reviews, including those of the most senior staff, such as consultant psychiatrists. This is a key way in which recovery principles can be used to identify service improvements at an individual and grassroots level.
- Service user participation in staff training – Traditional approaches to staff training undoubtedly have a role in introducing staff to recovery principles (Eunson, Sambrook & Carpenter, 2012). But the advent of Recovery Colleges (Perkins, et al., 2012) has now started to pioneer a new approach to training in which service users and staff are involved as equal partners in the learning process – designing and delivering courses and learning alongside staff. These approaches are now beginning to appear in secure settings.
These principles are illustrated in the case study given below (Box 5).
Box 5: Applying recovery principles in the organisation of care – Aurora Ward, West London Mental Health Trust
A women’s 10 bed admission ward, located in a large urban forensic service, had a reputation as a ‘disturbed ward’ where the women were frequently regarded as ‘violent, chronically unwell and difficult to engage.’ The professionals of all disciplines and grades were often observed to be stressed and morale appeared low. Unsurprisingly, the ward was not a popular place to work and service user outcomes were disheartening. Following a particularly unsettled period, the decision was taken to try a new approach.
A modest financial investment was made in order to provide intensive support to implementing a recovery-oriented model of care and the services of an externally appointed Recovery Consultant were engaged to support the service in its transition. The ward leadership team was refreshed and monthly Action Learning Meetings with the Recovery Consultant were introduced. Additionally, some recovery-oriented training for the ward community was delivered, one morning per month, by a trainer from Rethink Mental Illness.
The next step consisted of a half-day team building event, combined with a halfday developing a ‘Team Recovery Implementation Plan’ (TRIP) (Repper & Perkins, 2013). This was facilitated by the external Recovery Consultant and was attended by all staff. Five areas were prioritised and a team member lead identified for each who was tasked with developing an action plan, in collaboration with service users. The priority areas were:
- Provision of examples of real-life recovery stories to inspire hope in the women and in the staff team.
- Development of recovery-oriented care plans and crisis plans, using a range of selfmanagement tools, e.g. the Recovery Star, Personal Recovery Plan, etc.
- Provision of training and education to the ward community and wider areas of the forensic services (and the Trust) co-produced by patients and ward staff. This shared their experience of implementing the recovery approach within the ward and the benefits of a hospital stay where hope, opportunity and control are emphasised.
- Promoting service user involvement in policy and procedure revisions, including a revised ‘Engagement and Observation’ policy. Inclusion of service user and carers in risk assessments.
- Providing service users with greater opportunities for choice regarding the therapeutic options provided on the unit.
The TRIP process thus provided a model for increasing collaboration between staff and patients on the ward.
As the team progressed in their journey towards implementing a recovery-oriented service to the women admitted to the ward, they increasingly began to work in partnership. Service users and staff introduced a weekly morning session on the ward where they focused on implementing the team recovery plan as a ward community. Aspects of the environment were changed to facilitate a sense of community and encourage the women to be active agents in their recovery. Service users and carers were actively involved in clinical team meetings and in Care Programme Approach meetings, with a focus on supporting service users to participate throughout their care reviews, including by chairing the meetings in some instances. A strengths-based approach was adopted, focusing on what the service users could do and not just on what they could not do. A sense of community was cultivated, through activities such as planning and preparing community meals. A sense of emotional belonging was cultivated by marking special events, birthdays, anniversaries etc with cards, messages of hope and discussions in ward-based community meetings. Likewise, endings, such as service users and staff leaving the ward, were marked as important transitions in the life of the ward community.
To support the staff team in their responses to the women’s needs, regular staff team reflective practice groups were re-instated, with the facilitation of a psychotherapist from the forensic services psychotherapy department of the Trust.
The effect on the ward was dramatic. Incidents of violence, self-harm, complaints and safeguarding referrals all decreased markedly, as did the use of seclusion. Service user progression through the ward increased which had the effect of inspiring hope regarding recovery for other. Staff morale improved and sickness and turnover of staff reduced. Importantly, staff and service users spoke of feeling proud to be part of this ward community which became a vibrant, gender-sensitive service supporting the recovery of women requiring medium secure care in keeping with the principles of the National Women’s Mental Health Strategy.
Long periods of time in secure care can feel like stagnation, even going backwards, and this is obviously damaging to hope and self-belief (Allen, 2010). Evidence of progress is therefore very important to service users and this was a key message from the workshops. People said that visible and concrete evidence of progress, “steps in the right direction” were needed, even if there were setbacks – perhaps especially if there were setbacks. Peer feedback is a defining feature of therapeutic communities in prison settings and it is interesting to note that some European countries, such as Holland, also include this as routine in secure settings. Concerns regarding confidentiality and boundaries can make this challenging in UK settings, but these are not insurmountable obstacles.
Transition to the Community
Forensic services can support individuals to develop their citizenship roles in the community by involvement with voluntary groups, work or training (see below). This will help build their confidence and support their sense of agency and recovery (Dowling & Hutchinson, 2008). Collaborations and partnerships with local art galleries, libraries, RSPCA, gyms, museums, garden centres, community football projects, conservation projects and charities have been successful in a number of settings. As well as broadening people’s horizons and giving them access to more positive social networks these opportunities also encourage the person to develop pro-social behaviours and skills in a ‘real world’ environment. Of course, they must be combined with a positive approach to risk-taking and ‘safety planning’ (Boardman & Roberts, 2014).
Key area II: The quality of relationships
“Caring is simple, but it is not necessarily easy. The young woman who cared for me was made like that – she understood what was needed and she could provide it” (Former service user, high security hospital).
As indicated earlier, the quality of relationships between service users and the staff who work with them are central to people’s recovery journeys (Slade et al., 2014). This is the case whether the encounters are very brief, or extend over many years. Recovery-promoting interactions almost always involve a degree of collaboration and some form of emotional connection or bond (Martin et al., 2000; Moore et al., 2002). These are shaped by the specific characteristics of the ward or unit and the overall culture of the organisation. Recent inquiry reports have examined the culture of organisations where basic care has gone wrong (e.g. Francis Report, 2013). They focused attention on the importance of compassion, consideration and commitment in the delivery of care.
A recovery-oriented service that has a focus on the quality of relationships will need to offer a range of staff supports, such as clinical supervision groups, team reflective practice, and individual supervision, to promote reflective thinking and adaptation by staff in relation to the challenges that arise (Adshead, 2010; Aiyegbusi & Clarke-Moore, 2008; Aiyegbusi & Kelly, 2012; Bartlett & McGauley, 2010; Moore, 2012).
“It helps me when I see positive dynamics in the staff team; the right people doing the right job.” (Former service user, medium secure unit)
Forming a supportive, professional relationship takes time, perseverance and skill. Sometimes it involves just being ‘ordinary’: listening, keeping a conversation going, saying very little sometimes, not avoiding tricky subjects and laughing together. There are always barriers to working together – mistrust, negative attitudes, language and cultural obstacles – but having a common purpose and mutually agreed expectations are key. Service users value when staff show interest in the task and share some hope and vision for the possibility of positive change. It is very important in secure services that ‘relational security’ complements the necessary physical (walls and fences) and procedural security (rules and guidelines) and staff need to take an active responsibility for their part in promoting safe and constructive working relationships.
“I shouted at my primary nurse …. and a while later he knocked on my door and said to me, what was all that about? And in the end, we laughed and I realised that maybe he trusted me after all … and that was a good feeling.” (service user in a medium secure unit)
But, what happens when things go wrong? Several authors who have focussed on ‘difficult’ exchanges and breaches of boundaries have highlighted the value of thinking about ‘windows of opportunity’ in forming working relationships (Koekkoek et al., 2010; Gutheil & Brodsky, 2008).
Defining the boundaries of interactions involves weighing up the options about how to respond in any given situation. Often people have to respond quickly, thinking on their feet. Managing boundaries well involves knowing the patient and being well-prepared. Boundaries have to be firm, yet flexible, so that they protect patients and staff and do not create further barriers that impede recovery (Lazarus, 1994). It also needs to be remembered that over-reactions or the misapplication of sanctions can be as harmful as under-reaction.
Box 6: Key ‘Do’s’ and ‘Don’t’s’ for staff wishing to achieve constructive alliances in forensic settings
DOs
- Make time to talk and listen
- Collaborate
- Be open but clear about limits; know how to ‘draw the line’
- Use common sense
- Show enthusiasm for your job/the tasks
- Communicate confidence in your patients wherever possible
- Appreciate the impact of even small decisions
- Remain sensitive to the need for confidentiality
DON’Ts
- Forget to listen/have a closed mind about what is being said
- Forget to include/ or worse, actively exclude service users
- Cross or break boundaries/rules/show favouritism
- Go along with unhelpful practices just because ‘we’ve always done this’
- Become disconnected from the reason you took the post in the first place
- Lack confidence in patients
- Think, “oh that won’t matter…”
- Over-expose patients to questions/ distress: (“go at my pace”)
Box 7: Top Tips on ‘How to get well and stay well’
- When in hospital use the support and practise skills.
- Make sure you have things to do that you enjoy and have time to relax.
- Find at least one person to laugh with and pour our heart out to.
- Try to like yourself (mostly) and others by building friendships.
- Talk to someone when things are difficult.
- Remember you have choices about what you want to do.
- Find time to do the things you like to do and can do.
- Try new and helpful things now and again.
- Recognise there are some things about life that cannot be changed, in the short term.
- Try to feel reasonably good about where you are.
- When you feel bad, you may make yourself feel better if you ask for help when you need it.
- When others feel bad or need help, you are there for them.
- Take your medication and attend therapy.
Reproduced with permission from the Ravenswood House, Southern Health NHS Foundation Trust, ‘A Journey of Recovery’ leaflet produced by service users.
Service user’s at Ravenswood House, a medium secure unit in Hampshire, also developed a list of ‘Top Tips’ on ‘How to get well and stay well’. These complement the staff ‘Do’s and Don’ts’ and are shown in Box 7 above.
Key area III: Risk and safety
The management of risk is, of course, fundamental to the success or failure of a forensic service aiming to support recovery. Despite acts of violence, many of the individuals in forensic mental health settings are also among the most vulnerable individuals in society (Adshead, 2000). For many, the road to recovery starts with feeling safe. This often begins with feeling in control of oneself, having relationships that are characterised by hope, trust and compassion and by having safe living conditions (Borg & Kristiansen, 2004).
When recovery begins in secure settings it needs to be recognised that the pathways by which individuals may seek control and safety may still be harmful. Jason’s story highlights real difficulties in his relationships with the people who are trying to help him. Other patients may be intimidating or violent. Managing these behaviours, and the distress that often underlies them, means that certain restrictions and professional boundaries are needed for the safety of all. But, along with the necessity for safety and security, can come a culture of control. This has the potential to lead to a risk-averse culture, defensive practice, paternalism, and overcontrol (Moore, 1995; Langan & Lindow, 2004). It is therefore crucial in recoveryoriented services to ensure that boundaries and restrictions are focused upon creating a culture of safety as a foundation for recovery. The most effective way to do this is for each organisation’s culture to be developed by staff and patients working together.
Working together to create a culture of safety means supporting people to understand how their life experiences have contributed to their risk and the impact that this has had upon their safety and the safety of others. Thus, the management of risk and safety needs to be as collaborative as any other aspect of the person’s care in recovery-oriented services (Boardman & Roberts, 2014). This collaboration should be overt and transparent, both the person and the staff supporting them feeling safe, while acknowledging the difficulties and continuing to encourage hope and growth (Barker, 2012).
In all decisions, the benefits of positive outcomes need to be balanced against the consequences of negative outcomes. “Positive risk-taking” (PRT) has been the favoured term to refer to decisions that enable patients to move forward (Morgan, 2004; Department of Health, 2007). It has been described as being, “… necessary in each aspect of mental health where the primary purpose is that of improving quality of life of service users” (Ramon, 2004). Others have noted that, “the benefits may serve as the reasons why risks are taken; the losses may refer to any possible undesirable consequences” (Robertson & Collinson, 2011). PRT gives people in Jason’s situation the opportunity to test-out and demonstrate better selfmanagement through graduated reduction in restrictions and boundaries. Constructed in an explicit and collaborative fashion, this has the potential to build trust between the person and their clinical team and has been endorsed as best practice in managing risk (Department of Health, 2007).
However, the process by which PRT is undertaken is poorly understood and underresearched. Within our workshops there was little consensus concerning PRT. Indeed, the language of ‘positive risk-taking’ was challenged as being unhelpful, inviting the perception that such activities were ‘risky’ and therefore needed to be avoided. As an alternative, one patient called this process “safety-testing” as opposed to “positive risktaking”. He described it as being, ‘like the electrical plugs in my room, you have to test any new equipment for electrical safety…. going out on unescorted leave is like that, you’re testing me to see if I can be safe, so I can prove it’. This concept of ‘safety-testing’ seems a useful way of describing a different approach to risk management where the emphasis is on helping the person pursue their chosen goals safely. We have therefore used the term ‘safety planning’ in our recent briefing examining recovery-oriented approaches to risk (Boardman & Roberts, 2014).
‘Safety planning’ is co-constructed between the person and the team they are working with; it requires a foundation of relational security (Department of Health, 2010). The service itself should acknowledge that taking a risk is a fundamental part of human growth and learning, and that the perception of a person’s offending risk must be balanced accurately against the need for them to be provided with appropriate opportunities to recover (Langan, 2008). Boardman & Roberts also argue that there is a need to make a distinction between ‘major risks’ that need to be minimised and those ‘everyday risks’ that people should be entitled to experience. In secure services this distinction is easily blurred, leading to a generally a risk-averse culture.
A recovery-oriented approach to risk assessment and management should move explicitly from external control towards the person demonstrating they can use internal mechanisms to take back control themselves. Each step along the continuum of risk-sharing should be supported by creating ‘optimal choices’ for patients within a framework of a professional duty of care. With individuals like Jason, who have the restrictions of a hospital order, the evidence for the effectiveness of such a ‘personal safety plan’ must be of sufficient standard to reassure a Mental Health Tribunal and the Ministry of Justice that the person can live safely in lower security settings or in the community.
Organisational support for ‘safety planning’ also needs to be clear, with transparent processes and appropriate guidance. The use of clear processes, which involve collaboration and discussion as the default, and do not simply rely on filling in standardised questionnaires, is likely to produce more effective risk management plans as well as plans that the person is more likely to stick to. Clear structures and support for staff in acknowledging that recovery always involves some element of risk is then necessary to facilitate the adoption of these new approaches. Far from ignoring risk, a recovery-oriented approach therefore demands that staff use all their professional skills in forming trusting relationships and understanding patients’ priorities to come to more sophisticated and better informed management plans.
Risk and ‘strengths’
Risk assessments that highlight the person’s strengths and their existing coping skills present a much more rounded picture of the person. Indeed, it has been suggested that risk assessments that fail to balance risks with strengths are inherently inaccurate (Rogers, 2000). We should therefore be careful of assessments which are couched in negative or pejorative language. A recovery-based approach which incorporates strengths-based approaches (e.g. SAPROF – Vogel et al., 2009, or START – Webster et al., 2004) are helpful in these respects. A ‘strengths-based’ approach should assist people in accessing opportunities for personal recovery and growth, while also maintaining their safety and the safety of the public.
A further example of going beyond a narrow focus on risk to developing recovery opportunities is the “Good Lives” model (see www.goodlivesmodel.com; Ward, 2002). In this approach people are encouraged to consider what they have been trying to achieve in their lives and how the process by which they have tried to achieve this has been adaptive or maladaptive. The programme assists individuals to consider how they want their lives to be different, while reflecting on the realities of their lives and building accessible support networks to cope with those realities. Its focus is positive and it incorporates elements of discovery for offenders as well as recovery, challenging them to consider what the elements of a ‘good life’ would be and how they can achieve it. The approach has been shown to have an impact on offending behaviours such as sexual offending (Willis & Ward, 2013), but has only recently been applied to offenders with mental health problems (Robertson, Barnao & Ward, 2011).
Box 8: Reflections on Jason – James Wooldridge
I’ve been asked to comment on risk as this is a huge topic regarding patients in secure hospitals. One factor in assessing risk is the level of remorse. Although I fully realise that I have been a risk to others and that is why I was in hospital, in my own personal journey I have had to consider that as a result of my offence I have received the help and support that I so badly needed. I can see that from a very bad situation there have been some positive outcomes. It has been good for me to confront the aspects of my life that were damaging my future. An aspect of this that concerns me is that some people who feel unsupported in the community commit a crime in desperation, as a ‘cry for help’. The help is then provided but when a criminal record is added to a mental health condition, the stigma that person faces is far greater and the potential for recovery suffers as a result.
One common dilemma many patients face is knowing how much (or how little) to share with their care team when experiencing distressing or frightening thoughts. Shortly before my discharge from forensic services I had thoughts about handling sharp knives that concerned me. My experience of intrusive thoughts in the past told me that this could be down to recently coming off some sedative medication that was causing some sleeplessness and giving me more time at night to think about the implications of going home. I also knew that I had never acted on disturbing thoughts in the past and I was clear on the fact that thoughts don’t necessarily lead to actions. I had a choice: tell my care team and risk my discharge being postponed or self-monitor for a few days and see if the situation improved. Fortunately, the thoughts stopped as my sleep pattern stabilised and I suppose my twenty years’ experience of living with a mental health condition provided me with the self-confidence required to see this through.
The situation above could be seen as an example of positive risk-taking and how I effectively ‘safety-tested’ myself. This involved understanding the nature of the risk, the implications and then how to monitor progress.
Key area IV: Opportunities for building a ‘life beyond illness’ – Meaningful occupation
Activities that provide meaningful occupation have a central role in promoting recovery in mental health (Strickley & Wright, 2011) – so much so that the recovery journey has been described as an occupational journey (Kelly, Lamont, & Brunero, 2010). Activities that are meaningful, interesting and fulfilling are both the means by which people recover their sense of being in the world and an outcome of recovery (Sutton, 2008). Meaningful occupation provides purpose, structure, routine and pleasure. These all contribute to a sense of personal agency. The skills and competence developed as a result of taking part in meaningful activity increase an individual’s horizons and provide opportunities to build a life beyond the secure setting. They are something to wake up for. Filling time with personally meaningful activities restores a sense of value and purpose to life promoting hope and a belief that the individual can still pursue their dreams (Hammell, 2009; Kelly et al., 2010; Mee & Sumison, 2001; Pierce, 2001; Whalley-Hammell, 2004).
If Jason is going to develop a life beyond illness that is meaningful to him he will first need to figure out what this means. An activity is meaningful when it fits with a person’s values, goals and sense of self (Lloyd et al., 2007). With his unsettled background and few achievements in life so far, Jason may not have ever considered what makes his life worth living. Previous meaningful occupations may have been anti-social, harmful, even criminal (Twinley, 2013). People like Jason are therefore faced with particular challenges in finding activities which are pro-social and health affirming (Cronin-Davis, Lang, & Molineux, 2004; Twinley, 2013).
A starting point to support someone like Jason may be to look back on what he has done before, using a strengths approach, and to identify how different activities have influenced his sense of wellbeing (Lindstedt, Söderlund, Stålenheim, & Sjödén, 2005). Also, the more that his environment can offer space for exploration and opportunities to try things out, the more he can begin to find out for himself his interests and priorities. At a basic level, ward programmes that directly involve patients in the planning and delivery of activities will empower them to help themselves (Rebeiro et al., 2001; Alred, 2003). They also contribute towards a stable, predictable structure and routine which forms the bedrock of the unit community and culture.
Staff attitudes are crucially important in this process and knowledgeable staff who take time to get to know the service user and provide the right level of support at the right time are fundamental. Jason will need to work at his own pace: fear of failure may hold him back. Staff need to be sensitive to this and ensure that activities are pitched at the right level so that individuals can always experience some success. When individuals participate in activities that are emotionally and cognitively demanding there will be a need for restorative, recuperative time. For example, in the later stages of Jason’s admission, he may be participating in challenging work around his offending behaviour, other activities may then be an important counter-balance, providing solace, refuge and a place to ‘recharge the batteries’.
Rather than simulated work programmes, forensic services are now encouraged to strive towards activities that are authentic and associated with community living (Townsend, 1997). This requires the development of interventions that tackle the systemic issues within the wider service, such as policies on access to the community, social inclusion and employment programmes which facilitate or obstruct the development of working alliances with a range of community-based settings (Cronin-Davis et al., 2004). This process can start by inviting people with a range of experiences onto the secure units including artists, teachers, musicians, animal handlers, magicians and sports experts. They bring creative ideas, energy and new perspectives and provide an opportunity to challenge stigma through integration.
Advice from our workshops included: “start small and be inclusive”; “it takes time to build relationships”; “It has taken years to build trust with colleges and community resources but the benefits have been worthwhile”.
Open employment
Most people with mental health problems want to work (Grove, Secker & Seebohm, 2005) and for people who also have forensic histories finding meaningful employment in the ‘real world’ is a key part of their recovery (Davies et al., 2007). Jason presents particular problems to employment specialists (and employers) because of his combination of mental health problems and offending history, but he should not be regarded as impossible to support into open employment. The ‘Individual Placement and Support’ (IPS) model (Becker, Drake & Concord, 1994) has been used successfully with a variety of people with severe and enduring mental health difficulties and substance misuse problems and is recommended for forensic offenders (SOFMH/NHS Scotland/Scottish Government, 2011). In mainstream mental health services IPS has been evaluated in a number of randomised controlled trials and has consistently been found to be more than twice as effective as any other approach in maintaining people with severe psychiatric difficulties in paid employment (Burns et al., 2007; Bond, Drake & Becker, 2008; Porteus & Waghorn, 2007; Rinaldi & Perkins, 2007). It is currently being tested by the Centre for Mental Health in a trial with prisoners who have mental health problems and being released into community teams (Durcan, 2014).
Although IPS is the most effective way of helping people into paid employment, as indicated above, there are a number of other possibilities in terms of voluntary roles in a variety of community settings. Open employment should not, therefore, be seen as the only – or the most superior – occupational outcome. It depends on the person and what they want to do. IPS is important because it has demonstrated that we now have an approach which can help people with offending histories and mental health problems into paid employment should they wish to do so.
Key area V: Peer support
‘Peer support’ roles are unique in terms of seeing the person’s experience of using forensic services as a positive advantage when it comes to selection and recruitment. Of course, gaining support from people who have had similar experiences has been a feature of human interaction for as long as humans have been around in groups and communicating with one another. Similarly, the importance of naturally occurring friendships between peers has long been recognised in the mental health field and peer support worker posts, voluntary and paid, have been established in both third sector and statutory mental health services. The ImROC programme believes they are particularly important in terms of supporting recovery in mental health (Repper 2013a; 2013b).
But, peer support worker posts are still rare in forensic services. There are a number of reasons for this:
- Historically, expertise has focused on what is provided by mental health workers and service users are assumed to have to be passive, rather than active, contributors to this process (Boehm et al., 2014).
- Focus groups on the possibility of establishing a mentoring system in a secure hospital, suggested competition between staff and peer workers played a role in the difficulties of establishing such roles (Boehm et al., 2014).
- In order to provide peer support based on shared experiences, the peer worker would ideally have personal experience of both mental health problems and secure services. However, many people who have used secure services do not want to remain connected to the system once they have left, or have not been encouraged to take on a new role in relation to where they received secure care.
- While current legislation is supportive of the employment of people with mental health problems, many remain excluded from the workforce. There are particular anxieties about employing people with offending histories to work alongside potentially vulnerable people in secure services.
- Additional concerns relate to the wellbeing of the peer workers themselves – it can be stressful and potentially (re) traumatising for anybody to work in secure settings.
Despite these problems, there are examples of peer workers serving a unique and valuable function in secure settings. For example, Baron (2011) describes the emergence of this new role in the US: “Forensic Peer Specialists (FPSs) are now working one-onone with referrals from mental health and drug courts to provide the otherwise unavailable ongoing support consumers may need to avoid incarceration in the future. A few FPSs work with individuals inside jails and prisons to develop re-entry plans that ensure a smooth transition to community life. Most FPSs, however, work within community-based re-entry programs to provide both personal encouragement and practical assistance in the months following release” (p. 1).
In this example, forensic peer specialists served as community guides, coaches, and advocates, working to link recently discharged people with housing, vocational and educational opportunities, and community services. Within this context, they can model useful skills and effective problem-solving strategies, as well as responding to crises. In England, Together (see www.together.org.uk) is leading a new project scoping the development of peer worker posts in secure services. Thus, there is a small, but growing, cohort of paid support worker posts in secure services.
There are also many examples of unpaid peer support. ‘Buddy’ systems and ‘listening’ projects are common in many secure settings. Patients who have been on a unit for a longer time provide support to newer patients, offering a welcome to the unit and information to familiarise them with the routines and expectations of the environment. Within secure services, these have developed from the impetus provided by the requirement for a “buddy system” as part of the implementation of ‘My Shared Pathway’ (Ayub, et al., 2013). A project called “Peer+” at Kneesworth House Hospital1 has developed these roles even further, with formalised training and dedicated on-going supervision for a team of Peer+ workers across all wards.
