Recovery Colleges can revolutionise mental health services and help people to fulfil their potential.
They deliver comprehensive, peer-led education and training programmes within mental health services. They should be run like any other college, providing education as a route to Recovery, not as a form of therapy with courses co-devised and co-delivered by people with lived experience of mental illness and by mental health professionals.
1. Recovery Colleges
Rachel Perkins, Julie Repper, Miles Rinaldi and Helen Brown
Introduction
Recovery is a personal journey of discovery (Repper & Perkins, 2012). It involves making sense of, and finding meaning in, what has happened; becoming an expert in your own self-care; building a new sense of self and purpose in life; discovering your own resourcefulness and possibilities and using these, and the resources available to you, to pursue your aspirations and goals.
The challenge for mental health services is to assist people in this journey (Shepherd, Boardmam & Slade, 2008). This requires us to move beyond a narrow focus on symptom reduction to helping people to rebuild lives that they find satisfying, meaningful and valued (Repper & Perkins, 2003; Perkins, 2012; Perkins & Slade, 2012). This change is reflected in the mental health strategy ‘No Health Without Mental Health’ (Department of Health, 2011) which defines key outcomes as enabling people to gain:
“a greater ability to manage their own lives, stronger social relationships, a greater sense of purpose, the skills they need for living and working, improved chances in education, better employment rates and a suitable and stable place to live”.
If services are to assist people in achieving these outcomes, major cultural and organisational changes are required. Shepherd, Boardman and Burns (2010) identify ‘ten key organisational challenges’ ranging from changes in the quality of day-to-day relationships to management and leadership. These essentially involve:
- A redefinition of the purpose of services from reducing symptoms to rebuilding lives. Everything that we do must be judged in terms of the extent to which it helps people in their recovery journey.
- A change in the role of mental health professionals and professional expertise, moving from being ‘on top’ to being ‘on tap’: not defining problems and prescribing treatments, but rather making their expertise and understandings available to those who may find them useful.
- A recognition of the equal importance of both ‘professional expertise’ and ‘lived experience’ and a breaking down of the barriers that divide ‘them’ from ‘us’. This must be reflected in a different kind of workforce (one that includes peer workers), and different working practices founded on co-production and shared decision making at all levels.
- A different relationship between services and the communities that they serve. Enabling both individuals and communities to recognise their own resources and resourcefulness and recreating communities that can accommodate human distress.
In this paper we will argue that a Recovery College (alternatively called a Recovery Education Centre) embodies these transformations and is therefore central to driving recovery-focused organisational change. It uses an educational paradigm to complement traditional treatment approaches (Ashcraft & Anthony, 2005).
“We decided to use education as the model for approaching recovery, rather than develop more traditional alternatives. We did this because we want our center to be about reinforcing and developing people’s strengths rather than adding to the attention on what is wrong with them. The guiding vision we had for the Recovery Education Center is reflected in the mission statement: people will discover who they are, learn skills and tools to promote recovery, find out what they can be, and realise the unique contribution they have to offer.” (Ashcraft, 2000).
The move from a therapeutic to an educational approach carries with it a number of core changes in focus and relationships that are central to promoting recovery. These are summarised in Table 1.
Table 1 – Therapy and Education
A therapeutic approach
- Focuses on problems, deficits and dysfunctions;
- Strays beyond formal therapy sessions and becomes the over-arching paradigm;
- Transforms all activities into therapies – work therapy, gardening therapy etc;
- Problems are defined, and the type of therapy is chosen, by the professional ‘expert’;
- Maintains the power imbalances and reinforces the belief that all expertise lies with the professionals.
An educational approach
- Helps people recognise and make use of their talents and resources;
- Assists people in exploring their possibilities and developing their skills;
- Supports people to achieve their goals and ambitions;
- Staff become coaches who help people find their own solutions;
- Students choose their own courses, work out ways of making sense of (and finding meaning in) what has happened and become experts in managing their own lives.
