The long-standing myth that mental health service providers, users and commissioners “can’t agree on what recovery is, nor offer any evidence for it” is finally laid to rest in this paper.
Supporting recovery in mental health services: quality and outcomes aims to help organisations in the mental health sector develop clear, empirically-informed statements about what constitutes high-quality services, and how these will lead to key recovery outcomes for service users. It also includes a series of recommendations for health and social care providers and commissioners, and for NHS England and the Government, that aim to support development of an evidence-based approach to commissioning mental health services.
Download 8. Supporting Recovery in Mental Health Services: Quality and Outcomes
8. Supporting Recovery in Mental Health Services: Quality and Outcomes
Geoff Shepherd, Jed Boardman, Miles Rinaldi and Glenn Roberts
INTRODUCTION
The development of mental health services which will support the recovery of those using them, their families, friends and carers is now a central theme in national and international policy (DH/HMG, 2011; Slade, 2009). In order to support these developments we need clear, empiricallyinformed statements of what constitutes high-quality services and how these will lead to key recovery outcomes. This is what the present paper aims to do.
We have had to be selective in terms of the evidence we have considered and, in many cases, we have had to make subjective judgements to come to simple recommendations. We understand that not everyone will agree with our conclusions. Nevertheless, we hope that, at the very least, they will provide a useful framework within which discussions about quality and outcome can take place at a local level in a more informed way. We therefore hope that the paper will be of value to both commissioners and providers.
A NOTE ON AUTHORSHIP
Advances in recovery-focused practice arise from new collaborative partnerships between the people who work in mental health services and the people who use them. The ImROC briefing papers draw upon this work. Where ideas are taken from published materials we cite them in the conventional form, but we also want to acknowledge the many unpublished discussions and conversations that have informed the creative development of the project as a whole over the last five years. Each paper in this series is written by those members of the project team best placed to lead on the topic, together with invited guest authors and contributions from other team members. On this occasion the authors would also like to acknowledge the contribution of Mike Slade and his colleagues in the REFOCUS group at the Institute of Psychiatry to this paper. Their careful research and generous willingness to share ideas has been invaluable to the thinking summarised here.
BACKGROUND
The ImROC programme (Implementing Recovery through Organisational Change) was established by the Department of Health in England in 2008 to help local services become more supportive of recovery for those using them and their carers (Shepherd et al., 2011). Arising from this work, we have described the basic principles of recovery (Shepherd, Boardman & Slade, 2008), presented a methodology for achieving organisational change in mental health services (Shepherd, Burns and Boardman, 2010), and described how key elements of more recovery-oriented services might be developed (Perkins et al., 2012; Alakheson & Perkins, 2012; Boardman & Friedli, 2012; Repper, 2013). Most recently, we have presented evidence for the potential cost effectiveness of services which employ formal, peer workers (Trachtenberg et al., 2013). However, we have not yet formally addressed the key issues of ‘quality’ and ‘outcomes’.
Quality indicators provide the key link between evidence-based practice and improved outcomes (McColl et al., 1998). Thus, if we can identify a set of indicators for which there is evidence that, if present in a service, they will lead to specific outcomes which support recovery then this gives us a way of assessing its quality as a ‘recoveryoriented’ service. This does not conflict with our fundamental belief that recovery belongs to the people who use mental health services and is embedded in their unique and individual lives. Judgements about ‘quality’ and ‘outcomes’ must therefore ultimately rest with them, but at the same time we recognise that clinicians and managers need information which will guide them to provide services to support recovery in the most effective and efficient ways. We recognise that this is an ambitious undertaking – quality in healthcare is always highly multi-facetted – nevertheless, we have attempted to describe a structure which will make these complicated ideas accessible to a non-specialist audience, as well as to mental health professionals, managers and commissioners.
Our primary focus has been on the experience of adults of working age using specialist mental health services. This should not be taken to imply that we are not interested in applying this thinking to services which support recovery in other groups, e.g. children, older people, those with mental health problems not in touch with specialist mental health services. Nor does our emphasis on quality and outcomes in formal services imply that we believe these are necessarily the most important sources of support for recovery. Often, these are friends, families, community groups, churches, etc. and this is evidenced repeatedly in the rich collections of life stories of people who are ‘in recovery’ (e.g. Davies et al., 2011). Their contribution should never be overlooked.