Patients who have completed an episode of care in a particular unit can also be invited back to support those who are earlier in their treatment pathway (e.g someone who has been through a particular therapy group might come back to help to deliver and engage subsequent group members). Similarly, people who have moved on may return to the unit to talk to existing patients about their journey. This can inspire hope and belief in the possibility of a future after discharge (Davidson et al, 1999).
Recovery Colleges
One of the most exciting new developments supporting the recovery of people using mainstream mental health services is the ‘Recovery College’ (Perkins et al, 2012). These are places where service users can deploy their knowledge and experience of mental health issues (‘experts-by-experience’) working alongside professionals to design and co-deliver ‘courses’ on topics they identify as relevant to a mixed audience of service users, professionals and family members. Courses may vary in length from a single session to a fully accredited training programme. Recovery Colleges have proved extremely popular and appear to produce range of very positive outcomes (McGregor, Repper & Brown, 2014). Most Colleges are organised on a ‘hub-and-spoke’ model, with a central ‘hub’ in the mental health service and ‘spokes’ in a variety of community settings. Some Colleges are now beginning to deliver ‘spokes’ in forensic settings (high, medium or low secure).
The role of the peer can transform what have often been very negative experiences into something positive, “I’ve been through a lot in my time, now I want to give something back, helping other people who come after me”. This gives personal satisfaction and may be a powerful element in a reparative process. It is also inclusive in that everyone has experiences to share that may be useful to others. Of course, not everyone will be interested in participating, but for those that can work in this way they can be genuinely transformative.
Box 9: James Woolridge – Reflections
I’ve reflected on what’s been written in this document so far and what lessons I’ve personally learnt from being a secure patient. I do this not only because it is healthy for me to express my feelings and thoughts on what has happened in my life but also because it could help someone else who may have walked a similar path. My well-being was helped greatly by the realisation that many of the staff wanted what I wanted – that is to move on and leave secure services. Rather than fight the system from within, which ultimately led to life being harder, it dawned on me that if I worked with the staff then I stood a much better chance of achieving my goals.
A nurse once thanked me for sharing something that they learnt from talking to me. This was very important as I realised that learning is a two-way street and I welcome the development of Recovery Colleges where everyone’s a student and the emphasis is on learning together. I truly hope that some of my fellow patients realise that there is great comfort in knowing that someone who has experienced similar, life-changing events can live a productive life even with the limitations that come with being, or having been, a secure patient.
Whilst I mentioned remorse earlier and how this has to be balanced with the fact that I received the help and support I was so desperately crying out for, I am also aware of the ‘ripple effect’ my crime of setting two fires on a hospital ward and how this impacted on my fellow patients, the nurses on the ward, my family, my work and my life in general. My wife told me that at one point during my time as an inpatient she had approached a solicitor about divorce proceedings and the thought that I could have lost everything I hold so dear is a reminder of the severity of my crime.
In a strange way my experience of secure services helped me to take responsibility for my actions and provided a long, sharp shock. It also provided me with additional experience of mental health service provision and if it hadn’t been for my crime, I wouldn’t have been asked to contribute to this document.
Quality and outcomes
The problems of measuring quality and outcomes in services to support recovery are considerable. Specifying quality indicators means that we need to know which aspects of care are reliably associated with specific positive outcomes; identifying reliable outcome indicators depends on everyone agreeing what recovery-oriented services should be striving to achieve.
In both respects, this is not easy simply because the application of recovery principles is so new that the evaluative research is lacking. Notwithstanding, it is possible to identify some quality indicators in mainstream mental health services which do receive general support and some outcome indicators that most people agree on (Shepherd et al., 2014).
In forensic services, the lack of research linking recovery practices to outcomes is even greater, but much of this paper has been devoted to try to articulate quality indicators for care at both an individual and an organisational level. These are summarised in Box 10.
Box 10: Quality indicators for recovery supporting forensic services at the level of individual and organisational care
Individual level care
- Specific attempts are made to build high quality, trusting relationships from the beginning.
- A strengths-based approach is used to underpin care planning.
- Shared decision-making is used routinely in care planning.
- Service users are provided with information about the alternative treatments available (medical, psychological, social).
- Necessary rules and restrictions (‘boundaries’) are explained clearly.
- Service users report feeling safe in the environment.
- Service users are routinely involved in planning how to pursue their chosen life goals in ways that are safe for them and others (‘safety planning’).
Organisation of care
- There is reasonable consistency of staffing.
- Service users routinely participate in co-producing policies and procedures.
- Service users routinely participate in co-designing and co-delivering the ward programme.
- Service users routinely participate in co-designing and co-delivering staff training.
- Service users are routinely involved in staff selection and appraisal.
- The unit provides access to a range of occupational activities.
- The unit has good links with a range of community agencies who can offer placements.
- The unit has access to specialist vocational staff who have received training in the ‘Individual Placement and Support’ (IPS) model.
- The unit employs appropriately trained peer support workers.
- The unit provides Befriending or ‘Listening’ schemes.
- The unit regularly uses the ‘Team Recovery Implementation Plan’ (TRIP) as a way of assessing and improving the recovery-oriented practices.
- Service users have access to ‘Recovery College’-type provision.
This list could be operationalised and used as a check-list for assessing and developing the service. This would be best achieved through a process of co-production.
In relation to outcomes, there is greater commonality for people in forensic services and those in mainstream mental health services. We would therefore argue that the same list of outcome measures as ImROC proposed for mainstream services could be used here, perhaps with minor modifications. These are shown in Box 11.
Box 11: Summary recommendations for recovery outcomes measures (based on Shepherd et al., 2014, Supporting Recovery in Mental Health – Quality and Outcomes, Centre for Mental Health, London).
Definite
DOMAIN 1 – Quality of recovery-supporting care – To what extent do service users feel that staff in services are trying to help them in their recovery? Recommended measure: INSPIRE.
DOMAIN 2 – Achievement of individual recovery goals – To what extent have goals, as defined by the individual, been attained over time? Recommended measures: Goal Attainment Scaling (GAS), narrative accounts.
DOMAIN 3 – Subjective measures of personal recovery – To what extent do individuals feel that their hopes, sense of control and opportunities for building a life beyond illness have improved as a result of their contact with services? Recommended measure: Questionnaire on the Process of Recovery (QPR).
DOMAIN 4 – Achievement of socially valued goals – Has the person’s status on indicators of social roles improved as a result of their contact with services? Recommended measures: Relevant items from Adult Social Care Outcomes Framework (2012), Social inclusion web.
Possible
DOMAIN 5 – Quality of life and well-being – Has the person’s quality of life and/or well-being improved? Recommended measures: MANSA, WEMWBS.
DOMAIN 6 – Service use – As a result of their recovery being supported, has the person made an appropriate reduction in their use of other mental health services? Recommended measures: Relevant items from Mental Health Minimum Data Set & NHS Outcomes framework (but beware!).
Conclusions
We began with asking a simple question of our workshop participants: “What helps and what hinders recovery?” What emerged from those conversations was that recovery for forensic service users is, in many respects, identical to recovery for mental health service users in non-forensic settings. But, the recovery journey of people in forensic services is significantly different from others in one crucial aspect: people with offending histories have to address in some way the reality of what they have done and what brought them to forensic services. For forensic service users, personal recovery therefore needs to include offender recovery. This means addressing guilt, shame, confusion, turmoil – sometimes denial – with sensitivity and respect. If this can be done in such a way that the person is helped to ‘come to terms with themselves’ then personally defined recovery becomes genuinely possible.
Support for personally defined recovery should therefore be incorporated into mental health and well-being interventions for people in forensic services, just as for those outside of them. Risks need to be identified and managed so that the person can pursue their hopes and dreams safely. High quality relationships of trust and collaboration need to be built between service users and staff and service users should be able to participate as fully as possible in all aspects of their care through informed choices and shared decision-making. Care planning needs to be founded on the person’s strengths, while acknowledging their difficulties. Organisations then need to commit to developing a culture of safety for service users and staff and provide support for staff in maintaining their support for recovery. Trusts, directorates and leadership teams need to consider how they can invest in transforming the culture and practices in their services to prioritise recovery. Finally, contact with the wider community – peers, family, friends and informal social networks – needs to be actively encouraged – it provides the strongest foundation for hope and a positive sense of identity into the future.
Box 12: Final reflections – James Wooldridge
Thinking about Jason and recovery in this document has been challenging for me in many ways. I first heard about recovery as a way of living whilst a patient in secure services and I truly believe – then and now – that those who work in secure services have a far greater opportunity to work to support recovery than staff in acute ward settings. This is because in the acute settings I’ve experienced staff levels are lower, staff/patient interactions are limited and the emphasis seemed to be on throughput rather than high quality care.
In discussing these issues I tried to include many of the dilemmas that I personally faced whilst a patient, such as disclosure, remorse, having bad days, as well as the frustrations of being in such a closely-monitored environment. Above all, I wanted to convey a sense of hope. This is the cornerstone of recovery and needs to be nurtured by both staff and patient alike. In my recovery I would particularly acknowledge the role that my wife, my work, my music and my dog have played in maintaining my hope and supporting my recovery. Thanks to them and to all of you for reading this.
References
Adshead, G, (2000) Care or custody? Ethical dilemmas in forensic psychiatry. Journal of Medical Ethics 26, 302–304
Adshead, G. (2010) Introduction to ethics. In: A. Barlett & G. McGauley (Eds), Forensic Mental Health: Concepts, systems, and practice (pp. 293-294). Oxford: Oxford University Press.
Adshead, G. (2012a). Their Dark Materials: Narratives and Recovery in Forensic Practice. (http://www.rcpsych.ac.uk/pdf/Their%20 Dark%20Materials.%20narratives%20and%20 recovery%20in%20Forensic%20Practice%20 Gwen%20Adshead.x.pdf. Accessed on 24 June 2013)
Adshead, G. (2012b) This thing of darkness: Index offence work and recovery. Paper presented at the 5th Forensic Implementing Recovery through Organisational Change (ImROC) Seminar “Promoting recovery through positive working alliances”, The Learning Centre, South Staffordshire & Shropshire Healthcare Foundation Trust, 11 October 2012.
Aiyegbusi, A. & Clarke-Moore, J. (2008) Therapeutic Relationships with Offenders: An Introduction to the Psychodynamics of Forensic Mental Health Nursing
Aiyegbusi, A. & Kelly, G. (2012) Professional and Therapeutic Boundaries in Forensic Mental Health Practice. London: Jessica Kingsley Publishers.
Allen. S. (2010) Our Stories: Moving On, Recovery and Well-being. South West London & St. George’s Mental Health Trust Forensic Services.
Alred, D. (2003) Programme Planning. In: L. Couldrick & D. Alred (Eds.), Forensic Occupational Therapy. London: Whurr.
Ayub, R., Callahan, I., Haque, Q. & McCann, G. (2013) Increasing patient involvement in care pathways. Health Services Journal, 3 June 2013. (http://www.hsj.co.uk/ home/commissioning/increasing-patientinvolvement-in-care-pathways/5058959.article)
Barker, R. (2012) Risk and Recovery: Accepting the complexity. In: G. Drennan & D. Alred (Eds), Secure Recovery: Approaches to Recovery in Forensic Mental Health Setting (pp. 23-40). London: Routledge.
Baron, R. (2011) Forensic Peer Specialists: An Emerging Workforce. Center for Behavioral Health Services & Criminal Justice Research, Policy Brief, June 2011.
Bartlett, A. and McGauley, G. (2010) Forensic Mental Health: Concepts, systems, and practice. Oxford University Press: Oxford.
Becker, D.R., Drake, R.E. & Concord, N.H. (1994) Individual placement and support: a community mental health center approach to vocational rehabilitation. Community Mental Health Journal, 30, 193-206.
Boardman, J & Roberts, G. (2014) Risk, Safety and Recovery, ImROC Briefing Paper 9. London: Centre for Mental Health and Mental Health Network, NHS Confederation.
Boehm, B., Tapp, J., Carthy, J., Noak, J., Glorney, E. & Moore, E. (2014) Patient Focus Group Responses to Peer Mentoring in a High Security Hospital. International Journal of Forensic Mental Health, 13: 1–10.
Bond, G. R., Drake, R.E. & Becker, D. (2008) An update on randomized controlled trials of evidence-based supported employment. Psychiatric Rehabilitation Journal, 31, 280-290.
Borg, M., & Kristiansen, K. (2004) Recoveryoriented professionals: Helping relationships in mental health services. Journal of Mental Health, October 2004; 13(5): 493 – 505
Bowser, A. (2012) Nothing for us without us either. In : G. Drennan & D. Alred (Eds), Secure Recovery: Approaches to Recovery in Forensic Mental Health Settings (pp. 41-54). London: Routledge.
Burns, T., Catty, J., Becker, T., Drake, R., Fioritti, A., Knapp, M., Lauber, C., Tomov, T., Busschbach, J., White, S. & Wiersma, D. (2007) The effectiveness of supported employment for people with severe mental illness: a randomised controlled trial, The Lancet, 370, 1146-1152.
Copeland, M. (2011). The Wellness and Recovery Action Plan. Peach Press: West Dummerston, VT.
Cronin-Davis, J., Lang, A., & Molineux, M. (2004) Occupational Science: The forensic challenge. In Molineux (Ed.), Occupational Science for Occupational Therapists. Oxford: Blackwell.
Davidson, L., Chinman, M., Kloos, B., Weingarten, R., Stayner, D., & Tebes, J.K. (1999) Peer support among individuals with severe mental illness: A review of the evidence. Clinical Psychology: Science and Practice, 6 (2), 165-187.
Davies, S., Clarke, M., Hollin, C. & Duggan, C. (2007) Long-term outcomes after discharge from medium secure care: a cause for concern, British Journal of Psychiatry, 191, 70-74.
Davies, S., Wakely, E., Morgan, S. & Carson, J. (2012) Mental Health Recovery Heroes Past and Present. Pavilion Press: Sussex.
Department of Health Secure Services Policy Team. (2010) See, think, act: Your guide to relational security. London: Department of Health.
Department of Health. (2007) Best Practice in Managing Risk: Principles and evidence for best practice in the assessment and management of risk to self and others in mental health services. London: Department of Health.
Dorkins, E. & Adshead, G. (2011) Working with offenders: challenges to the recovery agenda. Advances in Psychiatric Treatment, 17, 178-187.
Dowling, H., & Hutchinson, A. (2008) Occupational therapy – it’s contribution to social inclusion and recovery. A Life in the Day, 12(3), 11-14.
Drennan, G., & Alred, D. (2012). Secure Recovery: Approaches to Recovery in Forensic Mental Health Settings. London: Routledge.
Durcan, G. (2014). Employment for offenders. Available at http://www.centreformentalhealth. org.uk/employment/andoffenders.aspx. (Accessed 30th Jul 2014).
Eunson, H., Sambrook, S., & Carpenter, D. (2012)Embedding recovery into training for mental health practitioners. In: G. Drennan & D. Alred (Eds), Secure Recovery: Approaches to Recovery in Forensic Mental Health Settings (pp. 172-185). London: Routledge.
Ferrito, M., Vetere, A., Adshead, G., & Moore, E. (2012) Life after homicide: accounts of recovery and redemption of offender patients in a high security hospital – a qualitative study. Journal of Forensic Psychiatry & Psychology, 23(3), 327-344.
Francis, R. (2013) Implementing the recommendations to The Francis Inquiry: A Year On. http://www.healthcareconferencesuk.co.uk/francis-inquiry-a-year-on.
Grove, B., Secker, J. & Seebohm, P. (2005) New Thinking about Mental Health and Employment. Oxford: Radcliffe
Gutheil, T.G. & Brodsky, A. (2008) Preventing Boundary Violations in Clinical Practice. New York: Guilford Press.
Hammell, K. (2009) Self care, productivity and leisure, or diimensions of occupational experience? Rethinking occupational “categories” Canadian Journal of Occupational Therapy, 76, 107-114.
Hillbrand, M. & Young , J. L. (2008) ‘Instilling hope into forensic treatment: The antidote to despair and desperation’. Journal of the American Academy of Psychiatry and the Law, 36, 90 – 94.
Kelly, M., Lamont, S., & Brunero, S. (2010) An occupational perspective of the recovery journey in mental health. British Journal of Occupational Therapy, 73(3), 129-135.
Koekkoek, B., van Meijel, B., van Ommen, J., Pennings, R., Kaasenbrood, A., Hutschemaekers, G & Schene, A. (2010) Ambivalent connections: a qualitative study of the care experiences of non-psychotic chronic patients who are perceived as ‘difficult’ by professionals. BMC Psychiatry, 10: 96 http:// www.biomedcentral.com/1471-244X/10/96
Langan, J. (2008) Involving mental health service users considered to pose a risk to other people in risk assessment. Journal of Mental Health, 17(5), 471 – 481
Langan, J., & Lindow, V. (2004) Living with Risk: Mental Health Service User Involvement in Risk Assessment and Management, Bristol: Joseph Rowntree Foundation/The Policy Press.
Lazarus, A. A. (1994) How certain boundaries and ethics diminish therapeutic effectiveness. Ethical Behaviour, 4: 255-261.
Lindstedt, H., Söderlund, A., Stålenheim, G., & Sjödén, P. (2005) Personality traits as predictors of occupational performance and life satisfaction among mentally disordered offenders. Nordic Journal of Psychiatry 59(5), 357-364.
Lloyd, C., King, R., McCarthy, M., & Scanlan, M. (2007) The association between leisure motivation and recovery: A pilot study. Australian Journal of Occupational Therapy, 54, 33-41.
MacKeith, J. (2011) The Development of the Outcomes Star: A Participatory Approach to Assessment and Outcome Measurement. Housing Care and Support, Vol 14, No. 3. (http://www.outcomesstar.org.uk/storage/ outcomes-star-library/articles/Development-of-Outcomes-Star-in-Housing-Care-and-Support. doc, Accessed on 10.06.2014)
Maden, T. (2007) Treating violence: a guide to risk management in mental health. Oxford: Oxford University Press.
Martin, D.J., Garske, J.P. & Davis, K. (2000) Relation of the therapeutic alliance with outcome and other variables: a Meta-Analytic review. Journal of Consulting & Clinical Psychology, 3: 438-450.
Maruna , S. (2005) Making Good: How Exconvicts Reform and Rebuild Their Lives. Washington : American Psychological Association .
McGregor, J., Repper, J. & Brown, H. (2014) “The college is so different from anything I have done”: A study of the characteristics of Nottingham Recovery College, Journal of Mental Health Education, Training and Practice, 9, 3-15.
Mee, J., & Sumison, T. (2001) Mental Health Clients Confirm the Motivating Power of Occupation British Journal Of Occupational Therapy, 64(3), 121-128.
Mezey, G. & Eastman , N. (2009) ‘Choice and social inclusion in forensic psychiatry: acknowledging mixed messages and double think’. The Journal of Forensic Psychiatry & Psychology, 20(4), 503 – 507.
Mezey, G. C., Kavuma, M., Turton, P., Demetriou, A., & Wright, C. (2010) Perceptions, experiences and meanings of recovery in forensic psychiatric patients. Journal of Forensic Psychiatry and Psychology, 21(5), 683-696.
Moore, B. (1995) Risk Assessment: A Practitioner’s Guide to Predicting Harmful Behaviour. London: Whiting and Birch.
Moore, E. (2012) Personality disorder: its impact on staff and the role of supervision. Advances in Psychiatric Treatment, 18, 44-55.
Moore, E., & Drennan, G. (2013) Complex forensic case formulation in recovery-oriented services: Some implications for routine practice. Criminal Behaviour and Mental Health (Special Issue: Case Formulation with Offenders), 23(4), 230–240.
Moore, E., Yates, M., Mallindine, C., Ryan, S., Jackson, S., Chinnon, N. & Kuipers, L. (2002) Expressed Emotion in relationships between staff and patients in forensic services: changes in relationship status at 12 month follow-up. Legal & Criminological Psychology, 7, 203-218.
Morgan, S. (2004) Positive risk-taking: an idea whose time has come. Health care risk report. Downloaded from: http://practicebasedevidence.squarespace.com/ storage/pdfs/OpenMind-PositiveRiskTaking.pdf
NHS Confederation/Centre for Mental Health (2012) Supporting Recovery in Mental Health, Briefing paper, Issue 244. London: NHS Confederation.
Perkins, R., Repper, J., Rinaldi, M., & Brown, H. (2012) Recovery Colleges. London: Centre for Mental Health.
Pfafflin, F. & Adshead, G. (2004) A matter of security: The application of Attachment Theory to Forensic Psychiatry and Psychotherapy. London : Jessica Kingsley Publishers.
Pierce, D. (2001). Untangling occupation and activity. American Journal of Occupational Therapy, 55(2), 138-146.
Porteus, N. & Waghorn, G. (2007) Implementing Evidence-Based Employment Services in New Zealand for Young Adults with Psychosis: Progress during the First Five Years. British Journal of Occupational Therapy, 70, 521-526.
Pouncey, C. L. & Lukens, J. M. (2010) Madness versus badness: the ethical tension between the recovery movement and forensic psychiatry. Theoretical Medicine & Bioethics, 31, 93–105.
Ramon, S. (2004) Approaches to risk in mental health. A multidisciplinary discourse. In: J. Tew (ed.), Social perspectives in mental health: Developing social models to understand and work with mental distress (pp. 184-199). London: Jessica Kingsley.
Rebeiro, K., Day, D., Semeniuk, B., O’Brien, M., & Wilson, B. (2001) Northern Initiative for Social Action: An occupation-based mental health program. American Journal of Occupational Therapy, 55(5), 493-500.
Repper, J. & Perkins, R. (2003) Social Inclusion and Recovery: A model for mental health practice. London: Bailliere Tindall.
Repper, J. & Perkins, R. (2013) The Team Recovery Implementation Plan: A Framework for Creating Recovery Focussed Services. ImROC Briefing No. 6. London: Centre for Mental Health and Mental Health Network, NHS Confederation.
Repper, J. (2013a) Peer Support Workers: Theory and Practice, ImROC Briefing Paper 5. London: Centre for Mental Health and Mental Health Network, NHS Confederation.
Repper, J. (2013b) Peer Support Workers: A Practical Guide to Implementation, ImROC Briefing Paper 7. London: Centre for Mental Health and Mental Health Network, NHS Confederation.
Rinaldi, M. & Perkins, R. (2007) Implementing evidence-based supported employment. Psychiatric Bulletin, 31, 244-249
Rinaldi, M. & Watkeys, F. (2014) Do our current approaches to care planning and the CPA enhance the experience and outcomes of a person’s recovery? The Journal of Mental Health Training, Education and Practice, 9(1), 26-34.
Roberts , G., Dorkins, E., Wooldridge, J., & Hewis, E. (2008) ‘Detained – what’s my choice? Part 1’ Discussion. Advances in Psychiatric Treatment, 14, 172-180.
Roberts, G. (2011) ‘Forensic service user’: transitional identity or life sentence? Commentary on … Working with Offenders. Advances in Psychiatric Treatment, 17, 188-190.
Robertson, J., & Collinson, C. (2011) Positive risk taking: Whose risk is it? An exploration in community outreach teams in adult mental health and learning disability services. Health, Risk & Society, 13(2), 147-164
Robertson, P., Barnao, M., & Ward, T. (2011) Rehabilitation frameworks in forensic mental health. Aggression and Violent Behavior, 16, 472-484.
Rogers, R. (2000) The uncritical acceptance of risk assessments in forensic practice. Law and Human Behaviour, 24,595-605
Shepherd, G., Boardman, J. & Slade, M. (2008) Making Recovery a Reality. London: The Sainsbury Centre for Mental Health.
Shepherd, G., Boardman, J. & Burns, M. (2010) Implementing Recovery – A methodology for organisational change. London: The Sainsbury Centre for Mental Health.
Shepherd, G., Boardman, J., Rinaldi, M., & Roberts, G. (2014) Supporting recovery in mental health services: Quality and Outcomes. ImROC Briefing Paper 8. London: Centre for Mental Health and Mental Health Network, NHS Confederation.
Simpson, A. I. F., & Penney, S. R. (2011) Editorial: The recovery paradigm in forensic mental health services. Criminal Behaviour & Mental Health, 21, 299-306.
Slade, M., Amering, M., Farkas, M., Hamilton, B., O’Hagan, M., Panther, G., Perkins, R., Shepherd, G., Tse, S., & Whitley, R. (2014) Uses and abuses of recovery: implementing recovery-oriented practice in mental health systems. World Psychiatry, 13, 12-20.
SoFMH/ NHS Scotland / Scottish Government (2011) Towards Work in Forensic Mental Health National Guidance for Allied Health Professionals. Published by Forensic Network, The State Hospital, Carstairs, Lanark ML11 8RP. http://www.forensicnetwork.scot.nhs.uk/allied-health
Strickley, T., & Wright, N. (2011) The British Research Evidence for Recovery, papers published between 2006 and 2009 (inclusive). Part one: a review of the peer-reviewed literature using a systematic approach. Journal of Psychiatric and Mental Health Nursing, 18, 247-256.