Specialist assessment and treatment are important, but they represent only a small part of what mental health services do and far more is required if people are to participate as equal citizens in economic, social and family life and do the things they value. An educational approach focuses on developing people’s strengths, and enabling them to understand their own challenges and how they can best manage these in order to pursue their aspirations. It facilitates the learning of skills that promote recovery and underpins greater confidence and the self-belief that comes with recognising your abilities and potential. We would argue that within a genuinely recovery-focused service a large part of what has traditionally been provided in the form of ‘individual work’ or ‘groups’ might be better framed within an educational paradigm and provided within a Recovery College.
Recovery Education Centres have been central to the development of recovery-focused services in the USA, such as those in Boston, Massachusetts and Phoenix, Arizona, and are now emerging in England based on the pioneering Recovery Colleges established in South West London in 2009 (www.swlstgtr.nhs.uk) and Nottingham in 2011 (www. nottinghamshirehealthcaretrust.nhs.uk). A film about the Recovery College in South West London can be viewed at www.youtube.com/ watch?V=VSOeQbkMVqc.
Defining features of a Recovery College
While Recovery Colleges vary, their power to transform both services and the lives of the individuals whom they serve rests on eight defining features.
1. Co-production between people with personal and professional experience of mental health problems
There should be co-production at every level and every stage, from initial planning and development, to decisions about operation, curriculum and quality assurance. Co-production of courses with local organisations – like colleges, the police, employment services, housing providers and debt advisors – is also important as is working in partnership with staff ‘Learning and Development’ departments.
In Nottingham, a Recovery College student with a background in special needs education brought skills used in his former career to work with mental health practitioners and other peers to develop ‘differentiation’ guidance for teaching groups of students with mixed needs and abilities and provided associated training for college tutors.
In the process of developing a Recovery College in Central and North West London, a group of prospective peer and peer carer trainers met with key mental health practitioners to agree an initial set of courses that would be offered. These were then drafted by pairs of peer and mental health practitioners in line with their interests and expertise. For example, one peer trainer had conducted research into self-harm and led the development of a workshop in this area. Peer trainers in South West London emphasised the importance and value of this co-production:
“Who can argue against the power of collaboration between clinician and peer when you see with your own eyes people living their dreams and having hope because of it? It just makes the job so rewarding.”
“We learn from each other and we inspire each other to help our students on their road to recovery. You see the positive change in students – becoming the people they want to be.”
2. There is a physical base (building) with classrooms and a library where people can do their own research
A physical base is a tangible representation of commitment to the model. However, a ‘hub and spoke’ approach, with satellite courses in different locations, is often necessary to ensure access for all those who want it. The recovery library is not a substitute for the local library, but should contain recovery materials (books, self-help materials, personal stories, DVDs etc.) and computers so that people can find out things for themselves by accessing the internet. As well as providing important resources for both staff and peers, the library enables people to come and see what is available and familiarise themselves with the service prior to enrolling on courses.
“I appreciate the wide range of self-help literature in the library.”
“What an Aladdin’s cave – I just wanted to spend a month in the library going through all the books and information packs.”
3. It operates on college principles
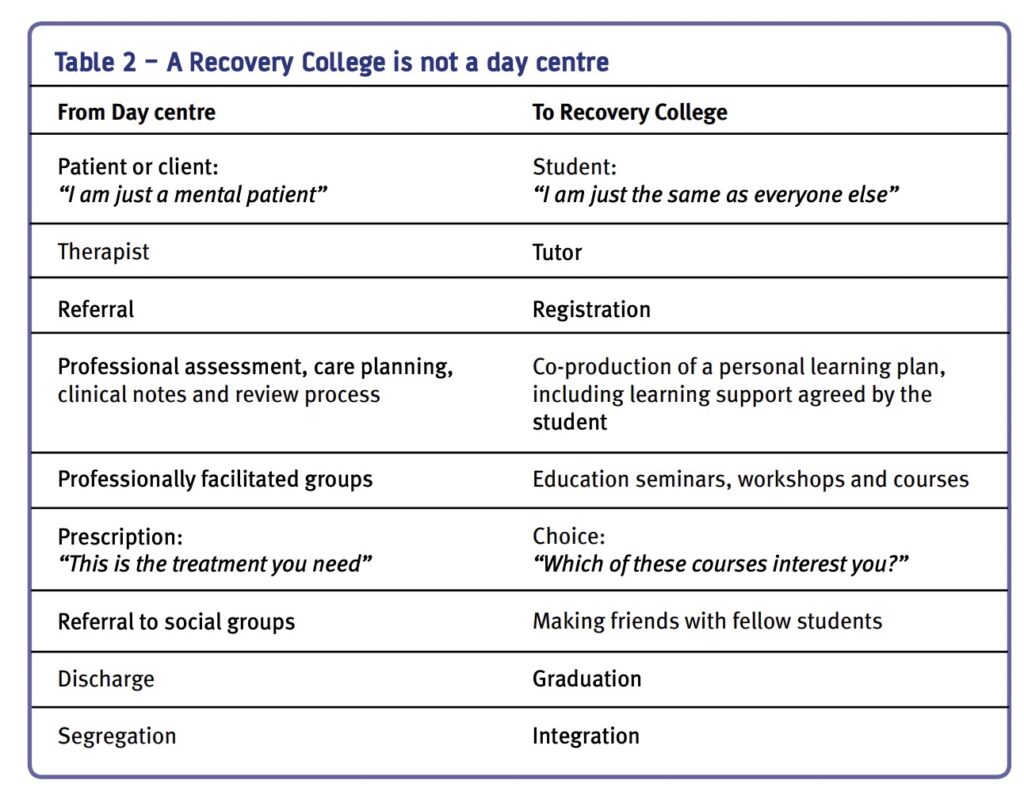
The College is not a day centre (see Table 2), nor does it offer treatment or co-ordination of care. Students select courses from a prospectus, they are not told what is good for them. Selection is not based on diagnosis or clinical condition, neither are risk assessments conducted by the college to see if they are ‘suitable’ to attend. As in any college, a ‘student charter’ describes what the person can expect to gain and what the College can expect from them in terms of attendance and behaviour.
4. It is for everyone
People with mental health problems, families, carers, staff from mental health service providers and people from partner agencies can all attend courses.The ethos of the Colleges is that they are open to everyone and most do not turn away anyone who has an interest.
“Thank you for meeting with me and my mum. You were very kind, and it’s such a help to know that you at the Recovery College are there for us and for my brother.”
5. There is a Personal Tutor (or equivalent) who offers information, advice and guidance
The ‘tutor’ helps students select the courses that suit them and develop individual learning plans based on their hopes and aspirations, to increase their knowledge and understanding, as well as to move on to possibilities in the community.
“[The tutor] made me realise I could do it. Helped me to work out what courses might help me achieve my goals.”
6. The College is not a substitute for traditional assessment and treatment
A Recovery College complements specialist, technical assessment and treatment by helping people to understand their problems and learn how to manage these better in order to pursue their aspirations. It is a place where ‘lived experience’ is blended with the expertise of mental health practitioners.
“Keeping a journal has helped me to take stock of my life and also provide a record of when I feel ill that I can show to my psychiatrist.”
7. It is not a substitute for mainstream colleges
If it is to promote participation and citizenship the College should not substitute for the general education and opportunities offered by local educational establishments. It can, however, provide a route on to mainstream education via, for example, ‘return to study’ courses.
“ I have gone to college and am now awaiting results for A-level English.”
8. It must reflect recovery principles in all aspects of its culture and operation
In this context the welcome provided, the messages conveyed by the physical environment and the language used are all important: language conveys strong messages about role, purpose, status and value. The messages should be of hope, empowerment, possibility and aspirations. Rather than highlighting deficits, problems and shortcomings, practices should all ensure that success is celebrated both with students (in the form of certificates of achievement) and in the working practices of College staff.