Sutton, D. (2008) Recovery as the Refabrication of Everyday Life. Auckland University of Technology, Auckland.
Townsend, E. (1997) Occupation: Potential for personal and social transformation. Journal of Occupational Science, 4(1), 18-26.
Twinley, R. (2013) The dark side of occupation: a concept for consideration. Australian Occupational Therapy Journal, 60, 301-303.
Vogel, V. de, Ruiter, C. de, Bouman, Y., & Vries Robbé, M. de (2009) SAPROF. Guidelines for the assessment of protective factors for violence risk. English Version. Utrecht, The Netherlands: forum Educatief.
Ward, T. (2002) Good lives and the rehabilitation of offenders: promises and problems. Aggression and Violent Behavior, 7, 513-528.
Ward, T. (2013) Editorial: The dual relationship problem in forensic and correctional practice: Community protection or offender welfare? Legal and Criminological Psychology, 19(1), 35-39.
Webster, C. D., Martin, M., Brink, J., Nicholls, T. L. & Middleton, C. (2004) Short-Term Assessment of Risk and Treatability (START). St. Josephs Healthcare, Hamilton and British Columbia Mental Health and Addiction Services.
Whalley-Hammell, K. (2004) Dimensions of meaning in the occupations of daily life. Canadian Journal of Occupational Therapy, 71(5), 296-305.
Willis, G. & Ward, T. (2013) The good lives model: Does it work? Preliminary evidence. In L. Craig, L. Dixon, & T.A. Gannon (Eds.), What Works in Offender Rehabilitation: An evidence based approach to assessment and treatment (pp. 305-318). Chichester: John Wiley & Sons.
1 Linda Ram and Janet Bakht, Social Work Department, Kneesworth House Hospital, Partnerships in Care, together with a committed group of in-patient service users.
About the authors
Gerard Drennan is currently Consultant Lead Psychologist in Forensic and Offender Health Pathways at the South London & Maudsley NHS Foundation Trust. However, through out the time of working towards and preparing this ImROC Briefing Paper, Gerard was supported in his development and understanding recovery-oriented practice in offender mental health settings through working with the service users and staff of the Secure & Forensic Services of Sussex Partnership NHS Foundation Trust, while in the role of Professional Lead for Forensic Clinical Psychology & Psychological Therapies. Training as a Psychoanalytic Psychotherapist and as a Restorative Justice Facilitator have also shaped Gerard’s approach to supporting service users in their progress towards personally defined recovery.
James Wooldridge has been using mental health services for over 30 years following a major breakdown whilst undergoing officer training at the Royal Military Academy Sandhurst in the early 1980s. After a variety of occupations, including being a printer, buyer, salesman and fireman, James went self-employed as a trainer/speaker/recovery consultant in August 2005 and created Positive Notions. James currently runs Recovery Devon and is also the South West Coordinator for the national Time To Change campaign. Despite having been sectioned over 20 times and with three stays in secure services, James has been married to Lesley for over 20 years and lives in a cottage in rural North Devon. James lives by the values and principles of the recovery approach and spends much of his working life encouraging others to further their personal recovery.
Together with:
Anne Aiyegbusi, Interim Director of Nursing and Patient Experience, West London Mental Health NHS Trust
Debbie Alred, Consultant Occupational Therapist, Sussex Partnership NHS Foundation Trust
Joe Ayres, Lead for Occupational Therapy and Arts Therapies, West London Mental Health Trust
Richard Barker, Consultant Clinical & Forensic Psychologist, Oxford Health NHS Foundation Trust (previously of Birmingham and Solihull Mental Health NHS Trust)
Sally Carr, Specialist Practitioner – Recovery (Forensic), South Staffordshire and Shropshire Healthcare NHS Foundation Trust
Helen Eunson, Consultant Nurse Trainee, Southern Health NHS Foundation Trust
Hilary Lomas, Consultant Occupational Therapist, Mersey Care NHS Trust
Estelle Moore, Professional Lead for Psychology and Psychological Services, West London Mental Health NHS Trust
Debbie Stanton, Recovery Co-ordinator, Forensic Division, Nottinghamshire Healthcare NHS Trust
&
Geoff Shepherd trained originally as a clinical psychologist and has worked most of his career in the NHS as a practitioner, manager and researcher. He is currently employed leading the ‘ImROC’ programme based at the Centre for Mental Health and the NHS Confederation’s Mental Health Network. Geoff has a particular interest in applying recovery principles in forensic and prison settings and worked for some years with local mental health inreach teams in prisons in Cambridgeshire. He is also interested in employment issues for people with mental health problems. He holds a visiting chair at the Institute of Psychiatry and continues to be active in mental health services research.
Making Recovery a Reality in Forensic Settings
This briefing paper has been produced for the Implementing Recovery through Organisational Change programme, a joint initiative from the Centre for Mental Health and the Mental Health Network of the NHS Confederation.
The pilot phase of ImROC ran from 2011-12 and was supported by the Department of Health, together with contributions from the participating services. The continuing work of ImROC is endorsed by the Department of Health and managed and supported by the Centre for Mental Health and Mental Health Network.
For more information on the current work of ImROC, please visit imroc.org.
ImROC, c/o Mental Health Network, NHS Confederation, 50 Broadway, London, SW1H 0DB
Tel: 020 7799 6666
imroc@nhsconfed.org
imroc.org
This paper shows how Team Recovery Implementation Plans, known as TRIPs, support a whole team in becoming more recovery focused, but should not be seen as a management device.
A TRIP aims to empower teams to translate recovery ideas into practice and to utilise the skills and resources of everyone at the front line, both those providing and those using services, to develop innovative ways of promoting recovery and recovery environments.
6. The Team Recovery Implementation Plan: A Framework for Creating Recovery-Focused Services
Julie Repper and Rachel Perkins
INTRODUCTION
Creating more recovery-focused services requires a change in culture and practice at every level of the organisation (Shepherd et al., 2010). In modern mental health services, the basic building block is the multidisciplinary team, whether in a hospital ward or in the community.
Supporting recovery through working with the whole team is at the centre of the processes of organisational change and a necessary complement to changing the attitudes and behaviour of front-line staff (Whiteley et al., 2009).
The ‘Team Recovery Implementation Plan’ (TRIP) was initially developed by Julie Repper and her colleagues in Nottingham and is a tried and tested instrument designed to assist with this goal. This paper describes the instrument and its practical use in a variety of settings.
Successfully embedding recovery ideas and practice into the day-to-day work of individual teams requires two parallel processes:
- Empowering teams (their staff and people using services) to translate abstract ideas about recovery into practice.
- Utilising the skills and resources of everyone at the front line (staff and people using services) to develop innovative ways of promoting recovery and recovery environments.
The creativity of front line staff can often be stifled by competing demands and directions coming from the top which are not aligned with recovery priorities. Similarly, the skills of people using the services are often underused and undervalued. They are seldom asked what they want staff to do or how they want services to support them, thus excluding them from having a meaningful influence on service design. And they are often not recognised as having a direct role in service delivery.
We are missing a trick here. By bringing together all the creativity and skills of staff and people using services, in both the design and delivery of innovative, recovery-focused services, we double our assets and make ‘coproduction’ a reality at a grass-roots level.
What is co-production?
“Co-production … promotes equal partnership between service workers and those intended to benefit from their services – pooling different kinds of knowledge and skill, and working together… designing and delivering public services in an equal and reciprocal relationship between professionals, people using services, their families and their neighbours.” (New Economics Foundation, 2011)
But there is no one way of ‘doing’ coproduction. It consists of a set of underpinning principles (Cahn, 2004; Boyle et al., 2010; Nesta, 2012). These are identified below:
- Recognising people as assets: building on all the strengths within the team/service by utilising both the expertise of using/ providing services and the other skills, resources and networks that they can bring.
- Mutuality and reciprocity: breaking down barriers, blurring roles, valuing what everyone brings, and enabling staff and people using services to share responsibility for both design and delivery.
- Extending the resource base by engaging peer, personal and professional networks: to build knowledge, and work together to design, deliver and support change.
- Team/services as catalysts for change rather than the creator of change: enabling people to lead their own recovery journey and empowering them to develop a range of resources in peer networks and communities to support these journeys.
The TRIP is based on these ideas and is designed to provide a framework to assist teams to co-produce services that will enhance the experience of people using them and so better facilitate their recovery.
The Team Recovery Implementation Plan (TRIP)
Initially developed by Julie Repper and her colleagues at Nottinghamshire Healthcare NHS Trust, the TRIP has been refined through use in the full range of adult mental health services. The aim of TRIP is not to provide a formal assessment device but to initiate a process of discussion, reflection, innovation and development within a team. It is not designed to provide comparison between teams, but to enable teams to co-produce, co-deliver and co-review of actions plans in an ongoing process. It is therefore not a management device: it is an heuristic tool to promote collaborative service development.
The instrument (see Appendix)
The TRIP comprises four key elements:
- An overview of all the resources that exist within the team (‘identifying assets’).
- A tool for benchmarking progress in recovery-focused practice.
- A list of the top three priorities for action agreed by everyone involved, together with action plans for future developments.
- A method for systematic review and resetting of goals.
All these elements are ‘co-produced’ by staff and service users working together. The intention of TRIP is to initiate a process to support a recovery-oriented way of working within the team, based on a shared responsibility for reviewing practice, agreeing areas for development and delivering change. Our experience of using TRIP within at least 15 organisations (statutory and voluntary) has taught us that it is the process of using TRIP, rather than TRIP in and of itself, that is most critical.
The process
- An overview of all the resources that exist within the team (‘identifying assets’). All staff will have mental health experience and training that will, hopefully, be useful; but they will also have ‘hidden talents’ – e.g. skills and interests in music, sport, cooking, gardening, languages, etc.; lived experience of trauma; an understanding of their own and others’ mental health problems; contacts with a range of communities and organisations. This process of asset finding and building among people using the service can involve all the available staff and residents for inpatient wards, but for community teams (with far larger numbers) it may be necessary to use representatives of people using the services who can reflect their diverse views. But it is important to identify and to use this total list of assets and resources to help support the recovery of people being looked after by the team.
- A tool for benchmarking progress in recovery-focused practice. The TRIP provides a series of ‘good practice’ statements drawn from Recovery Self Assessment (RSA) – Provider Version (O’Connell et al., 2005) and 10 Key Organisational Challenges (SCMH, 2010). These tools invite staff and people using services to consider what the team has already achieved in each area and what remains to be addressed. The benchmarking tool provides a framework for generating these discussions, but it should not limit them. The process involves everyone in discussions about these benchmarking statements and it is useful to rate each on a five point scale to help when deciding upon the importance of each area for future work. Examples of some TRIP benchmarking statements are given in Box 1.
- A list of the top three priorities for action agreed by everyone involved, together with action plans for future developments. Clearly, it is not possible for a team to do everything at once – a maximum of around three priorities appears to be realistic. These do not have to be the ‘worst’ areas: quick wins have an important role both in demonstrating achievement and cementing the co-production process. It can also be helpful to think about the twin dimensions of impact and ease of implementation and strike a balance between the two. At least one member of staff and one person using the service should then share responsibility for their implementation. The targets for action must be specific, measurable, achievable, realistic and timely (SMART); identifying what can be achieved by when and how progress will be measured.
- A method for systematic review and resetting of goals. Finally, the team needs to establish forums for reviewing progress, providing support and problem-solving, and holding the joint leads accountable for their actions. Part of an existing meeting like a ward community meeting or a team business meeting can be designated to deliver this function as long as it routinely includes people using the service. Alternatively a new, specific meeting can be created. An annual review beginning again with reviewing assets and benchmarking can then be undertaken to complete the cycle. This gives an opportunity to celebrate success, review priorities and agree new action plans.
Making co-production work
Too often nowadays, those working in and using front-line mental health services experience decisions being foisted on them from on high and there is a risk that organisation-wide enthusiasm for recovery-focused transformation of services may result in yet another set of top-down prescriptions that only serve to reinforce the feelings of disempowerment among both staff and people using services. For co-production to be really effective it is therefore essential that staff at all levels, together with the people using the service, are involved in the process on an equal footing. There must be an opportunity for everyone to discuss their different perspectives about what the team is doing and arrive at a consensus about the current situation and possible directions for development.
Our experience suggests that staff often feel uncomfortable about having open, equal discussions. Too often they feel they must not ‘wash their dirty linen in public’, and can be defensive when people using services do not appear to understand the constraints and demands under which they have to operate. Staff also sometimes assume that it is their job to sort everything out and fear that these open discussions will lead to demands that they cannot meet. This may stem from traditional approaches to user involvement which have asked people using services what they want with little honest information about the external imperatives and constraints that exist (e.g. externally imposed targets and regulations).
By contrast, the TRIP allows staff and people using the service to come together in a different way: to identify progress, to understand each other’s perspectives and constraints, to seek solutions together, and to share responsibility for implementing actions. This is a different way of working together: it is not ‘us’ involving ‘them’, it is asking how can we work together. These discussions are often helped by the presence of an external facilitator – either from another team, a local manager, or an external expert – to promote dialogue and mutual understanding. They should not be seen as a one-off exercise.
Whole team recovery away-days can be a productive way of co-producing a team plan. We have successfully run recovery awaydays, which include people using services, in a wide range of services: from wards in special hospitals and forensic services, through acute wards, rehabilitation services, early intervention and crisis services and community teams. As indicated earlier, for inpatient wards these can involve all staff and residents; for community teams it may be necessary to use representatives of people using the services who can reflect the diverse views of people using the team’s services. In some teams, people have been asked to give individual responses to the benchmarks, these can then be collated to help prioritise areas for action; others have used community meetings or team business meetings (with people using the service present) as part of the benchmarking process. Whichever method is used, it is important that people come together to agree priority actions and develop implementation plans.
The process of co-production continues through development and implementation of action plans: the joint leads need to agree who will do what by when and what other expertise (available within, or to, the team) they will draw upon. Responsibility for implementation should then not rest with the staff lead alone, but be shared with a service user lead. Their roles may be different, based on their skills and resources, but they are equally important.
It is important that the development of recovery-focused practice is a live part of the day-to-day work of the team. This is best achieved by a regular forum at which the joint leads report progress and seek the advice and assistance of their colleagues and their networks/contacts. For example, community and team meetings have been used to discuss one priority/action plan per week on a rolling programme.
Box 1: Examples of TRIP benchmarking statements
- We help people build and/or keep existing roles, relationships and connections with neighbourhoods and communities of their choice.
- We encourage people to make their own choices and decisions and support them even if we do not agree with them.
- We develop care/support plans and write notes in collaboration with service users focusing on their personal recovery plans and clearly stating plans for meeting their recovery goals.
- We work with service users to understand their perspective on ‘risk’, negotiate an agreed safety plan and share responsibility for safety (e.g. what the person can do, what staff can do to help).
- We involve significant others in care planning if so desired and use their expertise and insights (e.g. family and friends, peer support workers, advocates, other service providers).
- We provide examples of real success stories, life story books, DVDs, posters, for people to see what is possible and to inspire their hope.
- We offer everyone in our service access to recovery education where ideas about recovery and personal plans can be developed with others including peers who have moved on.
- We support the wellbeing of staff (e.g. wellbeing plans, supervision and appraisal including personal reflections and wellbeing).
Examples of the TRIP in Action
The priorities and action plans of teams have included a wide range of targets:
- Developing personal recovery goals as part of care plans and/or introducing Wellness Recovery Action Plans / personal recovery plans.
- Reviewing team / ward policies, e.g. risk assessment and management.
- Including people using services on staff interview panels.
- Agreeing on shared entries in notes and people having copies of their own session notes. People writing their own summaries and reports for review meetings.
- Improving the ward/team environment, including positive images and hopeful messages about the possibilities of life with a mental health problem, for example making a ‘Hope and recovery – what it means to me’ pin board.
- Developing a team/ward recovery library, including anthologies of recovery stories.
- Creating information packs (that include recovery stories and ‘things I know now that I wish I had known then’ tips).
- Co-producing directories of resources, sometimes with ‘trip advisor’ style ratings.
- Introducing carer recovery and wellbeing packs.
Box 2: Changes brought about through using the TRIP
At Nottinghamshire Healthcare NHS Trust, B2 acute admission ward in Bassetlaw began to use TRIP in 2008. By 2012, the average benchmarking rating had increased from 1.7 to 3.8. Over the four years of their use, action plans had resulted in many important changes including:
- The development of a self-help library and a visiting ‘living library’ of people (instead of books) who could recount their personal experience of recovery.
- Implementation of personal recovery plans for all.
- The local MIND group running a social group on the ward.
- Co-production of a carers’ leaflet and introducing a separate TRIP action plan with families and friends.
- A ‘Hope board’ of inspiring messages from people using the service.
- People using services and staff who took on joint lead roles were provided with a tailored programme of supervision, training and development.
- Introduction of protected time for staff to ensure more contact with people using the service.
- Increasing peer input on the ward, including the introduction of a Peer Support Worker.
- Introducing an evaluation of ‘levels of coercion’ using the scale developed by Szmuckler & Appelbaum (2008).
- Creating links with community resources and facilities (e.g. open days). Inviting external organisations and agencies to run events.
- Involving others within the mental health service to provide seminars and activities, for example, spirituality and mental health discussions for staff and service users.
- Developing buddy/mentoring systems.
- Introducing peer support workers and volunteers. Facilitating peer networks.
- Co-producing and co-delivering ‘safe dating’ and other courses in conjunction with recovery colleges.
- Celebrating moving on and ‘graduation’ from the team or ward with parties, good luck cards etc.
- Inviting former service users back to share their experience of the benefits and challenges of moving on.
Some practical examples of using the TRIP are shown in Box 2.
Nottinghamshire Healthcare Trust has used the TRIP as a means of enabling all clinical teams to work with the people using their services to identify their own, recovery focused priorities and to develop their own ways of addressing them. All teams are included in the transformation of the organisation and they each now annually benchmark their practice against the TRIP statements, progressively working towards their own recovery priorities. In this way the process can drive practice throughout the whole organisation.
While it is neither helpful nor accurate to compare teams in terms of the scores they award themselves, it has been helpful to aggregate data collected from teams across the Trust to identify the recovery focused practices that are considered to be most and least well developed. For example, ‘supporting family and friends’ seemed well developed; while ‘collaborative note writing’ was not. This exercise also identified recruiting peer workers as the most powerful innovation in driving change within teams (see Repper, 2013).
Central and North West London Foundation Trust have extended the use of TRIP beyond individual teams by using it as the basis for a recovery quality target (CQUIN). Teams were required to complete a TRIP and identify three team priorities which were then collated across service lines and progress monitored by commissioners. This moved away from the usual uniform target expected across all services, towards an individually tailored target developed by front-line staff and service users thus ensuring local relevance and ownership within an overarching, recovery-focused framework.
Box 3: Using the TRIP in West London
At West London Mental Health NHS Trust, the Aurora Ward (a female forensic admission ward) began to use TRIP in 2011. Their initial action plan, supplemented by a range of other initiatives deriving from their weekly progress reviews in community meetings between 2011 and 2012, included:
- The collection of recovery stories,
- The co-production of ‘ward house rules’,
- Communal meals,
- The marking of beginnings and endings: welcome meetings and parties when someone was moving on,
- Recovery sessions,
- Ward round self-reporting.
The impact of these, and the process of joint working between staff and residents that it promoted, improved the experience of the ward for everyone. Between 2011 and 2012:
- Incidents of self-injury fell from 39 to 8,
- Hours spent in seclusion fell from 987 to 483,
- The number of residents who moved on increased from 3 to 14,
- Staff sickness absence decreased from 10.4 To 4.66,
- Physical assaults of staff by patients decreased from 34 to 27.
Conclusion
Recovery is founded on the narratives of lived experience and these frequently emphasise the importance – for good or ill – of relationships at the front-line. Indeed, the need to change the nature of day-to-day interactions and relationships is the first of the ImROC programme’s 10 Key Organisational Challenges. But such changes cannot be achieved by training alone – they require local ownership, co-production, the involvement of staff and line managers, and a culture of innovation that can harness expertise and creativity across the organisation in order to create an environment in which all can grow and flourish. As Patricia Deegan noted nearly 20 years ago, “We are learning that the environment around people must change if we are to be expected to grow into the fullness of the person who, like a small seed, is waiting to emerge from within each of us … How do we create hope filled, humanised environments and relationships in which people can grow?“ (Deegan, 1996).
But services cannot make people recover. Neither can service directors make the work of their staff recovery-focused. What they can do is to nurture the wealth of knowledge, resourcefulness and ingenuity that exists among front-line staff and people using services and empower them to co-create their own solutions. Recovery is about recognising and building on these strengths and possibilities and the creation of recoveryfocused services can only be achieved by valuing the assets and ingenuity of all, whatever their formal ‘position’ in service hierarchies. The TRIP provides a framework that capitalises on the resources of people using services and the staff they see on a day-to-day basis in order to co-produce the fertile environment in which both can grow.
The TRIP is most effective when it is used in the context of an organisation that is committed to creating a recovery-focused culture. There needs to be an overarching recovery strategy, supported by training and awareness-raising for staff, people using services and those close to them. Within this context, the TRIP becomes the way in which individual teams can make recovery a reality at the front-line. However, it can only be one element in the strategy for organisational change.
The ‘Team Recovery Implementation Plan’ is reproduced in the Appendix and can be downloaded from imroc.org/resources.
References
Boyle, D., Coote, A., Sherwood, C. & Slay, J. (2010) Right Here, Right Now.Taking coproduction into the mainstream. London: NEF/ Nesta.
Cahn, E.S. (2004) No More Throw-Away People: The co-production imperative. Washington DC: Essential Books.
Deegan, P. E. (1996) Recovery and the Conspiracy of Hope. Paper presented at The Sixth Annual Mental Health Services Conference of Australia and New Zealand, Brisbane, Australia.
Nesta (2012) Working towards People Powered Health. Insights from Practitioners. London: Nesta.
New Economics Foundation (2011) In This Together. Building knowledge about coproduction. London: NEF.
O’Connell, M., Tondora, J., Croog, G., Evans, A. & Davidson, L. (2005) From rhetoric to routine: assessing perceptions of recoveryoriented practices in a state mental health and addiction system. Psychiatric Rehabilitation Journal, 28, pp 378-86.
Repper, J. (2013) Peer Support Workers: Theory and Practice. ImROC Briefing paper 5. London: Centre for Mental Health.
Shepherd, G., Boardman, J. & Burns, M. (2010) Implementing Recovery. A methodology for organisational change. London: Sainsbury Centre for Mental Health.
Szmukler, G. & Applebaum, P. (2008) Treatment pressures, leverage, coercion and compulsion in mental health care. Journal of Mental Health, 17, pp 233-44.
Whitley, R., Gingerich, S., Lutz, W. & Mueser, K. (2009) Implementing the illness management and recovery program in community mental health settings: facilitators and barriers. Psychiatric Services, 60, pp 202- 209.
Acknowledgements
Advances in recovery-focused practice arise from collaborative partnerships between individuals and organisations. The ImROC briefing papers draw upon this work. Each paper is written by those members of the project team best placed lead on the topic, together with contributions from others.
In this case, we particularly wish to acknowledge the contribution of those whose work on the co-production of care using instruments like the Team Recovery Implementation Plan (TRIP) has inspired and informed the field. Thanks for the support of the many clinical teams who have tried, tested and developed the tool in Nottinghamshire Health NHS Trust, and particularly the leadership of Beverley Johnson and Simon Barnitt.
Appendix
The Team Recovery Implementation Plan
You can download an editable word version of this plan from imroc.org/media/publications.
The Team Recovery Implementation Plan
This briefing paper has been produced for the Implementing Recovery through Organisational Change programme, a joint initiative from the Centre for Mental Health and the NHS Confederation’s Mental Health Network.
The pilot phase of ImROC ran from 2011-12 and was supported by the Department of Health, together with contributions from the participating services. The continuing work of ImROC is endorsed by the Department of Health and managed and supported by the Centre for Mental Health and Mental Health Network.
For more information on the current work of ImROC, please visit imroc.org.
ImROC, c/o Mental Health Network, NHS Confederation, 50 Broadway, London, SW1H 0DB
Tel: 020 7799 6666
imroc@nhsconfed.org
imroc.org
An estimated 1.5 million people in the UK care for or support a relative or friend who has a mental health problem. Yet it can be difficult to know how best to do this. And many carers feel unsupported by mental health services.
The guide sets out practical steps to help people provide support for their friend or family member to be as independent as possible and to do the things that matter to them: to build a better life with or without mental illness. It acknowledges that this can be difficult for family and friends and calls on mental health services to do more to help them in this demanding role.
4. Recovery: A Carer’s Perspective
Karen Manchin and Julie Repper
INTRODUCTION
An estimated 1.5 million people in the UK care for or support a relative or friend who experiences mental health problems. We all want to know what it means for the person we care for and for ourselves. We all know the importance of trying to understand what is happening to them, listening to their accounts of what it feels like, providing practical and emotional support in a manner that they find acceptable and walking alongside them – ‘being there’ and believing in them. Yet it can be difficult to know how best to do this.