In Nottingham, the Recovery College team finish the week by taking stock and marking achievements. They meet every Friday afternoon over tea and cakes to share success stories, examples of positive feedback and creative ideas they have come across during the week so that they always finish on a ‘high note’.
Developing a College and its curriculum
Recovery Colleges are co-produced in local partnerships. The provision of a range of different courses, seminars and workshops allow them to cater for people with diverse needs and preferences. Some people may want to dip in to specific courses, others may wish to construct for themselves a more comprehensive programme. Some people may ‘put their toe in the water’ with a single session that interests them and then move on to longer courses. The range of courses is determined by those who wish to attend them.
Most Colleges start by bringing together groups of peers and staff to develop an initial prospectus that is then augmented according to the suggestions and requests of students and trainers. Experience suggests that these cluster around five areas:
Understanding mental health issues and treatment options
Some of these courses are single sessions providing an introduction to specific challenges like psychosis, depression, self-harm, substance misuse, dementia and eating disorders. Some provide a more general introduction to the range of mental health difficulties, while others introduce people to the range of treatment options available, for example the range of different sorts of psychological therapies and medication.
Rebuilding life with mental health challenges
These courses range from one day introductions to recovery to longer courses that enable people to develop their own recovery plans and tell their own story. A range of self-management programmes for specific mental health conditions are offered (for example, living with bipolar disorder, coping with depression and anxiety management) as well as courses that help people to look after their physical health care and wellbeing (healthy eating, diet, exercise etc.). Other courses that address particular challenges can be added, such as ‘getting a good night’s sleep’, ‘anger management’, ‘becoming more assertive’, ‘coping with stress’ and ‘problem-solving’. Some of the most popular courses include ‘life coaching and goal setting for recovery’, ‘mindfulness’, ‘pursuing your dreams and ambitions’ and ‘spirituality and mental health’.
Developing life skills
These courses tend to fall broadly into two areas. First, there are courses that assist people to rebuild their lives outside services, such as: ‘managing a budget’, ‘managing your tenancy’, ‘looking after your personal safety’, ‘getting e-connected’ and ‘returning to work or study’. Second, there are courses that focus on getting the most out of services: for example, ‘getting the best from your ward round or care review’, ‘understanding the Mental Health Act and mental health review tribunals’ or ‘making a complaint’.
Capacity building among the peer workforce
Recovery Colleges provide courses that drive changes across the service by training peer support workers and peer trainers and providing courses that enable people with lived experience to participate in staff selection and training or sit on committees. The skills and confidence that people gain in these courses are useful not only within services, but are also transferrable to opportunities and employment outside services.
Family and friends
Some courses specifically focus on the challenges faced by people who provide care and support for family members and friends with mental health conditions. These are often attended by the individual and their relatives and assist the whole family to live with the challenges they face. This opportunity for families to learn together has proved particularly popular.
All Colleges produce an attractive prospectus for potential students detailing the courses provided. While staff may inform the people they serve about the College and help them to explore the possibilities there, people are not ‘referred’. Individual students enrol and register on the courses that interest them. The Colleges in Nottingham and South West London have grown rapidly, driven by popular demand and it has been difficult to keep pace with demand for courses. In terms of staffing:
- The South West London Recovery College – opened with a core staff complement of one full-time mental health practitioner and four part-time peer trainers providing eight pilot courses with some sessional input from staff in other teams within the organisation. By 2010 it offered 52 courses in 11 locations serving around 50 people per day. A total of 1350 different people used the College in its first year of operation.
- The Nottingham Recovery College started with a core staff complement of one fulltime mental health practitioner and 12 courses run by four sessional peer and sessional staff trainers drawn from other teams within Notttinghamshire Healthcare NHS Trust. In its third term the College offered 101 courses spanning 45 different topics, running in eight locations.