The concept of Recovery offers a framework which is relevant and constructive for both the person who experiences distress and their family and friends. Since it is not prescriptive, it can also facilitate the development of mutually supportive relationships.
This briefing paper examines what Recovery means for the families and friends of people with mental health conditions. It suggests ways in which these informal carers can support Recovery and looks at how mental health services can give the best possible help to do this. It also provides information about key resources, including the Triangle of Care and a Wellbeing Recovery Plan for families and friends.
THE MEANING OF ‘RECOVERY’
The value of ‘recovery’
There has been some debate about the appropriateness of the word ‘recovery’ in the context of mental health. It is generally used to describe ‘recovering from’ an illness or injury through restoration of function, the eradication of symptoms and returning to a previous life and routine. People who have experience of mental health problems have challenged this notion of recovery. They argue that their emotional and cognitive challenges do not need to be removed in order for them to ‘recover’ meaningful lives. They argue that it is possible to live well with – and without – these challenges, emphasising the importance of hope and the belief that they can contribute and take control of their ‘symptoms’ if they have access to the same opportunities as other citizens. Indeed, they have demonstrated that they can recover different and even better lives than they had envisaged before their mental health problems occurred.
“Recovery is the process of developing a new sense of self, meaning and purpose in life – the journey of the individual and those close to them in rebuilding a satisfying, hopeful and contributing life with a diagnosis of mental health problems.” (Deegan, 1989)
This concept of ‘recovery’ in mental health was a revolutionary idea at a time when people, including most mental health practitioners, believed there was no such thing as recovery from serious mental illnesses like schizophrenia. It was thought that to have hope was unrealistic and that people with mental health problems did not have the capacity to regain control over their lives and make the most of their opportunities.
Carers’ concerns about recovery
“It was something like perpetual bereavement … My daughter, the person who I used to know so intimately, and who I loved and wanted to rescue more desperately than I’d ever wanted anything, was beyond my reach… My girl had become a stranger to me and I to her.” (Varley, 2007)
The Recovery approach has caused considerable concern among many carers, service users and professionals. Some people have expressed concern that the term ‘Recovery’ is being misunderstood within statutory health services and is being used as an excuse to neglect people who reject support, or a reason for discharging those who say that they want to live independently. But this is not what the Recovery approach should be about. While independent living is an important aspiration for many, recovery-focused services do not abandon people when they make progress and nor do they ignore the needs and concerns of carers. Recovery should not be seen as a way of ‘selling’ service cuts. It is about enabling people to manage their own lives, not reducing support or raising access thresholds.
Family members may have supported someone for many years, through several periods of crisis, perhaps including inpatient admissions and involuntary treatment. We may have requested support on many occasions without result, expressed our views without being heard, and not been given essential information (as have sometimes been this author’s experiences). With such experiences, it is difficult not to lower our expectations. When services start to talk about helping our son, daughter or parent towards getting back to work or coming off medication, our experience warns against it. We may find ourselves saying, ‘He’ll never go back to work’ or ‘She’ll always need medication’.
If someone has been stable on medication after a long period of distress, it can feel very threatening if ‘recovery’ is assumed to mean a life without medication. Similarly, employment may feel like an impossible target and a frightening change that family and friends fear might bring the risk of further relapse. These are completely understandable responses. Carers need to feel that professionals are taking them seriously and will work through the possibilities in an honest and respectful discussion. An understanding of recovery should help carers, service users and professionals to have such conversations.
Recovery does not assume that people all reach a stage when they do not need support. All of us find new endeavours much easier with the support of families, friends and experts – including those who have personal experience of the same journey or those with professional expertise. Thus, pursuing recovery should not equate with discharge, neglect or isolation and, far from excluding family and friends, it should be actively drawing on their support.
The term ‘Recovery’ can also appear to take little account of the individual in relation to their culture and the nature of their close personal relationships. These are especially important when, for example, experiences of racism, sexism or homophobia are factors in distress. These may be beyond the scope of health services or family carers to fix, but as Kalathil (Mind, 2008) asks, “If recovery is the process of moving on to more empowering and meaningful ways of being, what does that mean to a person whose everyday experiences of living includes racism and discrimination?”.
If recovery may seem like a far-fetched idea for some of the people we support, we may have to change our ideas about what is possible, and when. We are used to seeing people with physical impairments encouraged and assisted to participate in society, but nobody would expect a blind person to wait until their sight is restored before they are ‘included’. Why should this be any different for someone with mental health problems? Why should we have to wait for the problem to go away before considering goals and opportunities? Not only will people be less disabled by their challenges if they are doing something they value, but while we are waiting for them to ‘get better’ they are losing everything they value in life – work, friends, independence, a home. Shouldn’t everyone be offered hope, choice and opportunities from their first contact with services?
A ROLE FOR FAMILY AND FRIENDS IN RECOVERY
“I would not be here if it were not for my family. I can always talk to my mum and she is great when I am really low. My Dad can sort things out in a crisis but he gets impatient with the way I live my life. It is my brother who really understands what I need when I’m feeling very bad.” (Gow, 2010)
Some people prefer to describe recovery as a journey of discovery because it is about growth and exploration, developing greater understandings, finding solutions about who helps and who does not, how best to use personal strengths and when to call on others. If we define recovery as a journey of self-discovery, ‘fellow travellers’ are then also welcome and ‘guides’ can be useful. Carers, supporters and staff are also on a journey of their own alongside the person experiencing distress.
“Who are we? What are we? Why are we here? These are not simply moral issues, they are also political. Recovery came out of the civil rights movement of the 1960s and is about a vision of a life lived to the full – with passion, humour and style.” (Urey, R., quoted in Mind, 2008)
Everyone’s story of recovery is unique, just as each experience of distress is unique. Mental health problems may come on suddenly, or they may take years to develop. We may each identify different events that set off our distress and different times when we can pinpoint that something felt different. We may also have very different explanations about why it happened. Everyone can recover a more meaningful life, but this will always mean different things to different people. Nevertheless, ‘recovery’ is for everyone. We should therefore always be ambitious about it, filled with hope.
Family members and long-standing friends have a unique role to play in recovery because we know the person well, often before their distress. We can therefore serve as a reminder that the person is not solely someone with a mental health problem, but someone with talents and abilities, a person with qualities, interests, skills, beliefs and ambitions.
“It has been invaluable to have… my husband with whom I can test ‘reality’. I let him know my perceptions and he gives me feedback. I am then able to consider that my perceptions may not be accurate and I modify my response accordingly if I wish.” (Leete, 1989)
Paid supporters, by contrast, only know the version that they have been told: they have joined the journey in the ‘middle’. Sometimes, that unfamiliarity can be an advantage, it can be reassuring to speak to someone who doesn’t know you. People don’t always want to tell family and friends what’s worrying them, especially if it links to feeling ashamed, of being weak and helpless. And while a minority of families and relationships are abusive or cannot provide support, that is not the case for most of us, who desperately want to know what we can do to help.
“We assumed blame… We had let her down. An overwhelming sense of guilt swept over us. We kept coming back to the ‘Why us?’ question. The present felt grim and we feared for the future… Initially our personal feelings had the quality of an emotional roller-coaster, but as despair set in we found ourselves becoming exhausted and without hope. We all began to entertain the possibility of improvement… often tiny incremental improvements have combined to achieve remarkable progress. She now lives in a supported home, remains well-integrated with her family and leads a full and happy life.” (Shiers, 2007)
We all want the best for our loved one. We are deeply and personally affected by their distress and often carry a burden of guilt, worrying that we caused the problem and that we should be able to help more. But we can benefit from our caring role. We feel good because we are in a position to support the person we love. We are valued and we feel privileged because someone confides in us, pleased to have someone around to talk with, and aware that we are developing new skills. Family and friends have a huge contribution to make and a lot to gain. This is the essence of mutual support.
“I have now learned to walk alongside my sister, instead of trying to tell her what to do or to push her in the direction I think she should go in. For years, I did try to push and experienced feelings of frustration, annoyance and, at times, total despair for her chosen path or inability to see things from my point of view. At times of her despair, I felt it too and at her lowest ebb, I was with her too… for my sister, my door remains open when it needs to be opened by her, and that is the most important thing.” (Action on Depression website)
Tim
“Tim’s illness began just over seven years ago, accelerating into crisis very quickly, at which point he was sectioned into hospital and given a diagnosis of schizophrenia. The impact of reaching that point in a few weeks after terrible worry, signing committal papers, psychiatric nurses trying and failing to take Tim forcibly from home, the Police eventually succeeding, the true terror and grief for the ‘loss’ of our son, and the dread of what the future would hold, were utterly devastating…
Over the last seven years we have learned patience. There are no quick fixes to recovery… we have spent many, many hours listening – often enough long into the night. I know that me being available to Tim at any time has been of immeasurable benefit… In the early days, I could only be a sympathetic and encouraging ear as Tim battled with the misery of his situation – his despair, depression, anxiety, anger.
He began to look around himself with new eyes and became deeply interested in understanding all he could of the human mind, and who better to teach me than Tim? He really has mined his own experiences for meaning and understanding, for growth and release… This exploration over the past years has formed the backbone of Tim’s recovery.
“On very weary days, there is always the temptation to hide behind the protective shield of illness where little is expected of the sufferer… Our experience of the mental health world is that expectation falls quickly into the hole of ‘we mustn’t set him up to fail’, which has the potential to keep everyone ‘safely’ in the world of the lowest common denominator.
We have worked with everything Tim is – in character, personality, potential, ability and inclination at every stage. In the past five years, Tim has tried a number of jobs, lived independently, travelled abroad, learned to drive his own car, taken up a wide variety of study, has been deeply involved in music, enjoys hill walking and badminton. There have been occasions where things haven’t ‘worked out’, but that’s fine, and we have never sought to wrap Tim up in cotton wool.
Today, as we look at Tim, we know he is all that he was meant to be – that the promise in the child is here in the man… He has at his command all the tools and strategies he has forged from his difficult journey, and the knowledge and mastery of himself.” (Gould, 2005)
Reproduced with permission from the Scottish Recovery Network.
HOW FRIENDS AND FAMILY CAN SUPPORT RECOVERY
“You have the wondrously terrifying task of becoming who you are called to be. Your life and dreams may have been shattered – but from such ruins you can build a new life full of value and purpose.” (Deegan, 1993)
There are many ways in which family and friends can help. We may be the first to identify unusual behaviours and beliefs and recognise the situations that seem to cause upsets (‘triggers’). We can learn over time what seems to help. We can provide early support and reassurance, making suggestions to alleviate further distress and offering practical support – cooking meals, doing washing, going on walks. We can also avert further difficulties, like sorting out housing to prevent eviction, explaining the situation to debt collectors to prevent destitution, etc. The importance of this protection of basic needs cannot be underestimated. But to support someone in their recovery, we also need to learn new skills and approaches to help them to build a life for themselves alongside their family and friends.
We suggest four areas where new skills might help family and friends build a new supportive relationship:
- recovery planning,
- building on strengths,
- developing helpful relationships,
- handing back control.
Recovery planning
Everyone makes plans in their lives to some extent. But until we understand the unique nature of each person’s recovery journey, we don’t know where to start to help someone else plan for the future. At the start, we have no idea how long it will last, what the options are or whether things will get better.
Despite all these unknowns, family and friends have a central role in helping people to hang on to roles and relationships that are important to them, helping them to understand what is happening to them and always working towards their personal goals – aims that are important to them, rather than to us. We can help them to keep well, prepare for potential challenges and remember who they are. We can encourage and support the person to develop their own Recovery Plan and then help them share it with those who can offer support.
Building on strengths
When a person is distressed, it is all too easy to begin thinking negatively. They may hear voices reinforcing this message. Or they may be facing the all too real results of overspending or self-harm. They may feel that the world is against them, that they are complete failures and everything that can go wrong will go wrong, so what’s the point of trying?
Having someone who can remind them of the positives can make a huge difference. This is not to deny the challenges, to pretend they don’t exist, or to insist that it is within the individual’s power to remain positive in the face of very real difficulties. But when people fall, it is important that their family and friends don’t fall with them. We have an important role in pointing out that they tried and what they have achieved. We can remind them of little things they have forgotten. It is very important that we hold on to our hope when they find it impossible to see the light at the end of the tunnel. It is our constant and enduring belief that things will get better that can help them through the darkness.
Developing helpful relationships
When we are providing a substantial amount of support, it is all too easy to get stuck in the experience of distress, forgetting our own needs and centering everything on the distressed person. This can create cycles of negative behaviour with all of us identifying the problems so that these become self-fulfilling as all the positive opportunities are removed.
The whole family can benefit from looking at their roles and relationships, including what strengths and skills each person brings and what people find most and least helpful.
Carers often talk about the difficulty of treading a tightrope between encouraging someone to do more and allowing them to rest and be supported. This isn’t easy – but it is helpful for everyone to talk about what helps them, what they find difficult in their relationships, and what options are available for coping more effectively.
Handing back control
Family and friends can easily get trapped into a position of doing more and more. We may gradually take responsibility for major tasks such as controlling money or paying the rent. Other, smaller, daily tasks such as washing and cleaning may slip into our domain of responsibility during periods of distress and these habits are difficult to break. We sometimes even find that we don’t trust a person to take their own medication and we start to take over control of that too.
Once these patterns build up, it can be hard to let go. It may feel ‘risky’, but unless we are prepared to hand back control and let the person manage their own life again, they cannot grow. Obviously, we must not ignore safety issues, but decisions about how to move forwards safely need to be shared between the person, their family and friends, and their professional team, with everyone supporting the individual to move on safely towards their chosen goals.
“That a person recovers means that the other people in his or her surroundings also have to recover; the unequal dependence relationship that was established between the person and his or her social network during times of deep distress must change. The helper must step down from this one-sided role and be prepared, not only to disengage, but also to perhaps now be the recipient of the person’s concern and advice.” (Topor et al., 2006)
HOW CAN SERVICES SUPPORT FAMILIES?
To fulfil these important and challenging roles, family and friends need effective support from mental health services. This support can come in a number of forms and will, of course, need to be tailored to every situation. Key actions for services include:
- identifying carers,
- tackling stigma and discrimination,
- understanding the impact of caring,
- delivering family interventions,
- developing carer peer support,
- offering education not therapy.
Identifying carers
Government guidance defines carers as people who “provide unpaid support to family or friends who couldn’t manage without this help, whether they’re caring for a relative, partner or friend who is ill, frail, disabled or has mental health or substance misuse problems” (Department of Health, 2012).
Identifying carers is not, however, a simple task. Many people do not consider themselves to be carers when they are supporting someone they care about: they are just friends, mothers, brothers, neighbours. They provide care as part of their natural social roles. If people don’t identify themselves as carers, they will have difficulty accessing Carers Centres, Carers Allowance, Carers Grants and Carers respite.
Many family members describe walking past signs and posters using the word ‘carer’ thinking they refer to paid care workers rather than informal, unpaid carers such as partners, friends or parents. Carers UK research (2006) suggests that 65% of people with a caring responsibility did not identify themselves as a carer in the first year of caring and for 32% it took over five years to be recognised. Carers from Black and Minority Ethnic communities also provide proportionately more care than White British carers (Carers UK, 2011).
It is likely that carers for people with hidden illnesses such as mental distress aren’t so easily recognised as those looking after elderly relatives. Even some carers’ organisations might prefer to refer mental health carers to specialist agencies. Young carers may be particularly challenging to identify and less likely to seek help.
The updated national carers strategy acknowledges the specific difficulty of identification for carers supporting someone through distress: “The onset of mental health problems and the process of seeking help can be particularly traumatic for families. Those supporting people with mental health, personality disorder or substance misuse problems can be wary of seeking help outside the family because of the stigma, discrimination and bullying that are still too often associated with these conditions.” (Department of Health, 2010)
It is also worth noting that many people can be both a service user and a carer. While NHS Trusts may gather statistics for the number of carers (including young carers) who support their service users, they are not required to collect data on the number of service users who also have caring responsibilities. Once people identify as carers, they may be able to access support as a carer, including carers respite and breaks. Providers should therefore routinely ask service users about their caring responsibilities and signpost them to appropriate support.
Tackling stigma and discrimination
Families who stand by someone through distress risk being affected by discrimination through association. This is now recognised in the Equality Act (2010). Carers Direct (2012) highlights the specific stigma experienced by carers, especially in the workplace, where colleagues might make assumptions about why they have to take time off. Carers may also feel unable to take time off work because they don’t want to mention the reason.
“They never knew at work. If I told them, I’d have to tell them about his problems. And he never wanted to do that because he hoped to get through it and didn’t want people to know. I didn’t want to break that confidentiality.” (Anonymous carer in Machin, 2006)
Time to Change (www.time-to-change.org. uk), the anti-stigma campaign, provides materials and a message that appeals to a wide audience. This may be an effective way to help services to engage with hidden carers.
Understanding the impact of caring
The caring role can affect carers’ own health and wellbeing. A recent national survey found that 87% of carers thought caring had a negative impact on their own mental health and 91% said they were affected by anxiety or stress (Carers UK, 2012). Indeed, forthcoming Royal College of GPs commissioning guidance suggests that all carers should be screened for depression (2013, in press).
However, carers may not feel able to mention their own distress. They may feel they have to continue to cope and, in comparison to the person they support, they may be seen as relatively ‘well’ or able. Young people in particular may be torn between wanting to support a parent and wishing to join in the everyday activities of their peers.
Noble (2008) has shown that carers of people who experience a stroke are three times more likely than average to experience symptoms of PTSD (post traumatic stress disorder). People who support someone through crises of psychosis or self-harm may be similarly traumatised by what they have experienced, but no-one usually thinks to ask. Staff on wards who witness suicide attempts will usually have de-briefing sessions and be offered support, but this is seldom offered to family and friends, although they may have witnessed far more and have a much greater emotional attachment.
Family members and friends of people who experience mental health problems therefore need support to think about their own recovery, not just in terms of practical help to get on with the business of living, but also emotional help. For many of us there is a huge sense of loss when we think back to the people we used to be and our hopes and dreams, both for ourselves and the people we support. Unless we can come to terms with this, it is hard for us to celebrate subsequent achievements and development.
For professionals, we can be a frustrating group because we are so focused on the support of our loved ones. It is all too easy for us to assume that if only the right support was available then everything would be fine and we are quick to blame services when our loved one does not recover quickly. Too often we believe that if we could rely on someone else to provide that support, then we would not be anxious or distressed and we would have the freedom to take a break and to share our worries.
Delivering family interventions
Although there is very little research into the experience of caring for a person with mental health problems, there is extensive research that demonstrates the effectiveness of psychosocial interventions for family members. Such interventions are based on the theory of Expressed Emotion (EE) which developed out of studies of the impact of family members on people with schizophrenia (Brown et al., 1962, 1972). The ‘EE’ interview provides a measure of the ‘amount’ of negative emotion displayed, typically in the family setting, usually by a family or care takers and measured on indicators of hostility, emotional over-involvement and critical comments.
Research has shown that EE provides a relatively robust measure of relatives’ emotional attitudes towards people with numerous psychiatric conditions (psychosis, anxiety, depression, borderline personality disorder) and physical illnesses (Wearden et al., 2000). High levels of negative emotions are strongly associated with a high risk of relapse.
Family interventions are generally delivered by trained specialists, either with individual families or in larger family groups. They focus on improving communication skills, reducing high ‘EE’ (mainly criticism and hostility) through enhanced problem-solving, thereby improving relationships within the family. Studies in several countries have found that they are effective in reducing the risk of relapse and readmission (Pharoah, 2006).
Developing carer peer support
Carers can become isolated and feel alone in their experiences. Many find that it helps to meet with other carers in groups, receiving and giving support to their peers. This may be particularly effective for carers in marginalised groups including families of people in secure services (Canning et al., 2009).
The last few years have seen the development of mutual support in mental health services with the employment of Peer Support Workers (Repper & Watson, 2012; Repper & Carter, 2011; Bassett, Faulkner et al., 2010). These new workers have training in skills such as active listening, recovery planning and story sharing. The focus of their work is on strengths and recovery, rather than problems and symptoms. But their unique gift is that they have been there: they have had a similar experience and are willing to share it. They can pass on a message of hope that mental distress can be survived and that many people who have been through it have achieved valuable, satisfying and contributing lives beyond illness.
Nottinghamshire Healthcare NHS Trust has extended the idea of peer support to include ‘Carer Peer Support Workers’ employed to provide information, signposting and practical support for family members based on their own experiences. Although only two posts have been in place for 12 months, carers who have received peer support are unanimously positive about their experience. They report that peer support is qualitatively different from professional support, giving them hope and belief in their ability to cope because of the roles modelled by the carer peers.
“I bring my own experience as a carer to the work I do with family carers to help them understand what has happened, help them have a better understanding of how the mental healthcare services work and to get them out and about again, encouraging them to take up interests or work and to look after their own health needs. I make sure they know they are entitled to a carers assessment if they haven’t already had one and am a point of contact if they feel the need to talk. We share our stories and look at ways of coping that have helped me, such as changing the language I use with the person I care for.” Judith Machin, Carer Peer Support Worker, Nottinghamshire Healthcare Trust
Offering education not therapy
Carers are usually thrown in at the ‘deep end’ when it comes to caring. They are often not asked if they want to be a carer and not given any training for their new role.
The ImROC project emphasises a move away from a service solely providing therapy, towards educating people, providing them with understanding and skills to manage their own lives and make their own decisions. This is the thinking behind Recovery Colleges (Perkins et al., 2012) where peer trainers work with professionals to co-produce and co-deliver a range of courses for people who use services, their families and friends as well as staff. Courses need to be developed specifically to meet the wishes and needs of family, friends and informal carers so that they all learn together. Courses may need to be delivered outside working hours so as to include working carers.
A number of courses have also been developed specifically for carers by other organisations. These include the Caring with Confidence (2009) course produced as part of the National Carers Strategy, a series of workbooks called ‘Caring for Yourself’ developed by Rethink Mental Illness (2012), a staff training DVD developed by Rethink Mental Illness (2011) and the Meriden training for staff and family members (Fadden & Heelis, 2011).
Meriden Family Programme worked with Rethink Mental Illness to develop a workbook for family and friends. This is built on a wealth of experience and expertise and helps carers to work out ways of coping successfully with the challenges of supporting someone with mental health problems (Fadden et al., 2012).
The Triangle of Care
The ‘Triangle of Care’ (Worthington & Rooney, 2010) aims to be, ‘a therapeutic alliance between service user, staff member and carer that promotes safety, supports recovery and sustains wellbeing.’ It attempts to ensure that NHS staff are aware of carers’ needs including the identification of people who take responsibility for providing support and providing the necessary information, overcoming problems created by confidentiality requirements.
Based on the experiences of many hundreds of carers, the Triangle of Care identifies six elements which create a framework for better collaboration and partnership between staff and carers. Since its launch in 2010, the Triangle of Care has been endorsed by 80% of Mental Health Trusts (by December 2012). Their staff are in the process of implementing the six elements.
The Triangle of Care recognises the important role played by families and friends and makes six suggestions to achieve better collaboration and partnership with carers.
Achieving better collaboration and partnerships with carers
- Identify Carers and the role they play at first contact or as soon as possible thereafter.
- Train staff to be ‘carer aware’ with carer engagement strategies and a clear understanding of carers’ rights in relation to their own assessment and the disclosure of information.
- Ensure that policy and practice protocols re confidentiality and sharing information are in place.
- Create defined post(s) responsible for delivering and sharing good practice in relation to carers.
- Provide carers with an introduction to the service and staff with a relevant range of information across the acute care pathway.
- Provide a range of carer support services along with a self assessment tool.
More information about the Triangle of Care project and ongoing developments can be found here: http://professionals.carers.org/health/articles/triangle-of-care,6802,PR.html.
CARERS’ RECOVERY PLANS
Carers may find it helpful to read and complete the ImROC health and wellbeing plan for family, friends and carers, which guides you through developing your own support plan including:
Your health and wellbeing maintenance plan
This is about identifying the activities and relationships that are important to you, how you might be able to make time for them in your busy life, and things you need to do to keep yourself feeling on top of things.
Your health and wellbeing ‘first-aid kit’
This helps you to think through what you can do to get yourself back on your feet when you feel upset, angry, discouraged or stressed out.
A plan for managing difficulties that arise and things that get to you
What you can do when things happen that knock you off balance, wear you down, upset or anger you… to stop them getting to you too much.
A plan for what to do when everything is getting too much for you
Despite your best efforts, there are likely to be times when difficulties drag on and escalate. All of us sometimes get to the point when we have had enough, feel unable to cope and just want to give up. It is important to think about what you can do to cope at times like this, but this may also be the time to ask for help.
The plan is available from the ImROC website at imroc.org.
CONCLUSION
While recovery may be a unique and personal journey, none of us follow it in isolation. Recovery planning must therefore consider the needs of our family and friends, and our community.
Services need to identify carers and staff need to recognise the immensely valuable and sometimes challenging role that we play – without us, they simply could not cope. They need to acknowledge that we may not naturally come forward for many reasons including stigma and discrimination. Work can then begin to ensure that carers have the information and support that we need to be a ‘fellow traveller’ in the recovery of the person we care for. We must also become experts in our own journeys of recovery.