The evidence base
A core component of Recovery Colleges is helping people to become experts in their own self-care. There is now a considerable body of evidence demonstrating the effectiveness of supported self-management education in health conditions of all types (Rinaldi, 2002; Foster et al., 2007; Cook et al., 2011). An educational approach which brings together the expertise of professional and lived experience also lies at heart of the ‘expert patient programmes’ that have proved so useful in relation to a range of long term health conditions (Department of Health, 2001; 2006; Lawn et al., 2007). Supporting self-management is now defined by National Institute for health and clinical excellence (NICE) as a key quality standard of adult mental health services, as part of the service user experience guidance (2011).
A wealth of evidence demonstrates the effectiveness of peer support within mental health services (Repper & Carter, 2011) and Recovery Colleges offer peer support from both peer trainers and fellow students.
Recovery Colleges are still in their infancy in this country so the evaluative evidence is limited. However, they have certainly proved very popular among those who use them:
“I wouldn’t be here if it wasn’t for the College.”
“What a positive and helpful approach. This type of course should have started years ago.”
“Extremely informative… it has given me further insight into myself and my thinking.”
“I can study in a safe place so I don’t have to worry if it goes pear-shaped if I get unwell – I can be safe learning.”
“It’s like the sun coming out to go into the Recovery College… it’s a wonderful proclamation of service users (and carers) being of value.”
Prior to the establishment of the South West London Recovery College, a pilot study was conducted comprising four recovery courses co-delivered by mental health practitioners and peer trainers (Rinaldi, Wybourn & Clenahan, in press). On average, students had been using mental health services for six years and 45% had a diagnosis of psychosis. Students were enthusiastic about the courses, with an 18 month follow-up showing:
- the majority (68%) felt more hopeful for the future than they had at the start of their course, most (81%) had developed their own plan for managing their problems and staying well; and 70% had become mainstream students, gained employment or become a volunteer;
- compared with those who did not attend courses, those who attended more than 70% of their scheduled sessions (67% of those who started) showed a significant reduction in use of community mental health services.
The comments made by students at Nottingham and South West London Colleges reinforce these findings:
“I have moved further in my recovery in one term here than in the past two years in the team.”
“I’ve halved my medication and learned lots of different ways to manage my anxiety.”
“I can’t believe what you have done for my son. I used to have to push him out of the door and he would cover his face. Now he goes out with his head held high.”
A survey of community mental health team care co-ordinators conducted one year after the establishment of the South West London Recovery College (Rinaldi & Suleman, 2012) showed that the majority (66%) had people on their caseload who had attended the College and they considered that people had benefited greatly from their attendance. In comparison with those who had no-one on their caseload who had attended the College, care co-ordinators who supported people who had used the College placed a higher value on self-management, were more comfortable about supporting them in these endeavours, and had higher expectations for those whom they served. Their comments included:
“I have a strong belief that service users have inner strengths, skills and resources and, with the right support ,such as courses at the Recovery College, can become experts in their own health and wellbeing and rebuild their lives.”
“Self-management is an integral part of my own approach which aims to foster independence, increased self-reliance, and the service user’s sense of responsibility for their own life outcomes.”
The transformative power of the Recovery College
The power of Recovery Colleges is two-fold. First, they assist the individuals whom they serve in their personal and collective journeys of recovery. Second, they assist organisations and services to become more recovery-focused. The creation of recovery-focused services requires a major transformation in purpose and relationships: a focus on rebuilding lives rather than reducing symptoms alone and a partnership between equals, rather than ‘experts’ and ‘patients’.
Recovery Colleges embody and drive these transformations in a number of ways:
1. They enable people to become experts in their own self-care and develop the skills they need for living and working
Recovery Colleges enable people to become experts in their own self-care and develop skills and confidence to manage their own recovery journey.