Useful web sites
There are a number of web sites where you can read about the experience of other relatives and friends:
www.mentalhealthfoundation.org.uk
www.channel4.com/health/microsites/0- 9/4health/mind/pex_managing.html
www.healthcentral.com/ depression/c/5570/17635/dealing
Acknowledgments
Thanks to Ruth Hannan from Carers Trust and Steve McIntosh from Carers UK for their comments about this paper, and to Alan Worthington for his input into the Triangle of Care.
About the authors
Julie Repper is recovery lead at Nottinghamshire Healthcare NHS Trust. She is also associate professor of recovery and social inclusion at the University of Nottingham and service user engagement fellow for East Midlands and chair of the Advisory Group for MHRN Carers in Research group (FACTOR). Julie is also a senior consultant on the ImROC programme and on the Genio funded Advancing Recovery in Ireland project.
Julie draws on her professional and personal experience of mental health problems to work with peers to develop innovative training, research and service developments. She is currently director of the Nottingham Recovery Education Centre and course director for the Peer Support Course at Nottingham University. She has written widely around recovery and leads several related research and service development projects.
Karen Machin works freelance within the mental health field, and has an interest in outcomes, communities and digital media. Based in the North West of England, she has worked universities and trusts, CSIP and Time to Change, in a variety of roles using skills including facilitation, research, events organisation and film making.
In the last 12 months, she has delivered training including peer support worker courses and Caring with Confidence courses.
Her user involvement experience includes setting up local organisations for service users and for carers, and fundraising for specific projects including young carers support, arts exhibitions and the world’s first carers complaints choir. She is one of the founder members of the ROLE network CIC, a social enterprise formed by service users/survivors and carers across the North West.
REFERENCES
Basset, T., Faulkner, A., Repper, J., Stamou, E. (2010) Lived Experience Leading the Way: Peer support in mental health. London: Together.
Brown, G. W., Monck, E. M., Carstairs, G. M., et al. (1962) Influences of family life on the course of schizophrenic illness. British Journal of Preventive and Social Medicine, 16, 55-68.
Brown, G. W., Birley, J. L. & Wing, J. K. (1972) Influence of family life on the course of schizophrenic disorders: a replication. British Journal of Psychiatry, 121, 241 -258.
Canning, A., O’Reilly, S., Wressell, L., Cannon, D., Walker, J. (2009) A survey exploring the provision of carers’ support in medium and high secure services in England and Wales. Journal of Forensic Psychiatry and Psychology, 20(6), Dec 2009, 868-885.
Carers Direct website, Stigma and Discrimination page. Available at: www.nhs.uk/carersdirect/yourself/takingcareofyourself/pages/stigmadiscrimination.aspx [accessed 13 February 2013]
Carers UK (2006) In the Know: the importance of information for carers. London: Carers UK.
Carers UK (2011) Half a million voices: Improving support for BME carers. London: Carers UK.
Carers UK (2012) In Sickness and Health. London: Carers UK.
Caring with Confidence (2009) course materials available online at www.nhs.uk/CarersDirect/carers-learningonline/Pages/resources-for-training-providers.aspx [accessed August 2012]
Action on Depression website, Valerie’s Diary. Available at: www.actionondepression.org/community/valeries-diary [accessed 13 February 2013]
Deegan, P. (1989) A letter to my friend who is giving up. Connecticut Association of Rehabilitation facilities, Cromwell, CT.
Deegan, P. (1993) Recovering our Sense of Value after being Labelled. Journal of Psychosocial Nursing, 31(4), 7-11.
Department of Health (2012) Carers www.dh.gov.uk/health/category/policy-areas/ social-care/carers/ [accessed August 6 2012]
Department of Health (2010) Recognised, valued and supported: next steps for the Carers Strategy. London: Department of Health.
Fadden, G. & Heelis, R. (2011) The Meriden Family Programme: Lessons learned over 10 years. Journal of Mental Health, 20(1), 79-88
Fadden, G., James, C. & Pinfold, V (2012) Caring for Yourself – self-help for families and friends supporting people with mental health problems. Birmingham: Rethink Mental Illness and Meriden Family Programme
Gould, V. (2005) A carer’s perspective on the recovery journey. Available at: www. scottishrecovery.net/Submitted-thoughts-andstories/a-carers-perspective-on-the-recoveryjourney.html [accessed 13 February 2013]
Gow, D. (2010) My Recovery Story. Paper given at Nottinghamshire Healthcare Trust Recovery Conference.
Leete, E. (1989) The treatment of schizophrenia: A patient’s perspective. Hospital and Community Psychiatry, 38, 486- 491.
Machin, K. (2006) Living with mental distress: the family’s experience (DVD)
Mind (2008) Life and times of a supermodel. London: Mind.
Noble, A. & Schenk, T. (2008) Posttraumatic stress disorder in the family and friends of patients who have suffered spontaneous subarachnoid hemorrhage. Journal Of Neurosurgery, 109(6), pp. 1027-33.
Perkins, R., Repper, J., Rinaldi, M. & Brown, H. (2012) Recovery Colleges. London: Centre for Mental Health.
Pharoah, F. M., Rathbone, J., Mari, J. J. & Streiner, D. (2006) Family intervention for schizophrenia. Cochrane Review 2006.
Repper, J. & Carter, T. (2011). Using personal experiences to support others with mental health problems. London: Together.
Repper, J. & Watson, E. (2012) A year of peer support in Nottingham: lessons learned. The Journal of Mental Health Training, Education and Practice, 7(2): 70-78.
Rethink Mental Illness (2012) Caring for yourself. Available at: www.rethink.org/living_with_mental_illness/caring/caring_for_ yourself.html [accessed 13 February 2013]
Royal College of General Practitioners (2013, in press) Commissioning for Carers. London: Royal College of General Practitioners. This guidance will be available at: www.rcgp.org.uk/carers
Shiers, D. (2007) Why us? in Hardcastle, M. et al. Experiences of Mental Health Inpatient Care: Narratives from Service users, carers and professionals. London: Routledge.
Topor, A. et al. (2006) Others: the role of family, friends and professionals in the recovery process, American Journal of Psychiatric Rehabilitation, 9:17-37.
Wearden, A., Tarrier, N., Barrowclough, C., Zaastovny, T. & Armstron Rathill, A. (2000) A Review of Expressed Emotion in Healthcare. Clinical Psychology Review, 20(5), pp. 633- 666.
Varley, J. (2007) Frustrated and angry in Hardcastle, M. et al. Experiences of Mental Health Inpatient Care: Narratives from Service users, carers and professionals. London: Routledge.
Worthington, A., Rooney, P. (2010) Triangle of Care. Available at: www.rcn.org.uk/ development/mental_health_virtual_ward/ triangle_of_care [Accessed 13 February 2013]
Recovery: a carer’s perspective
This briefing paper has been produced for the Implementing Recovery through Organisational Change programme, a joint initiative from the Centre for Mental Health and the NHS Confederation’s Mental Health Network.
The pilot phase of ImROC ran from 2011-12 and was supported by the Department of Health, together with contributions from the participating services. The continuing work of ImROC is endorsed by the Department of Health and managed and supported by the Centre for Mental Health and Mental Health Network.
For more information on the current work of ImROC, please visit imroc.org.
ImROC, c/o Mental Health Network, NHS Confederation, 50 Broadway, London, SW1H 0DB
Tel: 020 7799 6666
imroc@nhsconfed.org
imroc.org
Local councils and Health and Wellbeing Boards can support the commissioning of recovery-oriented services, as well as promoting good mental health and wellbeing in communities. This paper outlines the ways in which Health and Wellbeing Boards can influence commissioning to promote and protect mental wellbeing and support Recovery.
The paper sets out the steps that health care providers, those using or working in mental health services, voluntary groups, commissioners of services, Health and Wellbeing Boards, and those working in Public Health can take to support Recovery
3. Recovery, Public Mental Health and Wellbeing
Jed Boardman and Lynne Friedli
Introduction
Recovery is concerned with living a life beyond illness (Shepherd et al., 2008). While the ideas of recovery and recovery-oriented practice have the potential to transform mental health services, we need to look beyond what is provided by these services and examine the whole range of resources and opportunities that can support quality of life, full citizenship and human rights for people with mental health problems.
Recent developments in public health, notably the emphasis on mental health and wellbeing, can contribute to a greater orientation towards recovery – in local systems and in services, as well as in communities. The public health responsibilities of local councils, as well as the development of Health and Wellbeing Boards, are prompting creative thinking about what supports recovery where people live, as well as the benefits of greater integration between mental health services and public mental health and a more holistic approach to mental and physical health.
This paper outlines how public mental health and the growing ‘wellbeing’ movement can contribute to one of the key challenges for recovery: increasing opportunities for building a life beyond illness (Sainsbury Centre for Mental Health, 2009a), keeping in mind the principles of respect for people’s self determination, choice, control and potential, as well as for support that does not undermine citizenship.
It sets out the ways that health care providers, those using or working in mental health services, voluntary groups, commissioners of services, colleagues in public health and those with a role, or potential role, on Health and Wellbeing Boards, can support recovery through the development of public health and community based approaches. Health and Wellbeing boards have the potential to influence commissioning that promotes and protects mental wellbeing and supports recovery. We conclude by outlining 12 opportunities for these boards to support recovery-oriented commissioning.
Public health and local systems
Developments in public health
The context for commissioning, delivering and using mental health services is changing radically (Joint Commissioning Panel for Mental Health, 2012). As well as a continuing focus on personalised approaches to supporting people with mental health problems, this includes changes in local health and social care systems, giving a much stronger role to primary care and local authorities.
These changes have the potential to support a stronger recovery focus, both within services and within local communities. They also provide opportunities for wider public debate about meeting mental health needs. For mental health services, this should result in a richer awareness of different local resources and opportunities, how these can be drawn on by people involved in the design of their own care and support and how to protect valued community resources, especially in the context of sharp cuts in public spending.
Local government
Responsibility for public health is moving to local government and there is a growing emphasis on ‘public mental health’ or promoting the mental wellbeing of the whole population, as well as an ongoing commitment to reducing inequalities in health.
Equal recognition for both mental and physical health and the importance of mental health to overall health and quality of life is a core theme in a range of Government policy, including:
- Healthy Lives, Healthy People (Public Health White Paper: Department of Health, 2010a)
- No health without mental health (Cross Government Mental Health Outcomes Strategy: HM Government, 2011)
- Mental Health Implementation Framework (HM Government, 2012a).
Health and Wellbeing Boards
Health and Wellbeing Boards (HWBs) are statutory bodies, to be established by local authorities, with a formal wellbeing remit and strategic responsibility for coordinating commissioning across the NHS, social care, children’s and public health. HWBs must include at least one local councillor (elected member), directors of social services, children’s services and public health, representatives of clinical commissioning groups and the local Health Watch. They may also include any other partners considered to have an important influence on health and wellbeing locally.
Some localities have plans for both a formal Health and Wellbeing Board and a wider ‘partnership for wellbeing’ which could include a range of local providers, community and voluntary agencies and representatives of local communities e.g. faith communities. North Yorkshire County Council describes their new arrangements as follows:
“The [health and wellbeing] board will give communities a greater say in the services needed to provide care for local people and to tackle the wider influences on health, such as education, transport, housing, employment and leisure services. The board will have two “doing arms” to drive forward its day to day work. These will be North Yorkshire’s Children’s Trust and North Yorkshire’s Adult Partnership Trust (involving representation from acute hospital trusts, mental health trusts, the voluntary sector and care sector etc).”
North Yorkshire Partnerships, 2011
Assessing needs
HWBs are responsible for identifying and addressing local health and wellbeing needs, including undertaking Joint Strategic Needs Assessment (JSNA) and producing a Joint Health and Wellbeing Strategy (JHWS) based on local priorities (Department of Health/Local Government Association, 2011). JSNA’s should ensure that changing needs (e.g. housing, transport, demographics) are captured in local planning and that commissioning responds to the wider, societal determinants of health and health inequalities. In some areas, the JSNA will include a JSAA or Joint Strategic Assets Assessment, reflecting a growing interest in strengths-based approaches that capture health assets, as well as deficits, in local communities (Department of Health / Local Government Association, 2011; Foot & Hopkins, 2010).
A number of Health and Wellbeing Boards are using policy objectives from the Marmot Review to drive their health and wellbeing strategies and to ensure a focus on the wider determinants of health (Marmot, 2010; Commission on the Social Determinants of Health, 2008).
Place based approaches
HWBs have considerable potential to generate creative thinking and to encourage collaboration between councils, the NHS, the voluntary sector, communities and the public and to influence major shifts in local public sector spending. They reflect the importance of the ‘place shaping’ role of local government and will contribute centrally to how local people, especially those who are most vulnerable, experience their neighbourhoods. Joint Health and Wellbeing Strategies can be used to reflect growing evidence on the importance of mental health and wellbeing, the social, economic and human costs of mental health problems (Department of Health, 2010b) and to influence commissioning that promotes and protects mental wellbeing and supports recovery.
Recovery
Recovery oriented commissioning, that is working beyond the boundaries of conventional mental health systems, involves ensuring that people with mental health problems have a wide range of options for meeting their needs and aspirations, and that these are consistent with enjoying full citizenship and a life beyond services. This involves addressing how much people have to live on, housing, transport and getting out and about, opportunities for employment, training and education, safety, access to the natural world, leisure, sports and culture. In other words, the rich fabric of opportunities, activities, resources and relationships available where people live, which are central both to recovery and to public health. The responsibilities of HWBs include factors that have a strong influence on recovery and on opportunities for people with mental health problems (and other people with long term conditions) to determine how their support needs are met (Box 1). A recurring theme in the recovery literature is the importance of acknowledging and responding to the wider circumstances of people’s lives and experiences (Kalathil, 2011).
Much of the thinking about new approaches to providing care and support has come from mental health and disability rights and from people involved in the user, survivor and recovery movements (www.recoveryin-sight. com). There is still a considerable way to go before the full realisation of approaches which enable people with mental health problems to exercise real choice and control (Duffy, 2010a). It’s crucial that these issues are on the HWB agenda.
Box 1: HWB remit – factors influencing recovery
- Housing
- Education
- Transport
- Training and skills
- Employment
- Built and natural environment
- Income
- Social networks and neighbourhood life
- Arts and culture
- Sports and leisure
- Safety
- Primary care
Public mental health and wellbeing
Public mental health aims to improve mental health and wellbeing for the whole population and includes promotion and prevention, as well as achieving greater equity, quality of life and better outcomes for people experiencing mental ill health (Box 2).
Box 2: Cross government mental health strategy
No Health Without Mental Health is the key policy framework for promoting mental health and wellbeing, preventing mental health problems and improving treatment outcomes:
- More people will have good mental health
- More people with mental health problems will recover
- More people with mental health problems will have good physical health
- More people will have a positive experience of care and support
- Fewer people will suffer avoidable harm
- Fewer people will experience stigma and discrimination
Social determinants
Public mental health is concerned with the social determinants and understanding how factors like social position, occupation, income, housing, education and employment influence people’s mental health, including their chances of recovery (Campbell, 2010; Fair Deal for Wellbeing Discussion Kit). Public mental health is also centrally concerned with mental health inequalities, the impact of adverse events (violence, abuse, racism and other forms of discrimination) and the relationship between mental health and physical health (Fernando, 2010; Royal College of Psychiatrists, 2010). Poor mental health and wellbeing contribute to poorer outcomes in many areas of life, often reinforcing inequalities, because those who are most disadvantaged are most likely to experience both mental illness and poorer mental wellbeing. So, mental health is both a consequence and a cause of inequalities (Friedli, 2009).
Public Health England
Nationally, responsibility for public health, including public mental health, is transferring to a new public health service, Public Health England, sitting within the Department of Health. Public Health England will drive the new public health system, with greater alignment across the NHS, public health and social care, the integration of mental and physical health and a stronger focus on the prevention of ill-health. As part of this, it will support local public health services in ensuring that local commissioning takes full account of local mental health and wellbeing needs, and that local allocation of resources reflects these needs. In line with the leadership role of local government, Directors of Public Health (DPH) will be located within local authorities, with overall responsibility for health improvement in their areas.
Whole community approaches to recovery
Public mental health and the wider wellbeing movement are concerned with addressing the factors that influence mental wellbeing for everyone, whether or not they have a diagnosis, and with creating environments and cultures that support wellbeing: in schools, colleges, workplaces and on the streets. Public mental health can support recovery goals by asking what kind of communities support recovery and by investing in community based support that:
- builds community capacity
- reduces need and demand for specialist secondary mental health services
- alleviates the risk of crises.
This means support that is informed by needs assessment and consultation, building on knowledge of what people find helpful in their neighbourhoods (Box 3). This might include peer support groups, advocacy, tenancy support, adult education and training opportunities, sources of information and advice, e.g. on welfare rights or employment, as well as resources that support overall wellbeing and quality of life: culture and leisure services, public toilets, park benches and accessible footpaths.
From walking groups to literacy and numeracy classes, from learning English to managing debt, finding out about sources of low cost credit, tenancy maintenance, cookery classes and gardening projects, access to natural spaces and places to ‘stop and chat’, all neighbourhoods will have assets that support recovery and many are rich in community and voluntary organisations. Commissioning that supports and protects these sources of support, as well as identifying gaps and barriers to access, makes good economic sense (Department of Health, 2010b; Knapp et al., 2010) but may be vulnerable to short-term thinking in the current financial climate.
Box 3: Mental Wellbeing Impact Assessment
Mental Wellbeing Impact Assessment is a tool to assess and measure the impact of policy, planning and interventions on mental health and wellbeing. It has been widely used to inform planning and commissioning decisions and to ensure, for example, that the likely mental health impact of how a service or policy is delivered is taken into account.
It is built around four key factors that promote and protect mental wellbeing:
- enhancing control,
- increasing resilience and community assets,
- facilitating participation and inclusion,
- the wider social determinants of mental wellbeing: equity and social justice.
Mental Wellbeing Impact Assessment is also being used by local authorities to increase understanding of mental health and wellbeing and as a strategic tool for health and wellbeing boards.
(Cooke et al. 2011; Local Government Association, 2012)
Wellbeing debates
During 2011, The Office for National Statistics ran a public consultation on ‘what matters to people’s wellbeing’ , which will inform the development of new measures of national wellbeing (ONS, 2011).
A wide range of campaigns and agencies are involved in ongoing debates about what wellbeing means and what influences it (www.actionforhappiness.org/). Some are focussed primarily on individual wellbeing; others are concerned with wider economic and environmental factors (www.wellbeingproject. co.uk). Some councils are using ‘wellbeing’ to bring together different stakeholders, for example the Wellbeing and Happiness in Lambeth Programme (www.lambethfirst.org. uk/mentalwellbeing/). Wellbeing can provide an umbrella for exploring different cultural perspectives on health and mental health, for addressing issues of race and class (Fernando, 2010) and for reducing stigma and taboos around mental health problems.
Since publication of the Government Foresight Report (Government Office for Science, 2009), there has been growing interest in how mental health and wellbeing contribute to a wide range of outcomes – in education, employment, health, relationships, criminal justice and quality of life (Stoll et al., 2012). Increasingly, mental wellbeing or ‘mental capital’ is seen as an asset and a core element of resilience for individuals, families, organisations and communities.
Wellbeing and Recovery
Wellbeing is not only, or necessarily, about the absence of mental illness and there are many parallels between the literature on wellbeing and the principles of recovery, for example a common emphasis on what supports mental wellbeing, notwithstanding diagnosis or symptoms of illness. In this sense, a focus on wellbeing can be helpful in moving beyond narrow and contested definitions of mental illness, to address factors that underpin positive mental health for everyone, and to reduce inequalities in exposure to factors that are known to increase risk for mental health problems.
A valued life
Wellbeing is relevant to many different agendas that are also important to recovery, including health inequalities, social justice and the rights enshrined in the UN Convention on the Rights of Persons with Disabilities. The wellbeing literature also draws on a deeper understanding of the factors that make up a valued life for individuals, families and communities. These include a sense of meaning and purpose, opportunities to contribute, respect and dignity, freedom from racism and other forms of discrimination, feeling valued, family life and relationships, security, political voice, sense of belonging and affiliation (Nussbaum, 2011). People living in poverty, as well as other vulnerable or excluded groups, including people with mental health problems, consistently describe the pain of being made to feel of ‘no account’, which is often experienced as more damaging to wellbeing than material hardship.
This focus on the importance of values and social relationships is also central to assetsbased approaches and has influenced a greater emphasis on social outcomes or commissioning for social value i.e. how each pound spent also produces wider community wellbeing. Examples might include commissioning that supports family life, creates local jobs, empowers communities, strengthens control, uses local resources or skills and builds connections (O’Leary et al., 2011).
What a stronger focus on public mental health and wellbeing should mean for recovery
Recovery focuses on the individual: their unique experiences, values and preferences and emphasises the development of a personalised approach. This fits comfortably within clinical and social services where the development of a relationship between, say a professional and a service user, is crucial. In a recoveryoriented service the emphasis would be on coproduction, where attention to the perspective of the person is balanced by a supportive external perspective. In addition, there is a greater emphasis on moving the impact of services into the background, while supporting the relationship between people, their families and the communities in which they live. Professionals and others thus become available for help or intervention when needed, being “on tap, rather than on top”. These general principles are consistent with public health and wellbeing strategies which promote a greater sense of autonomy, agency and respect for people’s capacities.
Social justice
As well as emphasising recovery principles, personally valued goals and the need for mental health services to change, the recovery movement has also argued for social transformation to address the stigma and exclusion that are the common experience of people with mental health problems (Frese et al., 2009). In this way, recovery connects the personal with the political and is concerned with social justice, individual rights, citizenship, equality and freedom from prejudice and discrimination. A public health approach offers a strong focus on social determinants of health and on the reduction of health inequalities, which support the recovery movement’s concerns with social justice. Progress in these areas depends on changes that extend beyond the scope of health and health services, to economic, legal, political and social changes that support equity and the rights of all citizens, confronting for example poverty, the welfare system, discrimination, isolation and powerlessness (Duffy, 2011).
The principal ideas of recovery – hope, agency and opportunity – are also integral to practical considerations for citizenship: control over one’s life and decisions, setting one’s own direction, the means to shape one’s life, a place to belong, help from others and the opportunity to help others. This means an emphasis not only on personal development, but also on the need for collective support and reciprocity to allow people to build decent lives and for their communities to flourish (Duffy, 2012).
Social inclusion
“A focus on improving social inclusion, becoming social activists who challenge stigma and discrimination, and promoting societal well-being may need to become the norm rather than the exception for mental health professionals in the 21st Century.”
(Slade, 2010)
It is well documented that people with mental health problems, particularly those with long-term problems, are likely to be excluded from participating in many areas of society (Boardman et al., 2010). They are likely to have limited incomes, to be unemployed, have limited education or training, to have restricted social networks, to experience discrimination, to have few opportunities to engage in their local communities and to have poor physical health.
Being part of civil society has important implications for people with mental health problems to live a better life and one that they choose. They feel that it is important for themselves and their families to be part of their communities; to be valued members of those communities; to have access to the opportunities that exist in their communities and the prospect of contributing to them.
Community is both a means and an end (Duffy, 2010a). Rich and diverse communities provide opportunities for contribution, support and selfexpression: the conditions for full citizenship and for strengthening families and civil society. They also have potential to challenge stigma by providing a means of breaking down ignorance, prejudice and discrimination. The rights to a reasonable level of support, income and freedom from discrimination are essential components of this citizenship (Duffy, 2011).
Housing
Good housing is crucial for mental health and underpins recovery, social inclusion and citizenship. Settled housing provides the basis for individuals to build a more independent life and the opportunity to access employment, education, and the help and support they might need. Support with housing can improve mental health and help reduce the demand for health and social care (NHS Confederation, 2011).
Action to address housing is fundamental and, to be effective in improving recovery and reducing the unnecessary costs associated with poor access to housing and housing support, this means integration and collaboration across acute and secondary health care and housing (National Housing Federation, 2010; NHS Confederation, 2011; National Mental Health Development Unit, 2010). The creation of Health and Wellbeing Boards provides an opportunity for improving such collaboration and recognising the housing needs of people with mental health problems (NHS Confederation, 2011).
Employment
Like housing, employment is both a means of supporting wellbeing and an important indicator of recovery. Generally speaking, work is good for you (Waddell & Burton, 2006). People with long-term mental health problems have high rates of unemployment and worklessness is a key factor in contributing to their exclusion from mainstream society (Boardman et al., 2010). Lack of work is detrimental to mental health and wellbeing and it has been shown that, for people with mental health problems, having a job can lead to reduced symptoms, fewer admissions and reduced use of services.
Being in employment gives people the benefits of an income, social contact and a sense of purpose. There is a wealth of evidence for the effectiveness of supported employment schemes, in particular Individual Placement and Support (IPS), which aim to get people with severe mental health problems into paid competitive work (Sainsbury Centre for Mental Health, 2009b; 2009c). However, IPS is only patchily implemented in the United Kingdom and this deficit needs to be addressed by commissioners. Effective partnerships between health services, employers and employment agencies are essential to the process of getting people with mental health problems into work and supporting them while in work (Seymour, 2010).
Mental health problems contribute significantly to absenteeism and presenteeism and stigma and discrimination towards people with mental health problems in the workplace is high (Sainsbury Centre for Mental Health, 2007). The workplace offers important opportunities for improving wellbeing and combating stigma.
Recovery – from services to community development
The challenge for public mental health is to translate the principles of recovery, and what is known about recovery-oriented practices, into action at the community level. This may be easier where local authorities, for example Manchester City Council, are already commissioning mental health services in line with IMRoC principles.
Some suggestions are shown in Box 4. This involves change at two levels:
- First level change that benefits individuals through accessible services and opportunities which facilitate recovery.
- Second level change aimed at creating the conditions within communities that maintain recovery, including improving public attitudes, increasing access, reducing barriers and supporting connections.
(Onken, et al., 2007; Lanarkshire Recovery Network: Reflections and Future Focus http:// www.elament.org.uk/lanarkshire-recoverynetwork.aspx)
It is important that the principles of recovery are taken into community organisations and form the basis for staff training and the development of their organisational cultures.
The development of a strength-based approach, important for recovery-orientated practice (Slade, 2010) has its parallel in an assetbased approach to improve community health and wellbeing (Foot & Hopkins, 2010). These assets include the practical skills, capacity and knowledge of local residents, social capital, the effectiveness of local community and voluntary associations, and the resources of public private and third sector organisations. Assets-based approaches also place a strong emphasis on new models of partnership, where health and wellbeing are co-produced through more equitable and reciprocal relationships between health or social organisations and local communities (Foot & Hopkins, 2010; Solutions for Public Health, 2011).
Personalisation
The development of personal budgets and self-directed care is a key element of a recoveryoriented service (Alakeson & Perkins, 2012). Duffy (2010a; 2010b) has extended this into a personalisation model, the purpose of which is to allow people to take control of their own lives. This model contains four features: selfdirected support, co-production, communitybased support and total place commissioning. To operate this model requires support through the strengthening of informal networks, the extension of peer support, the use of community organisations, the engagement of support services and means of ensuring professional advice (Duffy & Fulton, 2010).
The use of peers is key to developing recoveryorientated services and this is reflected in public health developments. The challenge is developing not only a cadre of trained or formal peers, but also informal networks of peers and significant others. This would apply not only to people with mental health problems, but also their families and carers. The extension of the educational approach also requires co-produced solutions using peer trainers.
The development of community and public health approaches that support recovery through strengthening community and citizenship can complement, but not replace, good mental health services. It is important that the necessary support services and professional advice can be ensured when needed and that recovery-orientated mental health service are outward looking and are complemented and enhanced by parallel developments in local communities.
Box 4: Translating recovery principles and recovery-oriented activities into community developments
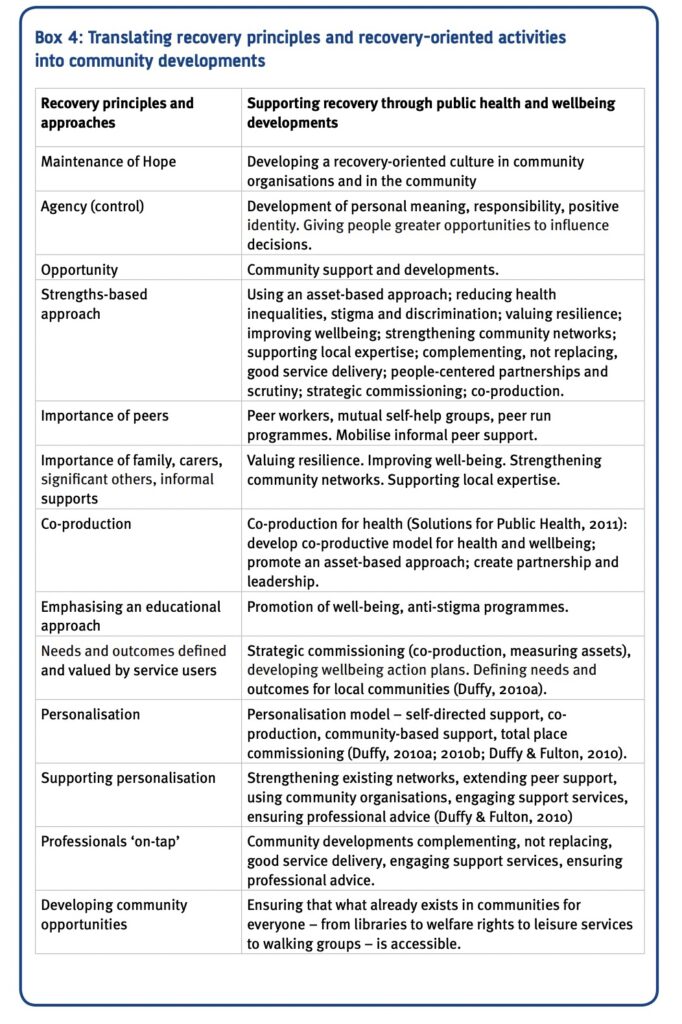
Commissioning for recovery: messages for Health and Wellbeing Boards
“Those most at risk are those without committed, unpaid relationships in their life. However good the service provider, people who have no one in their life who is not paid to be with them are vulnerable not only to abuse, but to gentle neglect and complacency.”
(Fitzpatrick, 2010)
- Recovery is made possible through access to everyday resources, relationships and opportunities, with professional support and services planned and organised around the needs and capacities of individuals, their friends and families. A core task for HWBs will be to ensure that Health and Wellbeing Strategies support the inclusion of people with mental health problems as full citizens.
2. Commissioning for Recovery involves two key principles:
- an overall commissioning strategy that reflects the importance of mental health and wellbeing and addresses the determinants of mental health;
- ensuring that people with mental health problems (and those who are vulnerable to poor mental health) have access to resources, opportunities and support from services that promote recovery.
3. The strength of the evidence on the importance of social contact, social relationships and social networks for public health, mental health and recovery (and the impact of isolation and loneliness, notably on those who are vulnerable or elderly), means that commissioning for social value should be central to Joint Health and Wellbeing Strategies. This includes addressing financial, environmental and service barriers that inhibit or undermine social relationships.
4. HWBs will need to provide leadership on the wider public mental health agenda, which creates a framework for commissioning that is ‘mental health aware’ and reaches out to those whose mental health needs are not being met, who face barriers in accessing support, have complex needs or experience multiple disadvantage (HM Government, 2012b). Improving mental health will contribute centrally to improving outcomes across a very wide range of domains (Department of Health, 2011a; 2011b; 2012a; 2012b).
5. The features of local communities that support recovery cut across all sectors, organisations and agencies: ‘good support can come from many places’ (Alakeson & Duffy 2011). HWBs will therefore have a crucial co-ordinating and partnership building role, notably with those outside health and social care e.g. local employers, schools and colleges, police and criminal justice, sports, leisure, culture and environmental services.
6. Knowing what mental health support is available, helpful and trusted and protecting valued assets for mental health will depend on:
- Finding ways to involve people with mental health problems and their networks, especially those whose voices are rarely heard, for example those who are homeless, gypsy travelers and other BME groups and young people;
- Building, maintaining and disseminating information about sources of support, particularly small scale community or business services, faith groups and informal networks that are not part of mainstream statutory or voluntary sector networks;
- Increasing accountability to those who use (and those who are reluctant to use) services (NICE, 2012);
- Using the evidence to demonstrate the value of prioritising mental health spending and thinking creatively about spend, e.g. linking up the ring-fenced public health budget with other budgets to join up services across the NHS and local government.
7. . Draw on the learning from approaches that have been successfully used in promoting recovery-oriented services. These include personalisation, co-production and peer support.
8. . Good housing is crucial for mental health and underpins both recovery and citizenship. Addressing housing is associated with a very wide range of improved outcomes and is also cost-effective. Collaboration between mental health services and housing agencies is essential
9. Employment is a key recovery outcome and important for wellbeing and inclusion. People with mental health problems should be supported to remain in work. There is a strong evidence base for schemes to support people with mental health problems into open employment. The joint strategic needs assessment should provide a view of the local mental health and employment situation (London Mental Health and Employment Partnership, 2012).
10. The principles of recovery oriented commissioning for people with mental health problems, with their focus on shifting power and control to those who use services, are also relevant to people with physical and intellectual disabilities, people with long term physical conditions and to addressing wider issues of equity, justice and empowerment raised by the user/survivor movement and advocates within the Black and minority ethnic mental health voluntary sector.
11. . Poverty, deprivation, exclusion and disadvantage are major barriers to recovery. Total place or ‘whole place’ approaches, which may include community budgets, are based on growing evidence that neighbourhood life is a key factor in health and other outcomes and that poor outcomes cluster at a very local level.
12. Concerted efforts to ensure that employment services meet the needs of people with mental health problems and addressing barriers to good quality employment, should be matched by ensuring that people are aware of their entitlements and dignity in entitlement.
References
Alakeson, V. & Duffy, S. (2011) Health efficiencies: the possible impact of personalisation on health care. Sheffield: Centre for Welfare Reform.
Alakeson, V. & Perkins, R. (2012) Recovery, Personalisation and Personal Budgets. London: Centre for Mental Health & NHS Confederation.
Boardman, J., Currie, A., Killaspy, H., Mezey, G. (2010) Social Inclusion and Mental Health. London: RCPsych publications.
Campbell, F. (editor) (2010) The social determinants of health and the role of local government. Available at: www.idea.gov.uk/idk/core/page. do?pageId=17415112
Commission on the Social Determinants of Health (2008) Closing the gap in a generation: health equity through action on the social determinants of health. Geneva: World Health Organization.
Cooke, A., Friedli, L., Coggins, T., Edmonds, N., Michaelson, J., O’Hara, K., Snowden, L., Stansfield, J., Steuer, N., Scott-Samuel, A. (2011) Mental Wellbeing Impact Assessment: a toolkit for well-being. 3rd ed., London: National MWIA Collaborative.
Department of Health (2010a) Healthy Lives, Healthy People: Our Strategy for Public Health in England. London: Department of Health.
Department of Health (2010b) No health without mental health: A cross-Government mental health outcomes strategy for people of all ages Supporting document – The economic case for improving efficiency and quality in mental health. London: Department of Health.
Department of Health (2011a) NHS Outcomes Framework. London: Department of Health.
Department of Health (2011b) Local Government leading for public health: factsheet. London: Department of Health.
Department of Health (2012a) Public health outcomes framework. London: Department of Health.
Department of Health (2012b) Adult social care outcomes framework. London: Department of Health.
Department of Health/Local Government Association (2011) New partnerships, new opportunities. A resource to assist setting up and running health and wellbeing boards. London: Department of Health.
Duffy, S. (2010a) Citizenship & Community. Finding the Key to Total Place. Working Paper Version 2.0. Sheffield: Centre for Welfare Reform.
Duffy, S. (2010b) Personalisation in mental health. Sheffield: Centre for Welfare Reform
Duffy, S. (2011) Real Welfare Reform. Sheffield: Centre for Welfare Reform.
Duffy, S. (2012) Peer Power: an evaluation of the personalisation forum group. Sheffield: Centre for Welfare Reform.
Duffy, S. & Fulton, K. (2010) Architecture for Personalisation. Sheffield: Centre for Welfare Reform.
Fair Deal for Wellbeing Discussion Kit Available at: www.ourlife.org.uk/ourlife/en/whatwe-offer/why-engage/a-fair-deal-for-wellbeingdiscussion-kit/
Fernando, S. (2010) Mental health, race and culture. London: Palgrave.
Fitzpatrick, J. (2010) Personalised Support. How to provide high quality support to people with complex and challenging needs – learning from partners for inclusion. Sheffield: Centre for Welfare Reform.
Foot, J. & Hopkins, T. (2010) A glass half-full: how an asset approach can improve community health and well-being. London: Improvement and Development Agency. From: www.idea.gov.uk/idk/aio/18410498
Frese, F.J., Knight, E.L., Saks, E. (2009) Recovery from Schizophrenia: with views from psychiatrists, psychologists, and others diagnosed with this disorder. Schizophrenia Bulletin 35, 370-380.
Friedli, L. (2009) Mental health, resilience and inequalities – a report for WHO Europe and the Mental Health Foundation. London/Copenhagen: Mental Health Foundation and WHO Europe.
Government Office for Science (2009) Foresight Mental Capital and Wellbeing. London: Government Office for Science.
HM Government (2011) No health without mental health: a cross government mental health outcomes strategy. London: Department of Health.
HM Government (2012a) No Health without Mental Health: Implementation Framework. London: Department of Health.
HM Government (2012b) Social justice: transforming lives. London: Department for Work and Pensions.
Joint Commissioning Panel for Mental Health (2012) Briefing. London: Royal College of Psychiatrists.
Kalathil, J. (2011) Recovery and Resilience: African, African-Caribbean and South Asian Women’s narratives of recovering from mental distress. London: Mental Health Foundation.
Knapp, M., Bauer, A., Perkins, M., Snell, T. (2010) Building community capacity: making an economic case. University of Kent: PSSRU.
Local Government Association (2012) Mental Wellbeing Impact Assessment – Programme 2011. London: Local Government Association.
London Mental Health and Employment Partnership (2012) Incorporating mental health and employment in your Joint Strategic Needs Assessment and Health and Wellbeing Strategy. London: NHS London
Marmot, M. (2010) Fair Society, Healthy Lives. The Marmot Review. Strategic review of health inequalities in England post-2010. London: The Marmot Review.
National Housing Federation (2010) Health and housing: worlds apart? Housing care and support solutions to health challenges. London: National Housing Federation.
National Institute for Health and Clinical Excellence (2012) Quality standard for service user experience in adult mental health. London: NICE.
National Mental Health Development Unit (2010) Mental Health and Housing. Housing on the Pathway to Recovery. London: National Mental Health Development Unit.
NHS Confederation (2011) Housing and Mental Health. Briefing. Issue 233. London: NHS Confederation.
North Yorkshire Partnerships: Health & Wellbeing Board (2011) Available at: www.nypartnerships.org. uk/index.aspx?articleid=16804
Nussbaum, M. (2011) Creating capabilities – the human development approach. Cambridge, Massachussets and London: Harvard University Press
Office of National Statistics (2011) Measuring national wellbeing. Measuring what matters: National Statistician’s reflections on the national debate on measuring National Well-being. London: Office of National Statistics.
O’Leary, T., Burkett, I., Braithwaite, K. (2011) Appreciating Assets. London: IACD & Carnegie UK Trust.
Onken, S.J, Craig, C.M., Ridgeway, P., Ralph, R.O., and Cook, J.A. (2007) Analysis of the definitions and elements of recovery: a review of the literature. Psychiatric Rehabilitation Journal 31(1) 9-22
Royal College of Psychiatrists (2010) No health without public mental health: the case for action. London: Royal College of Psychiatrists.
Sainsbury Centre for Mental Health (2007) Mental Health at Work: Developing the Business Case. Policy Paper 8. London: Sainsbury Centre for Mental Health.
Sainsbury Centre for Mental Health (2009a) Implementing Recovery – A new framework for organisational change. London: Sainsbury Centre for Mental Health.
Sainsbury Centre for Mental Health (2009b) Doing what works. Individual placement and support into employment. Briefing 37. London: Sainsbury Centre for Mental Health.
Sainsbury Centre for Mental Health (2009c) Commissioning what works. The economic and financial case for supported employment. Briefing 41. London: Sainsbury Centre for Mental Health.
Seymour, L. (2010) Common Mental Health Problems at Work. What we know about successful interventions. A progress review. London: Sainsbury Centre for Mental Health.
Shepherd, G., Boardman, J., & Slade, M. (2008) Making Recovery a Reality. London: Sainsbury Centre for Mental Health.
Slade, M. (2010) Mental illness and well-being: the central importance of positive psychology and recovery approaches. BMC Health Services Research 10, 26.
Solutions for Public Health (2011) Co-production for health: a new model for a radically new world. Oxford: Solutions for Public Health.
Stoll, L., Michaelson, J., Seaford, C. (2012) Wellbeing evidence for policy: A review. London: New Economics Foundation.
Waddell, G. & Burton, A.K. (2006) Is work good for your health and well-being? London: TSO.
Personal health and social care budgets can help people with a mental health condition to set their own goals and rebuild their lives.
This paper discusses how the twin concepts of personalisation and recovery are transforming mental health services in the UK.
2. Recovery, Personalisation and Personal Budgets
Vidhya Alakeson and Rachel Perkins
Introduction
There are two subjects that have the potential to shape mental health policy and practice in the UK and internationally: recovery and personalisation. Both have emerged independently and are prominent in the Government’s mental health strategy, No Health Without Mental Health (Department of Health, 2011). In similar ways, both challenge the current predominance of professional, clinical knowledge over the expertise of lived experience in the mental health system and require significant changes in the culture, practice and organisation of mental health services. At their core, both recovery and personalisation are rooted in self-determination and reclaiming the rights of full citizenship for people with a lived experience of mental health problems.
The purpose of this paper is to explore the links between recovery and personalisation and demonstrate how both are part of a common agenda for mental health system transformation. While personalisation in mental health services is a more recent concept, it builds on approaches that are already underway as part of recovery-oriented practice. In fact, personalisation, personal budgets (PBs) in social care and personal health budgets (PHBs) in the NHS can help embed and enhance recovery-oriented practice.
The first part of this paper describes personalisation, personal budgets and personal health budgets. The second sets out the shared philosophy and objectives of recovery and personalisation and discusses what the two approaches mean for changing the current service system. The third part focuses on personal health budgets as tools for recovery and identifies the eight core features that need to be put in place if recovery-oriented services are to maximise the potential of personal health budgets.
Personalisation, personal budgets and personal health budgets
Having left institutions, many disabled people found themselves living in the community but segregated from others and denied the opportunity to play a full part in family and community life. This led to a call for independence that was expressed most clearly in the desire of individuals to take control of their support in order to create a more meaningful, more integrated and more fulfilled life for themselves as active participants in the community (Brewis & Fitzgerald, 2010). The concept of personalisation was developed in part as a response to the demands raised by the ‘independent living’ movement defined as “all disabled people having the same choice, control and freedom as any other citizen – at home, at work, and as members of the community” (Disability Rights Commission, 2002).
Personalisation emphasizes greater individual control of the resources and supports needed to enable people to participate as equal citizens and pursue their own ambitions and aspirations rather than those determined for them by services and professionals (PMSU, 2005; ODI, 2008). Personal budgets in social care and personal health budgets in the NHS are, therefore, tools to support the personalisation of health and social care services.
A personal budget is an allocation of social care or NHS resources or an integrated allocation of both that is controlled by an individual and can be used to meet identified goals. PBs and PHBs give individuals and their carers greater say over how their health and social care needs are met. They do this by transferring control of public resources to individuals rather than having the state commission services on their behalf. Individuals can receive the money directly, it can be managed by an independent third party, or can be held as a virtual budget by commissioners. Whichever way individuals choose to receive the money, they should still be able make the decisions that matter most to them.
PBs and PHBs are also more than a budget; they are the basis of a different conversation between individuals, those who support them and clinical professionals in which each shares information and expertise to produce better outcomes. There are seven basic steps in the personal budget or personal health budget process, which are set out in the box overleaf
Putting People First (LGA, ADASS, NHS, 2007) made personalisation and personal budgets the cornerstone of policy in adult social care, meaning “every person across the spectrum of need, having choice and control over the shape of his or her support, in the most appropriate setting”. For some, exercising choice and control will require a significant level of assistance either through professionals or through independent support brokers. Local Authorities have subsequently committed that by 2013, all adults using community-based social care services will have a personal budget.
Personal health budgets were first proposed in the 2008 Darzi Review (Department of Health, 2008), with a national pilot programme launched a year later alongside an in-depth evaluation (Department of Health, 2009). PHBs were introduced into the NHS having been found to improve satisfaction and quality of life in social care across a range of disabilities at the same time as improving value for money. In its report to the government on NHS modernisation, the NHS Future Forum called for greater drive behind the implementation of personal health budgets (NHS Future Forum, 2011). In response, Andrew Lansley, Secretary of State for Health, committed to roll out the right to ask for a PHB in Continuing Healthcare in 2014, with other parts of the NHS to follow (see http://www.personalhealthbudgets. dh.gov.uk/News/item/?cid=8390 for details).
Twenty six pilot sites across the country are experimenting with PHBs for mental health in areas such as early intervention, assertive outreach, high-cost residential placements, psychological therapy services, older people’s mental health services and in community mental health teams (see www.personalhealthbudgets. dh.gov.uk for further details). A small number of pilots are also underway in the United States and in Western Australia. One of the central reasons why PBs and PHBs are effective tools for recovery is that the very approach embeds the three core components of recovery: hope, control and opportunity (Repper & Perkins, 2003, 2012; Shepherd et al., 2008).
The seven step personal budget process
- The first step is for individuals to complete an assessment or self-assessment questionnaire that identifies areas where they need support.
- The assessment generates a score which is linked to a resource allocation system (RAS) to produce a personal budget amount. The RAS ensures that resources are allocated in a fair and transparent way to individuals according to need.
- The personal budget amount provides the starting point for developing a recovery support plan which identifies the goals a person has for his or her recovery and how those goals could be met. People can plan by themselves, with the support of friends and family, with peer support or with a professional broker. There is no set menu for support, allowing people and their supporters to develop highly personal, creative solutions.
- The support plan is approved on the basis of being financially and clinically appropriate. Since there is no fixed menu, approval should focus on the likelihood that the support plan will contribute to a person’s recovery.
- Individuals can exercise as much or as little direct control over the money in their personal budget as they choose. They can receive it as a direct payment which they manage, they can use a third party to manage the money on their behalf or it can be held by a provider or commissioner.
- With decisions about the money made, the services and supports in the plan can be put in place, either by the person themselves or by the organisation that holds the budget in collaboration with them.
- A person’s support plan is reviewed on a regular basis and its effectiveness is judged on the basis of whether the goals identified in the plan are being met and the person is progressing in their recovery. If a person’s needs change significantly, they will complete a new self-assessment and will be allocated a new personal budget amount.
Recovery and personalisation: a shared purpose
Recovery and personalisation see people who use services as “whole people in their whole context” (Brewis & Fitzgerald, 2010). This means recognizing that alongside the diagnoses, deficits and dysfunctions individuals may have, they also have strengths, skills and assets to contribute. They have likes and dislikes, preferences, tastes and values. Everyone is more than a ‘mental patient’ and occupies multiple roles as, for example, parent, sibling, child, employee and carer. An individual’s social context also brings with it strengths and possibilities for enhanced recovery. The support of family members, social networks or having a valued role in the community can all provide the hope that drives individual recovery.
Recognising individuals as whole people and harnessing their strengths, preferences and motivations will strengthen the possibility of recovery. In the context of personalisation, the ‘real wealth’ framework (see box on the right) has been developed to define the factors that underpin the quality of people’s lives (Duffy, 2010). The challenge for the mental health system is to enhance not deplete the ‘real wealth’ that provides the basis for individual recovery and a fairer society.
For example, the common failure to take psychiatric medication often stems from the negative effects of prescribed medicines on facets of life that individuals consider important, such as their role as a parent or employee – their real wealth. These activities have also been described as ‘personal medicine’ – the everyday activities that can be a source of motivation and have significant therapeutic value (Deegan, 2005). A conflict between professionally recommended treatment and ‘personal medicine’ arises when medical professionals fail to consider the individuals when making treatment decisions (Deegan & Drake, 2006).
The five dimensions of real wealth
- Strengths – Each person is endowed with a particular set of strengths and weaknesses. These strengths go far beyond the physical and include skills, interests and even needs.
- Relationships – One of the most important guarantees of good physical and mental health is to have friends, family and other supporters. In times of difficulty, friends and family are usually the most important source of support.
- Community – Most individual achievements are only possible to the extent that people are able to access appropriate opportunities from within a community. Work, education, contribution and personal expression all rely on community opportunities.
- Control – A person’s ability to access the community, build relationships and use their individual strengths all depend on having control over the future. Some elements of control are dependent on access to financial resources. A lack of control makes it impossible for a person to fully realise their goals.
- Resilience – Perhaps the most important factor that determines the ability of a person to achieve good outcomes is their own sense of resilience, their ability to see and value positive opportunities and not to be overwhelmed by difficulties and problems. This can also be thought of as hope.
Source: www.centreforwelfarereform.org.uk
What recovery and personalisation mean for current systems and services
Today’s mental health services are organized around the three Cs: cure, care and containment. The primary focus of services is one of cure: the reduction/elimination of symptoms or problems. Unless and until a person’s problems can be eliminated they are ‘cared for’ and, should they be a threat to their own health and safety or that of others, they are ‘contained’ (Perkins, 2012; Perkins & Slade, 2012). This focus does not recognize the basic goals that most individuals have for their lives: to have meaningful activity; to have meaningful relationships; and to have a place to call home (Nerney, 2011). Recovery and personalisation challenge the mental health system to support individuals to achieve these goals. They call into question the current ‘gift model’ in mental health services in which professionals are in control and individuals are recipients of the care and treatment decided by these ‘experts’ (Duffy, 2010).