2. They explicitly recognise the expertise of mental health professionals and the expertise of lived experience in a process of ‘co-production’
A Recovery College is run by both peer trainers and mental health practitioner trainers. All courses are co-produced, co-delivered and co-received by staff, people with mental health problems and the people who are close to them.
3. They break down the destructive barriers between ‘them’ and ‘us’ that perpetuate stigma and exclusion
Co-produced, co-delivered courses enable students to see what people with mental health problems can achieve. Trainers are both people with lived experience and mental health practitioners (who may themselves have lived experience of subjects in which they provide training) and they are employed on equal terms. Barriers between ‘them’ and ‘us’ are not only broken down in the provision of courses, they are also broken down within the student group. People with lived experience and those who provide their support (both informal carers and mental health practitioners) learn together and from each other. The transformation from ‘service user’ to ‘student’ affords a positive identity beyond that of ‘mental patient’.
4. They provide peer support
In Recovery Colleges the peer support offered by peer trainers and fellow students enables people to feel less alone, offers images of hope and possibility and allows people to learn from others who have faced similar challenges and use their lived experience to help others.
5. Group learning and mutual support replaces the disabling isolation engendered by a sole reliance on individual work
Recovery Colleges create a network of social opportunities among peers and the general community which can reduce the social isolation that so many people experience. Like any students, people attending Recovery College courses often form relationships that extend beyond the classroom.
6. They afford choice, control and self-determination Students are not passive recipients of the ‘prescriptions’ of experts.
Within a Recovery College there are no prescriptions: students select the courses that interest them from a prospectus, do their own research in a library, and attend courses that enable them to take control and pursue what is important to them.
7. They promote participation in the local community A Recovery College achieves this in three ways.
First, people from local organisations can be involved in providing courses. Second, individuals can attend courses that assist them to develop the knowledge and skills necessary to return to work, study, and participate in the community. Third, people with a diagnosis of a mental health condition study alongside their relatives, friends and neighbours.
From margins to mainstream
Many services are in the process of developing Recovery Colleges, however, they remain ‘pilot’ services. Their full transformative power cannot be fully realised until they move from being a novel, marginal addition to being a central component of recovery-focused services.
For individuals, the research literature demonstrates the importance of ensuring that self-management education is fully integrated into healthcare systems and that learning is reinforced by all professionals with whom the person has contact (Coulter, 2011; Protheroe, Rogers & Kennedy, 2008; Pulvirenti, McMillan & Lawn, 2011). Similarly, if people are to take control over their lives and pursue their aspirations it is important that the confidence, skills and insights they gain from the Recovery College are not undermined by experiences with other parts of the mental health service.
For services and organisations, the Recovery College must become a core driver for whole system change. This can be achieved in three ways. First, they are able to model different relationships between people using services and mental health practitioners. Second, they can identify and prepare people with lived experience for employment as peer workers across the service. And third, they may replace some elements of existing services. These elements can make a Recovery College a high impact development with a major ‘domino effect’ across a mental health service over time.
Colleges cannot, of course, replace all specialist assessment and treatment or non-specialist outreach support. But mental health services try to provide a great deal more than this in the form of information, advice on self-management and support in day-to-day life for both individuals and their families – all delivered, almost exclusively, on an individual basis. The opportunity to reduce costs and provide services in the form of co-produced seminars and courses that decrease isolation and increase peer support, while at the same time offering a broad range of professional expertise, therefore has the potential to deliver a ‘win-win’ situation – better services at lower cost.
A note on authorship
Advances in recovery-focused practice have arisen from collaborative partnerships between a number of individuals and organisations. The Implementing Recovery through Organisational Change (ImROC) briefing papers draw upon this work. Where ideas are taken from published materials we cite them in the conventional form, but we also want to acknowledge the many unpublished discussions and conversations that have informed the creative development of the project as a whole over the last five years. Each paper in this series is written by those members of the project team best placed to lead on the topic, together with invited guest authors and contributions from other team members. We particularly wish to acknowledge the contribution of those whose work on the practical implementation of recovery values has formed the testbed for many of the ideas. Without these pioneers, there would be nothing to write about.
References
Ashcraft, L. (2000) META Services recovery education center business plan. Phoenix Arizona: META Services Inc.
Ashcraft, L. & Anthony, W. (2005) A story of transformation, Behavioral Healthcare Tomorrow, April, 12-22
Cook, J.A., Copeland, M.E., Jonikas, J.A., et al. (2011) Results of a randomised controlled trial of mental illness self-management using wellness recovery action planning. Schizophrenia Bulletin doi: 10.1093/schbul/sbr012
Coulter, A. (2011) Engaging patients in healthcare. Maidenhead: Open University Press.
Department of Health (2001) The Expert Patient: A new approach to chronic disease management for the 21st century. Department of Health: London
Department of Health (2006) Supporting people with long-term conditions to self-care: A guide to developing local strategies and good practice.
Department of Health: London Department of Health (2011) No Health Without Mental Health: A Cross-Government Mental Health Outcomes Strategy for People of All Ages. London: HM Government
Foster, G., Taylor, S, J, C., Eldridge, S. Ransay, J. & Griffiths, C.J. (2007) Self-management education programmes by lay leaders for people with chronic conditions. Cochrane database of Systematic Reviews Issue 4. Art. No.: CD005108.
Lawn, S., Battersby, M. W., Pols, R. G., Lawrence, J., Parry, T., & Urukalo, M. (2007). The mental health expert patient: Findings from a pilot study of a generic chronic condition self-management programme for people with mental illness. International Journal of Social Psychiatry, 53(1), 63-74
National Institute for Health and Clinical Excellence (2011) Service user experience in adult mental health: improving the experience of care for people using adult NHS mental health services, NICE clinical guideline 136 www.nice. org.uk/cg136
Perkins, R. (2012) UK mental health policy development – An alternative view, in Phillips, P., Sandford, T. and Johnston, C. (eds) Working in Mental Health: Practice and Policy in a Changing Environment, Oxford: Routledge
Perkins, R. & Slade, M. (2012) Recovery in England: Transforming statutory services? International Review of Psychiatry, 24(1), 29-39
Protheroe, J. Rogers, A., Kennedy, AP., et al. (2008) Promoting patient engagement with selfmanagement support information: a qualitative meta-synthesis of processes influencing uptake. Implementation Science. 3, 44.
Pulvirenti, M., McMillan, J., Lawn, S. (2011) Empowerment, patient centred care and selfmanagement. Heath Expectations. Doi:10.1111/ j.1369-7625.2011.00757.x.
Repper, J. & Perkins, R. (2003) Recovery and Social Inclusion, London: Balliere Tindall
Repper, J. & Carter, T. (2011) A review of the literature on peer support in mental health services, Journal of Mental Health, 20(4): 392–411
Repper, J. & Perkins, R. (2012) Recovery: A journey of discovery for individuals and services, in Phillips, P., Sandford, T, & Johnston, C. (Ed) Working in Mental Health: Practice and policy in a changing environment, Oxford: Routledge
Rinaldi, M. (2002) Manic depression and self management, in Ramsey, R., Page, A., Goodman, T. & Hart, D. (Eds.). Changing Minds: Our Lives and Mental Illness. London: Gaskell
Rinaldi, M. & Suleman, M. (2012) Care co-ordinators attitudes to self-management and their experience of the use of the South West London Recovery College, London: South West London and St George’s Mental Health NHS Trust
Rinaldi, M., Wybourn, S. & Clenahan, M. (in press) The development, piloting and outcomes from a Recovery College in England, Psychiatric Rehabilitation Journal
Shepherd, G., Boardman, J. & Slade, M. (2008) Making Recovery a Reality. London: Sainsbury Centre for Mental Health
Shepherd, G., Boardman, J. & Burns, M. (2010) Implementing Recovery: a methodology for organisational change, London: Sainsbury Centre for Mental Health