The scale of the challenge to the current system was well documented in a series of papers by the NHS Confederation that reported the views of Chief Executives, mental health clinicians and service users about personal health budgets. Demand for PHBs among service users was strong as all wanted to change something about their current care package but few were optimistic about gaining greater control (NMHDU and Mental Health Network, 2009, 2011a, 2011b). Each group saw significant barriers to the implementation of PHBs in the NHS, many of which were linked to current culture and practice. As one psychiatrist remarked:
“I’m a highly trained, highly expert specialist in a field which has involved many years of training, many years of clinical experience, and my job is to know the best evidence and best practice. It would be completely against my code of practice to say to a young person, yes go ahead and spend money on something that has no evidence base.” (NMHDU & Mental Health Network, 2011a).
The three most important challenges posed by recovery and personalization for the mental health system are:
- shifting the established balance of power between individuals and professionals,
- ending the dominance of clinical treatment, and
- reorienting the system towards wider social outcomes.
Shifting the balance of power
Central to the challenge that recovery and personalisation pose to the existing service system is the issue of who holds the power and control (see Repper & Perkins, 2003, 2012; Shepherd et al., 2008). Personalised recoveryfocused practice requires recognising two sorts of expertise: professional expertise grounded in research, training and clinical experience and the expertise of having lived with a mental health condition. The challenge for services is to move from attempts to ensure compliance with ‘expert’, professional prescriptions to a process of shared decision-making that brings together these two types of expertise, shifting from a ‘gift model’ to a ‘citizenship model’ with the individual at the centre of the service system (Duffy, 2010).
“Shared decision making diverges radically from compliance because it assumes two experts – the client and the practitioner – must share respective information and determine collaboratively optimum treatment …. It helps to bridge the empirical evidence base, which is established on population averages, with the unique concerns, values and life context of the individual client. From the vantage point of the individual healthcare client, the efficacy of a particular medication is not certain … the question of how the medication will affect the individual becomes an open experiment for two co-experimenters – the client and the practitioner.” (Deegan & Drake, 2006)
Striking a better balance between the two types of expertise is particularly important for longterm conditions such as mental health problems where the condition and its impact on everyday life have to be managed by individuals and their families, with only intermittent intervention from professionals. Even a person receiving intensive support from an Assertive Outreach Team will see a clinician for no more than 156 hours in a year (3 hours per week). This constitutes but a small fraction of the person’s life.
A new relationship with clinical treatment
Linked to the concept of a power shift has to be a move away from the centrality of clinical treatment as the only valid route to well being. Some people find treatment – whether psychological of pharmacological – helpful, but treatment forms only a part (and probably a smaller part than most professionals would care to acknowledge) of what is often a rich tapestry of ways in which people manage the challenges they face.
”Over the years I have worked hard to become an expert in my own self-care… Sometimes I use medications, therapy, self-help and mutual support groups, friends, my relationship with God, work, exercise, spending time in nature – all of these measures help me remain whole and healthy, even though I have a disability.” (Deegan, 1993)
Professionals will remain important, they have important tools to share: the latest guidelines, knowledge of research evidence and experience from clinical practice. But in a recoveryoriented system, professional expertise should be ‘on tap’, not ‘on top’ (Repper & Perkins, 2003, 2012; Shepherd et al., 2008). It should be readily on hand and available when it is needed but it is up to individuals how they use that knowledge and the extent to which it is balanced by other approaches and priorities. The value of professional treatment and intervention lies in supporting self-care and the pursuit of individual ambitions.
From service silos to health and social outcomes
Supporting people to rebuild their lives means breaking out of existing service silos dictated largely by government funding and bureaucratic systems to pursue improvement in outcomes. It means placing greater emphasis on services such as housing, friends and social networks, education and employment alongside clinical care and treatment. This will involve greater coordination across public services as well as greater flexibility in the way NHS and social care resources can be used. A college course may help someone recover and a computer connected to the internet may keep someone safe enough to remain out of hospital, but neither would traditionally be paid for by the NHS. It will also mean greater use of universal services and community resources that promote inclusion and social connection, in contrast to community-based services that have often trapped people in segregated settings (Boardman & Friedli, 2012).
Personal health budgets as tools for recovery
The extension of personalisation from social care into the NHS creates new opportunities to use personal health budgets to support recovery. There is, as yet, no blueprint for exactly how PHBs should work, where they are most effective and the appropriate scope for individual control. A lot of experimentation has been undertaken through the pilot programme that will inform these questions. But the eight features discussed below will need to be put in place if PHBs are to be effective tools for recovery:
- A simple, fair resource allocation system
- Effective recovery planning (combined with effective support when required)
- New approaches to opportunity and safety
- A more diverse workforce
- Monitoring on the basis of outcomes not spending
- A new evidence base
- A more diverse market
- Sustainable funding
1. A simple, fair resource allocation system
For individuals to take control of their recovery and be able to plan effectively how best to use the resources at their disposal, it is important for them to know upfront how much they have to plan with. This does not mean that the budget is the only important dimension of a PHB. In fact, it is the change in the conversation that happens through a well-functioning recovery planning process that is critical. But a transparent allocation of resources is a good starting point for planning and it protects equity while allowing a range of ways in which people are supported.
The PHB pilot features three broad approaches to resource allocation:
- Small, one-off payments are being used to enhance individual recovery.
- Resource allocations systems that match an assessment of need to an amount of money. This is the approach being taken in Croydon (see box above).
- PHBs based on the cost of existing packages of care. This has been the approach taken with large, residential care packages.
In addition, attempts are being made to integrate NHS and social care resources to provide individuals with a single, integrated budget and planning process. It will be critical to ensure that allocation systems for PHBs remains simple and focused on recovery and do not become overly complicated and bureaucratic, as they have done in some Local Authorities (TLAP, 2011).
2. Effective recovery planning
For personal health budgets to be effective, planning must focus on a person’s whole life – what is good, what could be better, what matters most to them and what are their goals and aspirations. The planning that the mental health system does for and with individuals should, therefore, be seen as only one contribution to self-management. For people who are subject to the Care Programme Approach (CPA), that care plan can be integrated into a single plan to support recovery that the person manages as part of their own selfmanagement plan, Personal Recovery Plan or ‘Wellness Recovery Action Plan’
A recovery support plan does not have to be written for a particular length of time. It may be that a short-term plan for the next month is most appropriate, with a longer term plan to follow. It is possible to build contingencies into the plan. For example, some people find a short stay in a bed and breakfast or increased support from a personal assistant at home a particularly effective form of respite that can prevent hospitalisation. They can keep money aside from their budget to pay for this when it is needed. Clinicians can be too bound by traditional ways of thinking to be effective at recovery planning. Independent support brokers can be effective but can significantly add to costs. Friends and family members, peers with lived experience and members of the community can all provide support for recovery planning. If everyone who develops a recovery plan supports one other person to plan, the costs can be kept to minimum. (Financial sustainability is discussed further below.)
Croydon’s Resource Allocation System (RAS)
This is the approach to resource allocation taken in the Croydon PHB pilot for substance misuse. Several of the domains in Croydon’s RAS would not attract funding in the traditional substance misuse treatment system. However, Croydon has adopted a more recovery-oriented approach and recognizes the importance of supports outside of traditional treatment. The system allocates funding against the following domains through a supported selfassessment questionnaire that individuals complete with a care navigator:
- Opiate use stabilization,
- Ongoing prescribing (opiate substitute),
- Detoxification,
- Help with symptoms of withdrawal,
- Practical barriers/obstacles to treatment,
- Risk and harm reduction,
- Helping individuals to change their behaviour/use of substances,
- Emotional and mental health,
- Key relationships/ family and friends,
- Community integration and community life.
Responses to statements/descriptors under each of these domains produce a score which is then linked to an allocation of resources. Not all individuals will attract resources in all domains of the RAS. An individual’s personal health budget is the sum total of the allocations in each domain.
The domains of the RAS do not restrict how a personal health budget is used. The support planning process helps the personal health budget holder to make best use of the PHB alongside universal services and other community resources.
3. New approaches to safety and opportunity
Recovery depends on individuals having control and access to opportunities and this raises concerns about safety. However, it is important to remember that recoveryoriented and personalised services are built on shared decision-making and the coproduction of outcomes between clinicians and individuals. Relationships based on a thorough understanding of a person’s perspective and values can increase safety (Scott-Moncrieff et al., 2009). When individuals are involved in making choices, they are more likely to better manage any risks involved. When individuals choose who is involved in their care, they are more likely to stay safe and when they work in partnership with clinicians and can enter into an honest conversation about choices, there are fewer risks involved (Langen & Lindow, 2004; Perkins & Goddard, 2008). (There will be a paper in this series on risk, due out later in 2012 – see Boardman & Roberts, 2012.)
4. Creating a more diverse workforce
In order to implement personal health budgets, professionals are required to work in different ways with individuals, supporting them to make choices rather than developing care plans on their behalf. When asked about PHBs, clinicians, irrespective of their professional background, were most concerned about the tensions between individual choice and their professional duty of care. In addition, GPs, psychiatrists and psychologists were most concerned about individual choice in the context of evidence-based care and the extent to which PHBs would result in better health outcomes. Occupational therapists, social workers and nurses who generally have more experience of PBs, were primarily concerned that PHBs would add to bureaucracy (NMHDU and Mental Health Network, 2011a). This full range of concerns will need to be addressed in adapting the workforce to work effectively with PHBs.
Some roles that are currently performed by professionals may be taken over by peer workers in a more personalized, recoveryoriented system. The involvement of peer workers and third sector organizations in the delivery of services could allow clinical professionals to become more focused on those tasks where they have unique skills and expertise. (There will be a paper in this series on peer support, due out later in 2012.)
Peer support will be critical to personalisation. Peers can provide informal support for recovery planning as discussed above. Trained peer workers are being used as recovery coaches in PHB programmes such as Texas Self-Directed Care (www.texassdc.org). Using disabled people and user-led organizations to provide support planning for PBs in social care has been shown to create a more person-centred and less bureaucratic process than support provided by Local Authorities (Campbell et al., 2011).
5. Monitoring on the basis of outcomes not spending
Recovery support plans should be regularly reviewed to ensure that their goals are being met. Individuals are held accountable for meeting the goals and not for each individual purchase they make. This is more important than closely monitoring spending. The case study opposite provides an example of the health and social objectives that Ann, a PHB holder in Northamptonshire, has chosen and the mix of clinical and non-traditional services and supports that she is using to meet those objectives.
Individuals have the strongest incentives to make good use of their personal budget and generally maximise value for money more effectively than commissioners. Nevertheless, concerns about fraud and abuse are frequently raised in the context of personalization. There is almost no evidence internationally of significant fraud and abuse and programmes can be designed to maximize accountability. For example, PHBs can be held by a third party rather than being directly paid to individuals in the form of a direct payment to increase financial control. This may be appropriate where individuals have, for example, serious addiction issues.
6. Building a new evidence-base
Recovery and personalisation call for the development of a new evidence base looking at the effectiveness of treatment, care and supports in generating ‘real wealth’ and supporting individuals to live the lives they choose.
There is currently a limited evidence base related to the contribution of clinical care and other interventions to the wider, life outcomes that people care about most. There is no evidence as to whether Clozapine is effective in helping a person with schizophrenia to get a job or whether cognitive behaviour therapy helps someone with depression to find a partner. The evaluation of the PHB pilot programme will develop this evidence base by assessing the extent of the clinical improvement and recovery that is secured through individual choice and control compared to treatment as usual.
7. Creating a more diverse market
For personalisation and recovery to succeed, there needs to be a range of alternative provision in place. Although PHBs can be used to purchase mainstream opportunities that promote wellbeing (like joining a gym to increase physical health, or driving lessons to enable a person to see their family and friends), early experience with personal health budgets shows that investment in creating new provision can pay off. In the PHB pilot for alcohol detoxification in Southampton, for example, work with providers has led to the creation of a range of alternatives to inpatient detoxification that did not previously exist. In social care personal budgets, Stockport has developed an online market place that allows individuals to find a broad range of providers, from providers of clinical services such as physiotherapy to music teachers and yoga instructors.
However, there is a risk of moving too quickly to give individuals a budget before there is anything available outside of statutory services. It is, therefore, important to find ways to ensure that people can access assured alternatives when contracts are changed and that changes happen on a timescale that allows investment in alternatives to occur. Some areas rapidly closed day services and individuals were given a personal budget as an alternative but found little else on offer locally. Notional budgets that designate a certain level of resources to each individual without removing the money from existing contracts can be an important intermediate step towards personalisation. Individual service funds that allocate funding for individuals to a provider who then develops a package of services and supports in collaboration with the individual can also act as a stepping stone.
Ann’s personal health budget: a case study from the Northamptonshire PHB pilot
Ann is a mother and grandmother from Northamptonshire, with a large family who care for her. She has depression, anxiety and a personality disorder and has been using mental health services for ten years. She was taking approximately 36 overdoses a year but with help from her community mental health team (CMHT), other mental health services and learned self-help techniques she had managed to reduce this to three to five times a year. Last year she had 18 overnight inpatient stays, three respite stays and 49 contacts with professionals from the CMHT.
Ann was eligible for a PHB as part of Northamptonshire’s mental health pilot. Her indicative budget was calculated based on the cost of the CMHT service in the previous 12 months, a clinical assessment of her health status and from this, an estimation of the CMHT services that she was likely to use in the following 12 months. Ann’s care coordinator discussed the budget allocation with her and the final amount was agreed by Ann.
One of Ann’s central objectives from her recovery support plan is to be able to help her family rather than being a source of concern to them. Some of the other outcomes that Ann wants to achieve with her budget include:
- Reducing her demand on the CMHT, on acute mental health services and on her GP
- Reducing the number of overdoses she takes,
- Increasing her confidence and socialisation and decreasing her self-harming behaviour,
- Reducing her reliance on medication, and
- Cutting down or stopping smoking.
With her PHB, Ann has bought regular, twice weekly psychotherapy sessions, 3 contacts with her consultant psychiatrist and a minimum of 25 contacts with her care coordinator. A short course of NHS psychotherapy in the past had started to work for Ann so she negotiated to reduce her contacts with her care coordinator and psychiatrist to free up funds to pay for a private psychotherapist, one that she chose herself.
Ann has now had a PHB for seven months and is making steady progress towards achieving her health outcomes. So far she has had no inpatient admissions or overdoses. She has not needed to use the crisis team or respite service. She has reduced her contact with her psychiatrist, from once every three months to once every four months. She has less contact with her care coordinator and there is a possibility that she will be discharged from the CMHT in 2012/13. She has reduced her medication and has lost some weight. She is especially pleased that her relationship with her family, her children and grandchildren has greatly improved. She sees a lot more of them now because she has changed so much. They are not so frightened for her any more and want to see her more often.
8. Sustainable funding
While the personal health budget pilot programme did attract additional funding from the Department of Health, the long term sustainability of PHBs will depend on the extent to which they can be implemented on a cost neutral basis, at least over time. Experience from the pilot sites indicates that the upfront costs of implementation were on average £150,000 over two years, with the expectation that ongoing costs will be less as PHBs become embedded into existing NHS delivery structures. This figure represents investment in developing local systems and procedures, including support for individual planning (Jones et al., 2011). The final report of the national evaluation will assess the extent to which upfront investment improves outcomes for PHB holders by creating a more effective process and, therefore, improves value for money in the long run.
Local areas will need to find some initial investment for implementation. However, the bigger challenge is to free up money to provide personal health budgets themselves and to fund ongoing support for recovery planning thus avoiding double running costs (NMHDU and Mental Health Network, 2009). Much of the money in the mental health system is currently tied up in block-purchased contracts with NHS provider organisations in secondary care. Unless some of this money can be released to invest in personal health budgets, it is difficult to see how they can be taken to scale. Until then, individuals’ choices will be restricted to commissioned services.
There is emerging evidence that PHBs can reduce use of emergency and secondary mental health services. However, these savings will need to be released by decommissioning some services if the funding is to be redirected into personalization. Taking money out of secondary care to invest in community services is a long standing challenge in the NHS and one which personalisation only makes more acute (Davidson et al., 2012).
In this context, the development of mental health Payment by Results (PbR) may be helpful. Although there are serious doubts about the consistency between the cash value attributed to care clusters through PbR and the resources allocated to individuals with similar levels of need through PHBs, Payment by Results could provide a catalyst to break up block contracts. By allowing money to move more freely around the system, PbR may benefit Personal Health Budgets. However, the relationship between the two will need to be carefully managed if Payment by Results is not to limit the flexibility of PHBs given the clinical definition of care clusters within PbR (Clarke, 2011).
Conclusion: Recovery and personalisation: raising expectations
Many people in mental health services have lost hope for the future. They have been told not to expect to work or find a partner, not to expect the things that other people take for granted. The system has focused on problems and disorders and has often eroded aspirations. This lack of hope for the future creates a culture of low expectations that affects those who use services as much as those who provide them. In the end, low expectations become a self-fulfilling prophecy as life is reduced to being defined as a user of mental health services. ‘Real wealth’ is eroded and replaced by isolation, dependence on services and the failure to participate in society as a full citizen.
Recovery-oriented services demand a new attitude. Professionals and providers must challenge themselves and the individuals they work with to have high expectations of what is possible. The culture of services must offer people opportunities to rebuild their lives through an individual journey that accepts what has happened and moves beyond it. The success of the recovery approach should be judged according to the changes it achieves in people’s lives and the extent to which it enables people to achieve the goals they set for themselves, not solely how well their symptoms are managed.
Personal health budgets provide a tool to enable this individual journey, recognizing and nurturing individuals in their many different roles, with aspirations for the future and talents to contribute. Services that embed the principles of recovery and personalisation must offer hope and challenge, not limiting people to the confines of their disorders, but supporting them to define and realise a life that they choose and value.
References
Boardman, J. & Friedli, L. (2012 forthcoming) Recovery, Public Mental Health and Wellbeing. In press.
Boardman, J. & Roberts, R. (2012 forthcoming) Risk, Safety and Recovery. In press.
Brewis, R. & Fitzgerald, J. (2010) Citizenship in Health: Self-direction theory to practice. Wythall, West Midlands: In Control Partnerships.
Campbell, N., Cockerell, R., Porter, S., Strong, S., Ward, L. and Williams, V. (2011) Independent Living Strategy: Support planning and brokerage. Final report from the support planning and brokerage demonstration project. London: Office for Disability Issues.
Clark, M. (2011) Mental health care clusters and payment by results: considerations for social inclusion and recovery. Mental Health and Social Inclusion, 15 (2). pp. 71-77.
Davidson et al. (2012) Personal Health Budgets: Experiences and outcomes for budget holders at nine months. Fifth Interim Report. London: Department of Health.
Deegan, P. (1993) Recovering our sense of value after having been labelled mentally Ill. Journal of Psychosocial Nursing and Mental Health Services, 31, 7-11
Deegan, P. (2005) The importance of personal medicine: A qualitative study of resilience in people with psychiatric disabilities. Scandinavian Journal of Public Health, 2005; 33 (Suppl 66): 29–35
Deegan, P. & Drake, R. (2006) Shared Decision Makingand Medication Management in the Recovery Process. Psychiatric Services, 57, 1636-1639
Department of Health (2008) High Quality Care for All. London: Department of Health.Department of Health – Primary care and Community Services (2009) Personal Health Budgets: First Steps. London: Department of Health.
Department of Health (2011) No Health Without Mental Health: A Cross-Government Mental Health Outcomes Strategy for People of All Ages. London: HM Government.
Disability Rights Commission (2002) Policy Statement on Social Care and Independent Living. London: Disability Rights Commission.
Duffy, S. (2010) Personalisation in Mental Health. Sheffield: Centre for Welfare Reform in association with Yorkshire and Humberside Improvement Partnership, Care Pathways and Packages Project & Association of Directors of Adult Social Services.
Jones et al. (2011) The Cost of Implementing Personal Health Budgets. PSSRU discussion paper. London: Department of Health.
Langen, J. & Lindow, V. (2004) Living With Risk. Bristol: Policy Press.
Local Government Association, Association of Directors of Adult Services and NHS (2007) Putting People First: A shared vision and commitment to the transformation of Adult Social Care. London: HM Government.
Mental Health Network and National Mental Health Development Unit (2009) Shaping Personal Health Budgets: A view from the top. London: NHS Confederation.
National Mental Health Development Unit and Mental Health Network (2011a) Facing Up to the Challenge of Personal Health Budgets: The view of frontline professionals. London: NHS Confederation.
National Mental Health Development Unit and Mental Health Network (2011b) Personal Health Budgets: The views of service users and carers. London: NHS Confederation.
Nerney, T. (2011) Lost Lives: The paucity of quality in human services. Michigan: Centre for Self-Determination (see www.centerforself-determination.com)
NHS Future Forum (2011) Choice and Competition: Delivering real choice. London: Department of Health.
Office of Disability Issues (2008) Independent Living. A cross-government strategy about independent living for disabled people. London: HM Government.
Perkins, R. & Slade, M. (2012) Recovery in England: Transforming statutory services? International Review of Psychiatry, 24(1): 29–39
Perkins, R. (2012) UK mental health policy development: A counter-argument deriving from users’ experiences. In Phillips, P., Sandford, T. & Johnston, C. (Eds) Working in Mental Health: Practice and Policy in a Changing Environment. Oxford: Routledge.
Perkins, R. & Goddard, K. (2008) Sharing responsibility for risk and risk-taking. Module 5 in NHS Education for Scotland Realising Recovery Learning Materials, NHS Scotland (see www.nes.scot.nhs.uk/mentalhealth)
Prime Minister’s Strategy Unit (2005) Improving the Life Chances of Disabled People. London: Cabinet Office.
Repper, J. & Perkins, R. (2003) Social Inclusion and Recovery. London: Balliere Tindall.
Repper, J. & Perkins, R. (2012) Recovery: A journey of discovery for individuals and services. In Phillips, P., Sandford, T. & Johnston, C. (Eds) Working in Mental Health: Practice and Policy in a Changing Environment. Oxford: Routledge.
Scott-Moncrieff, L., Briscoe, J. & Daniels, G. (2009) An independent investigation into the care and treatment of Daniel Gonzales. NHS South East Coast and Surrey County Council
Shepherd, G., Boardman, J. & Slade, M. (2008) Making Recovery a Reality. London: Sainsbury Centre for Mental Health.
Think Local Act Personal (2011) Response to the Department of Health’s Caring for our Future Engagement Programme. London: Think Local Act Personal Partnership
Recovery Colleges can revolutionise mental health services and help people to fulfil their potential.
They deliver comprehensive, peer-led education and training programmes within mental health services. They should be run like any other college, providing education as a route to Recovery, not as a form of therapy with courses co-devised and co-delivered by people with lived experience of mental illness and by mental health professionals.
1. Recovery Colleges
Rachel Perkins, Julie Repper, Miles Rinaldi and Helen Brown
Introduction
Recovery is a personal journey of discovery (Repper & Perkins, 2012). It involves making sense of, and finding meaning in, what has happened; becoming an expert in your own self-care; building a new sense of self and purpose in life; discovering your own resourcefulness and possibilities and using these, and the resources available to you, to pursue your aspirations and goals.
The challenge for mental health services is to assist people in this journey (Shepherd, Boardmam & Slade, 2008). This requires us to move beyond a narrow focus on symptom reduction to helping people to rebuild lives that they find satisfying, meaningful and valued (Repper & Perkins, 2003; Perkins, 2012; Perkins & Slade, 2012). This change is reflected in the mental health strategy ‘No Health Without Mental Health’ (Department of Health, 2011) which defines key outcomes as enabling people to gain:
“a greater ability to manage their own lives, stronger social relationships, a greater sense of purpose, the skills they need for living and working, improved chances in education, better employment rates and a suitable and stable place to live”.
If services are to assist people in achieving these outcomes, major cultural and organisational changes are required. Shepherd, Boardman and Burns (2010) identify ‘ten key organisational challenges’ ranging from changes in the quality of day-to-day relationships to management and leadership. These essentially involve:
- A redefinition of the purpose of services from reducing symptoms to rebuilding lives. Everything that we do must be judged in terms of the extent to which it helps people in their recovery journey.
- A change in the role of mental health professionals and professional expertise, moving from being ‘on top’ to being ‘on tap’: not defining problems and prescribing treatments, but rather making their expertise and understandings available to those who may find them useful.
- A recognition of the equal importance of both ‘professional expertise’ and ‘lived experience’ and a breaking down of the barriers that divide ‘them’ from ‘us’. This must be reflected in a different kind of workforce (one that includes peer workers), and different working practices founded on co-production and shared decision making at all levels.
- A different relationship between services and the communities that they serve. Enabling both individuals and communities to recognise their own resources and resourcefulness and recreating communities that can accommodate human distress.
In this paper we will argue that a Recovery College (alternatively called a Recovery Education Centre) embodies these transformations and is therefore central to driving recovery-focused organisational change. It uses an educational paradigm to complement traditional treatment approaches (Ashcraft & Anthony, 2005).
“We decided to use education as the model for approaching recovery, rather than develop more traditional alternatives. We did this because we want our center to be about reinforcing and developing people’s strengths rather than adding to the attention on what is wrong with them. The guiding vision we had for the Recovery Education Center is reflected in the mission statement: people will discover who they are, learn skills and tools to promote recovery, find out what they can be, and realise the unique contribution they have to offer.” (Ashcraft, 2000).
The move from a therapeutic to an educational approach carries with it a number of core changes in focus and relationships that are central to promoting recovery. These are summarised in Table 1.
Table 1 – Therapy and Education
A therapeutic approach
- Focuses on problems, deficits and dysfunctions;
- Strays beyond formal therapy sessions and becomes the over-arching paradigm;
- Transforms all activities into therapies – work therapy, gardening therapy etc;
- Problems are defined, and the type of therapy is chosen, by the professional ‘expert’;
- Maintains the power imbalances and reinforces the belief that all expertise lies with the professionals.
An educational approach
- Helps people recognise and make use of their talents and resources;
- Assists people in exploring their possibilities and developing their skills;
- Supports people to achieve their goals and ambitions;
- Staff become coaches who help people find their own solutions;
- Students choose their own courses, work out ways of making sense of (and finding meaning in) what has happened and become experts in managing their own lives.
Specialist assessment and treatment are important, but they represent only a small part of what mental health services do and far more is required if people are to participate as equal citizens in economic, social and family life and do the things they value. An educational approach focuses on developing people’s strengths, and enabling them to understand their own challenges and how they can best manage these in order to pursue their aspirations. It facilitates the learning of skills that promote recovery and underpins greater confidence and the self-belief that comes with recognising your abilities and potential. We would argue that within a genuinely recovery-focused service a large part of what has traditionally been provided in the form of ‘individual work’ or ‘groups’ might be better framed within an educational paradigm and provided within a Recovery College.
Recovery Education Centres have been central to the development of recovery-focused services in the USA, such as those in Boston, Massachusetts and Phoenix, Arizona, and are now emerging in England based on the pioneering Recovery Colleges established in South West London in 2009 (www.swlstgtr.nhs.uk) and Nottingham in 2011 (www. nottinghamshirehealthcaretrust.nhs.uk). A film about the Recovery College in South West London can be viewed at www.youtube.com/ watch?V=VSOeQbkMVqc.
Defining features of a Recovery College
While Recovery Colleges vary, their power to transform both services and the lives of the individuals whom they serve rests on eight defining features.
1. Co-production between people with personal and professional experience of mental health problems
There should be co-production at every level and every stage, from initial planning and development, to decisions about operation, curriculum and quality assurance. Co-production of courses with local organisations – like colleges, the police, employment services, housing providers and debt advisors – is also important as is working in partnership with staff ‘Learning and Development’ departments.
In Nottingham, a Recovery College student with a background in special needs education brought skills used in his former career to work with mental health practitioners and other peers to develop ‘differentiation’ guidance for teaching groups of students with mixed needs and abilities and provided associated training for college tutors.
In the process of developing a Recovery College in Central and North West London, a group of prospective peer and peer carer trainers met with key mental health practitioners to agree an initial set of courses that would be offered. These were then drafted by pairs of peer and mental health practitioners in line with their interests and expertise. For example, one peer trainer had conducted research into self-harm and led the development of a workshop in this area. Peer trainers in South West London emphasised the importance and value of this co-production:
“Who can argue against the power of collaboration between clinician and peer when you see with your own eyes people living their dreams and having hope because of it? It just makes the job so rewarding.”
“We learn from each other and we inspire each other to help our students on their road to recovery. You see the positive change in students – becoming the people they want to be.”
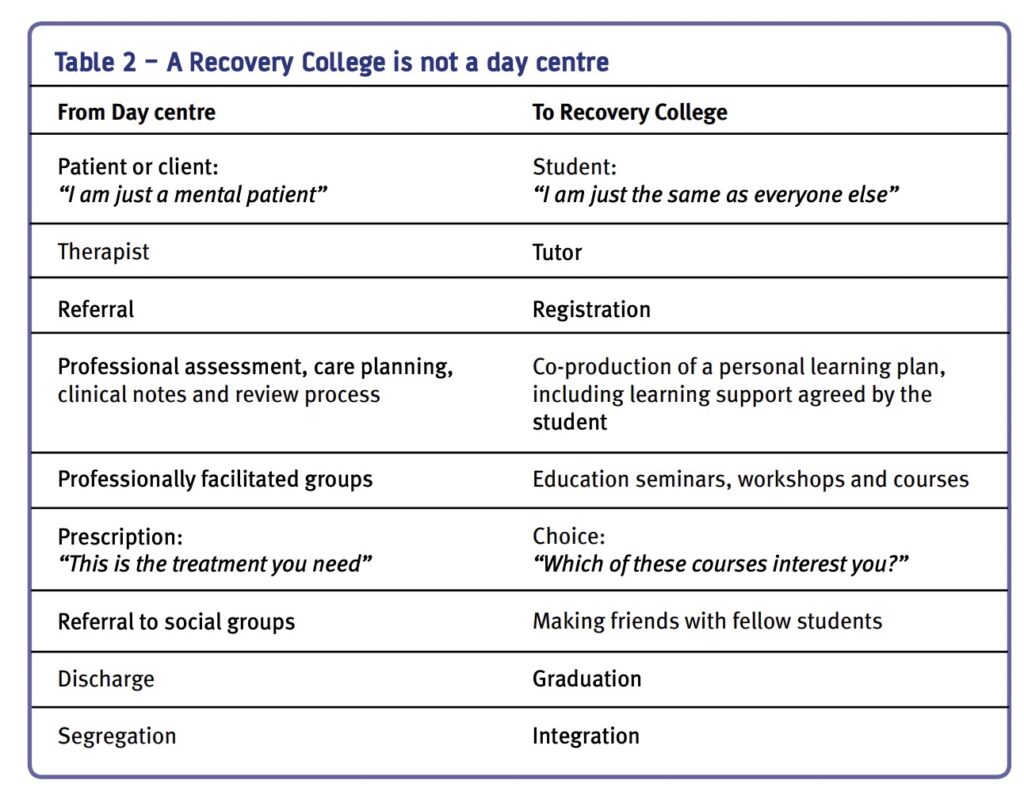
2. There is a physical base (building) with classrooms and a library where people can do their own research
A physical base is a tangible representation of commitment to the model. However, a ‘hub and spoke’ approach, with satellite courses in different locations, is often necessary to ensure access for all those who want it. The recovery library is not a substitute for the local library, but should contain recovery materials (books, self-help materials, personal stories, DVDs etc.) and computers so that people can find out things for themselves by accessing the internet. As well as providing important resources for both staff and peers, the library enables people to come and see what is available and familiarise themselves with the service prior to enrolling on courses.
“I appreciate the wide range of self-help literature in the library.”
“What an Aladdin’s cave – I just wanted to spend a month in the library going through all the books and information packs.”
3. It operates on college principles
The College is not a day centre (see Table 2), nor does it offer treatment or co-ordination of care. Students select courses from a prospectus, they are not told what is good for them. Selection is not based on diagnosis or clinical condition, neither are risk assessments conducted by the college to see if they are ‘suitable’ to attend. As in any college, a ‘student charter’ describes what the person can expect to gain and what the College can expect from them in terms of attendance and behaviour.
4. It is for everyone
People with mental health problems, families, carers, staff from mental health service providers and people from partner agencies can all attend courses.The ethos of the Colleges is that they are open to everyone and most do not turn away anyone who has an interest.
“Thank you for meeting with me and my mum. You were very kind, and it’s such a help to know that you at the Recovery College are there for us and for my brother.”
5. There is a Personal Tutor (or equivalent) who offers information, advice and guidance
The ‘tutor’ helps students select the courses that suit them and develop individual learning plans based on their hopes and aspirations, to increase their knowledge and understanding, as well as to move on to possibilities in the community.
“[The tutor] made me realise I could do it. Helped me to work out what courses might help me achieve my goals.”
6. The College is not a substitute for traditional assessment and treatment
A Recovery College complements specialist, technical assessment and treatment by helping people to understand their problems and learn how to manage these better in order to pursue their aspirations. It is a place where ‘lived experience’ is blended with the expertise of mental health practitioners.
“Keeping a journal has helped me to take stock of my life and also provide a record of when I feel ill that I can show to my psychiatrist.”
7. It is not a substitute for mainstream colleges
If it is to promote participation and citizenship the College should not substitute for the general education and opportunities offered by local educational establishments. It can, however, provide a route on to mainstream education via, for example, ‘return to study’ courses.
“ I have gone to college and am now awaiting results for A-level English.”
8. It must reflect recovery principles in all aspects of its culture and operation
In this context the welcome provided, the messages conveyed by the physical environment and the language used are all important: language conveys strong messages about role, purpose, status and value. The messages should be of hope, empowerment, possibility and aspirations. Rather than highlighting deficits, problems and shortcomings, practices should all ensure that success is celebrated both with students (in the form of certificates of achievement) and in the working practices of College staff.
In Nottingham, the Recovery College team finish the week by taking stock and marking achievements. They meet every Friday afternoon over tea and cakes to share success stories, examples of positive feedback and creative ideas they have come across during the week so that they always finish on a ‘high note’.
Developing a College and its curriculum
Recovery Colleges are co-produced in local partnerships. The provision of a range of different courses, seminars and workshops allow them to cater for people with diverse needs and preferences. Some people may want to dip in to specific courses, others may wish to construct for themselves a more comprehensive programme. Some people may ‘put their toe in the water’ with a single session that interests them and then move on to longer courses. The range of courses is determined by those who wish to attend them.
Most Colleges start by bringing together groups of peers and staff to develop an initial prospectus that is then augmented according to the suggestions and requests of students and trainers. Experience suggests that these cluster around five areas:
Understanding mental health issues and treatment options
Some of these courses are single sessions providing an introduction to specific challenges like psychosis, depression, self-harm, substance misuse, dementia and eating disorders. Some provide a more general introduction to the range of mental health difficulties, while others introduce people to the range of treatment options available, for example the range of different sorts of psychological therapies and medication.
Rebuilding life with mental health challenges
These courses range from one day introductions to recovery to longer courses that enable people to develop their own recovery plans and tell their own story. A range of self-management programmes for specific mental health conditions are offered (for example, living with bipolar disorder, coping with depression and anxiety management) as well as courses that help people to look after their physical health care and wellbeing (healthy eating, diet, exercise etc.). Other courses that address particular challenges can be added, such as ‘getting a good night’s sleep’, ‘anger management’, ‘becoming more assertive’, ‘coping with stress’ and ‘problem-solving’. Some of the most popular courses include ‘life coaching and goal setting for recovery’, ‘mindfulness’, ‘pursuing your dreams and ambitions’ and ‘spirituality and mental health’.
Developing life skills
These courses tend to fall broadly into two areas. First, there are courses that assist people to rebuild their lives outside services, such as: ‘managing a budget’, ‘managing your tenancy’, ‘looking after your personal safety’, ‘getting e-connected’ and ‘returning to work or study’. Second, there are courses that focus on getting the most out of services: for example, ‘getting the best from your ward round or care review’, ‘understanding the Mental Health Act and mental health review tribunals’ or ‘making a complaint’.
Capacity building among the peer workforce
Recovery Colleges provide courses that drive changes across the service by training peer support workers and peer trainers and providing courses that enable people with lived experience to participate in staff selection and training or sit on committees. The skills and confidence that people gain in these courses are useful not only within services, but are also transferrable to opportunities and employment outside services.
Family and friends
Some courses specifically focus on the challenges faced by people who provide care and support for family members and friends with mental health conditions. These are often attended by the individual and their relatives and assist the whole family to live with the challenges they face. This opportunity for families to learn together has proved particularly popular.
All Colleges produce an attractive prospectus for potential students detailing the courses provided. While staff may inform the people they serve about the College and help them to explore the possibilities there, people are not ‘referred’. Individual students enrol and register on the courses that interest them. The Colleges in Nottingham and South West London have grown rapidly, driven by popular demand and it has been difficult to keep pace with demand for courses. In terms of staffing:
- The South West London Recovery College – opened with a core staff complement of one full-time mental health practitioner and four part-time peer trainers providing eight pilot courses with some sessional input from staff in other teams within the organisation. By 2010 it offered 52 courses in 11 locations serving around 50 people per day. A total of 1350 different people used the College in its first year of operation.
- The Nottingham Recovery College started with a core staff complement of one fulltime mental health practitioner and 12 courses run by four sessional peer and sessional staff trainers drawn from other teams within Notttinghamshire Healthcare NHS Trust. In its third term the College offered 101 courses spanning 45 different topics, running in eight locations.
The evidence base
A core component of Recovery Colleges is helping people to become experts in their own self-care. There is now a considerable body of evidence demonstrating the effectiveness of supported self-management education in health conditions of all types (Rinaldi, 2002; Foster et al., 2007; Cook et al., 2011). An educational approach which brings together the expertise of professional and lived experience also lies at heart of the ‘expert patient programmes’ that have proved so useful in relation to a range of long term health conditions (Department of Health, 2001; 2006; Lawn et al., 2007). Supporting self-management is now defined by National Institute for health and clinical excellence (NICE) as a key quality standard of adult mental health services, as part of the service user experience guidance (2011).
A wealth of evidence demonstrates the effectiveness of peer support within mental health services (Repper & Carter, 2011) and Recovery Colleges offer peer support from both peer trainers and fellow students.
Recovery Colleges are still in their infancy in this country so the evaluative evidence is limited. However, they have certainly proved very popular among those who use them:
“I wouldn’t be here if it wasn’t for the College.”
“What a positive and helpful approach. This type of course should have started years ago.”
“Extremely informative… it has given me further insight into myself and my thinking.”
“I can study in a safe place so I don’t have to worry if it goes pear-shaped if I get unwell – I can be safe learning.”
“It’s like the sun coming out to go into the Recovery College… it’s a wonderful proclamation of service users (and carers) being of value.”
Prior to the establishment of the South West London Recovery College, a pilot study was conducted comprising four recovery courses co-delivered by mental health practitioners and peer trainers (Rinaldi, Wybourn & Clenahan, in press). On average, students had been using mental health services for six years and 45% had a diagnosis of psychosis. Students were enthusiastic about the courses, with an 18 month follow-up showing:
- the majority (68%) felt more hopeful for the future than they had at the start of their course, most (81%) had developed their own plan for managing their problems and staying well; and 70% had become mainstream students, gained employment or become a volunteer;
- compared with those who did not attend courses, those who attended more than 70% of their scheduled sessions (67% of those who started) showed a significant reduction in use of community mental health services.
The comments made by students at Nottingham and South West London Colleges reinforce these findings:
“I have moved further in my recovery in one term here than in the past two years in the team.”
“I’ve halved my medication and learned lots of different ways to manage my anxiety.”
“I can’t believe what you have done for my son. I used to have to push him out of the door and he would cover his face. Now he goes out with his head held high.”
A survey of community mental health team care co-ordinators conducted one year after the establishment of the South West London Recovery College (Rinaldi & Suleman, 2012) showed that the majority (66%) had people on their caseload who had attended the College and they considered that people had benefited greatly from their attendance. In comparison with those who had no-one on their caseload who had attended the College, care co-ordinators who supported people who had used the College placed a higher value on self-management, were more comfortable about supporting them in these endeavours, and had higher expectations for those whom they served. Their comments included:
“I have a strong belief that service users have inner strengths, skills and resources and, with the right support ,such as courses at the Recovery College, can become experts in their own health and wellbeing and rebuild their lives.”
“Self-management is an integral part of my own approach which aims to foster independence, increased self-reliance, and the service user’s sense of responsibility for their own life outcomes.”
The transformative power of the Recovery College
The power of Recovery Colleges is two-fold. First, they assist the individuals whom they serve in their personal and collective journeys of recovery. Second, they assist organisations and services to become more recovery-focused. The creation of recovery-focused services requires a major transformation in purpose and relationships: a focus on rebuilding lives rather than reducing symptoms alone and a partnership between equals, rather than ‘experts’ and ‘patients’.
Recovery Colleges embody and drive these transformations in a number of ways:
1. They enable people to become experts in their own self-care and develop the skills they need for living and working
Recovery Colleges enable people to become experts in their own self-care and develop skills and confidence to manage their own recovery journey.
2. They explicitly recognise the expertise of mental health professionals and the expertise of lived experience in a process of ‘co-production’
A Recovery College is run by both peer trainers and mental health practitioner trainers. All courses are co-produced, co-delivered and co-received by staff, people with mental health problems and the people who are close to them.
3. They break down the destructive barriers between ‘them’ and ‘us’ that perpetuate stigma and exclusion
Co-produced, co-delivered courses enable students to see what people with mental health problems can achieve. Trainers are both people with lived experience and mental health practitioners (who may themselves have lived experience of subjects in which they provide training) and they are employed on equal terms. Barriers between ‘them’ and ‘us’ are not only broken down in the provision of courses, they are also broken down within the student group. People with lived experience and those who provide their support (both informal carers and mental health practitioners) learn together and from each other. The transformation from ‘service user’ to ‘student’ affords a positive identity beyond that of ‘mental patient’.
4. They provide peer support
In Recovery Colleges the peer support offered by peer trainers and fellow students enables people to feel less alone, offers images of hope and possibility and allows people to learn from others who have faced similar challenges and use their lived experience to help others.
5. Group learning and mutual support replaces the disabling isolation engendered by a sole reliance on individual work
Recovery Colleges create a network of social opportunities among peers and the general community which can reduce the social isolation that so many people experience. Like any students, people attending Recovery College courses often form relationships that extend beyond the classroom.
6. They afford choice, control and self-determination Students are not passive recipients of the ‘prescriptions’ of experts.
Within a Recovery College there are no prescriptions: students select the courses that interest them from a prospectus, do their own research in a library, and attend courses that enable them to take control and pursue what is important to them.
7. They promote participation in the local community A Recovery College achieves this in three ways.
First, people from local organisations can be involved in providing courses. Second, individuals can attend courses that assist them to develop the knowledge and skills necessary to return to work, study, and participate in the community. Third, people with a diagnosis of a mental health condition study alongside their relatives, friends and neighbours.
From margins to mainstream
Many services are in the process of developing Recovery Colleges, however, they remain ‘pilot’ services. Their full transformative power cannot be fully realised until they move from being a novel, marginal addition to being a central component of recovery-focused services.
For individuals, the research literature demonstrates the importance of ensuring that self-management education is fully integrated into healthcare systems and that learning is reinforced by all professionals with whom the person has contact (Coulter, 2011; Protheroe, Rogers & Kennedy, 2008; Pulvirenti, McMillan & Lawn, 2011). Similarly, if people are to take control over their lives and pursue their aspirations it is important that the confidence, skills and insights they gain from the Recovery College are not undermined by experiences with other parts of the mental health service.
For services and organisations, the Recovery College must become a core driver for whole system change. This can be achieved in three ways. First, they are able to model different relationships between people using services and mental health practitioners. Second, they can identify and prepare people with lived experience for employment as peer workers across the service. And third, they may replace some elements of existing services. These elements can make a Recovery College a high impact development with a major ‘domino effect’ across a mental health service over time.
Colleges cannot, of course, replace all specialist assessment and treatment or non-specialist outreach support. But mental health services try to provide a great deal more than this in the form of information, advice on self-management and support in day-to-day life for both individuals and their families – all delivered, almost exclusively, on an individual basis. The opportunity to reduce costs and provide services in the form of co-produced seminars and courses that decrease isolation and increase peer support, while at the same time offering a broad range of professional expertise, therefore has the potential to deliver a ‘win-win’ situation – better services at lower cost.
A note on authorship
Advances in recovery-focused practice have arisen from collaborative partnerships between a number of individuals and organisations. The Implementing Recovery through Organisational Change (ImROC) briefing papers draw upon this work. Where ideas are taken from published materials we cite them in the conventional form, but we also want to acknowledge the many unpublished discussions and conversations that have informed the creative development of the project as a whole over the last five years. Each paper in this series is written by those members of the project team best placed to lead on the topic, together with invited guest authors and contributions from other team members. We particularly wish to acknowledge the contribution of those whose work on the practical implementation of recovery values has formed the testbed for many of the ideas. Without these pioneers, there would be nothing to write about.
References
Ashcraft, L. (2000) META Services recovery education center business plan. Phoenix Arizona: META Services Inc.
Ashcraft, L. & Anthony, W. (2005) A story of transformation, Behavioral Healthcare Tomorrow, April, 12-22
Cook, J.A., Copeland, M.E., Jonikas, J.A., et al. (2011) Results of a randomised controlled trial of mental illness self-management using wellness recovery action planning. Schizophrenia Bulletin doi: 10.1093/schbul/sbr012
Coulter, A. (2011) Engaging patients in healthcare. Maidenhead: Open University Press.
Department of Health (2001) The Expert Patient: A new approach to chronic disease management for the 21st century. Department of Health: London
Department of Health (2006) Supporting people with long-term conditions to self-care: A guide to developing local strategies and good practice.
Department of Health: London Department of Health (2011) No Health Without Mental Health: A Cross-Government Mental Health Outcomes Strategy for People of All Ages. London: HM Government
Foster, G., Taylor, S, J, C., Eldridge, S. Ransay, J. & Griffiths, C.J. (2007) Self-management education programmes by lay leaders for people with chronic conditions. Cochrane database of Systematic Reviews Issue 4. Art. No.: CD005108.
Lawn, S., Battersby, M. W., Pols, R. G., Lawrence, J., Parry, T., & Urukalo, M. (2007). The mental health expert patient: Findings from a pilot study of a generic chronic condition self-management programme for people with mental illness. International Journal of Social Psychiatry, 53(1), 63-74
National Institute for Health and Clinical Excellence (2011) Service user experience in adult mental health: improving the experience of care for people using adult NHS mental health services, NICE clinical guideline 136 www.nice. org.uk/cg136
Perkins, R. (2012) UK mental health policy development – An alternative view, in Phillips, P., Sandford, T. and Johnston, C. (eds) Working in Mental Health: Practice and Policy in a Changing Environment, Oxford: Routledge
Perkins, R. & Slade, M. (2012) Recovery in England: Transforming statutory services? International Review of Psychiatry, 24(1), 29-39
Protheroe, J. Rogers, A., Kennedy, AP., et al. (2008) Promoting patient engagement with selfmanagement support information: a qualitative meta-synthesis of processes influencing uptake. Implementation Science. 3, 44.
Pulvirenti, M., McMillan, J., Lawn, S. (2011) Empowerment, patient centred care and selfmanagement. Heath Expectations. Doi:10.1111/ j.1369-7625.2011.00757.x.
Repper, J. & Perkins, R. (2003) Recovery and Social Inclusion, London: Balliere Tindall
Repper, J. & Carter, T. (2011) A review of the literature on peer support in mental health services, Journal of Mental Health, 20(4): 392–411
Repper, J. & Perkins, R. (2012) Recovery: A journey of discovery for individuals and services, in Phillips, P., Sandford, T, & Johnston, C. (Ed) Working in Mental Health: Practice and policy in a changing environment, Oxford: Routledge
Rinaldi, M. (2002) Manic depression and self management, in Ramsey, R., Page, A., Goodman, T. & Hart, D. (Eds.). Changing Minds: Our Lives and Mental Illness. London: Gaskell
Rinaldi, M. & Suleman, M. (2012) Care co-ordinators attitudes to self-management and their experience of the use of the South West London Recovery College, London: South West London and St George’s Mental Health NHS Trust
Rinaldi, M., Wybourn, S. & Clenahan, M. (in press) The development, piloting and outcomes from a Recovery College in England, Psychiatric Rehabilitation Journal
Shepherd, G., Boardman, J. & Slade, M. (2008) Making Recovery a Reality. London: Sainsbury Centre for Mental Health
Shepherd, G., Boardman, J. & Burns, M. (2010) Implementing Recovery: a methodology for organisational change, London: Sainsbury Centre for Mental Health
In Nigeria ImROC is a current co-applicant in a HOPE study that will commence in 2022 This project is about developing peer workers to support homeless people in Nigeria in partnership with Kings College London.
In Kenya ImROC is a current co-applicant in a HOPE study that will commence in 2022. This project is about developing peer workers to support homeless people in Kenya in partnership with Kings College London.
In Ethiopia ImROC is a current co-applicant in a HOPE study that will commence in 2022 and continue through 2023/24. This project is about developing peer workers to support homeless people in Ethiopia in partnership with Kings College London.
ImROC has a close working relationship with Norwegian services in Stavangar, Bergan and Oslo. Norway is currently represented by Miles Rinaldi (ImROC Consultant) in the current ImROC work-stream forming and supporting the International Peer Leadership Qualification.
Get In Touch
We would love to hear more about your project. Please fill out this form and we will get back to you.
imroc@imroc.orgImROC Head Office PO Box 11115 Nottingham NG14 6UZ