CURRENT ISSUES
As indicated above, the purpose of trying to identify valid quality indicators is to give commissioners and providers a basis for designing services that are most likely to produce certain outcomes. In the current climate this is becoming increasingly urgent as services in England struggle to categorise groups of patients with similar levels of need into different ‘clusters’ and then estimate the costs associated with effective care pathways for people who fall into these clusters. This system is known as Payment by Results (PBR) and it is intended that it will form the basis of new funding formulae for mental health services. Whether it will be successful or not is, at the moment, unclear. What is clear is that if recovery-supporting service developments are to be funded in the future, then recovery quality indicators need to be built into the care pathways in all the relevant clusters.
This in turn means that these indicators should have evidence for their association with outcomes comparable to those approaches described in the guidance for effective service provisions produced by the National Institute for Health and Care Excellence (NICE). This presents difficulties for recovery-oriented services because many of the elements are relatively new and the evidence base is therefore inherently limited (although not, as we shall see later, non-existent).
In addition to these attempts to specify quality indicators in the context of PBR cluster pathways, recent dramatic failures of care have given rise to a much greater emphasis on indicators which are not necessarily evidence-based, but reflect very basic criteria for compassionate and humane services (Francis, 2013). This renewed emphasis on the quality of supporting relationships is welcome and, as we shall see, it is highly consistent with recovery principles.
Given the complexity of the subject matter to be presented here, we have decided to take the unusual step of dividing the remainder of the paper into two. Part I contains a summary of the key indicators and recommendations for outcome measures. Part II contains a technical appendix which sets out additional detailed information to justify the quality and outcome measures recommended.
PART I. SUMMARY AND RECOMMENDATIONS
Quality indicators at an individual level
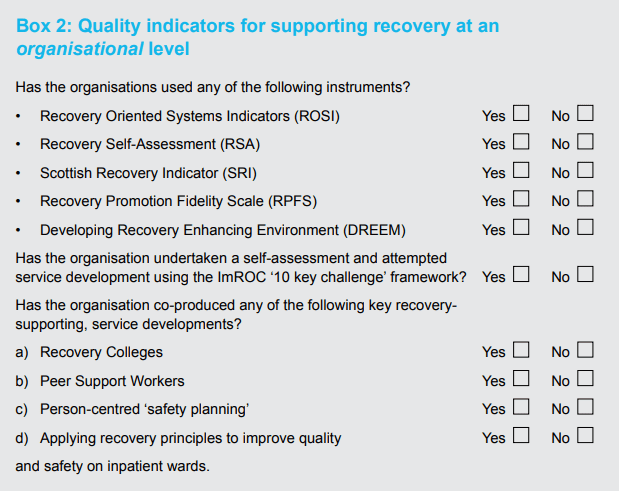
In terms of specifying quality indicators for recovery, it is useful to distinguish between service quality at the level of individual interactions and organisational level features. At an individual level, Slade and his colleagues in the REFOCUS group have made a further helpful distinction between ‘recovery-promoting relationships’ and ‘pro-recovery working practices’ (Bird et al., 2011). The former relates to the general quality of the therapeutic relationship and applies to all relationship-based interventions (this covers the kind of basic relationship factors referred to in the Francis Report (Francis, 2013)). The latter refers to a specific set of practices relating to the support of recovery. In addition to these, we can add a number of approaches which, although not necessarily derived directly from recovery ideas, are nevertheless highly consistent with supporting recovery for individuals. This set of individual level indicators is summarised in Box 1. The individual level quality indicators shown in Box 1 could easily be converted into a selfassessment tool for auditing services and could form part of the contract specification for providers.
Box 1: Quality indicators for supporting recovery at an individual level
Staff should aim to…
Facilitate recovery-promoting relationships
- establish shared values
- demonstrate good, basic relationships skills (empathy, warmth, respect)
- support personal hopes and aspirations
- promote a sense of control (‘agency’).
Use ‘pro-recovery working’ practices
- narrative accounts (recovery stories)
- a ‘strengths’ approach
- ‘coaching’ methods
- Personal Recovery Plans (WRAP, STAR)
- self-management
- shared decision-making
- person-centred ‘safety planning’.
Consider specific approaches which will support recovery not developed from a recovery perspective, e.g.
- Joint Crisis Plans (JCP)
- ‘Housing First’
- Individual Placement and Support (IPS)
- use of ‘personal budgets’ (social and health).
Recovery-promoting relationships
Relationships are at the heart of recovery. The creation of supportive relationships depends upon establishing shared values and demonstrating empathy, warmth, respect and a willingness to go the ‘extra mile’ (Borg & Kristiansen, 2004). These form the bedrock for all forms of care and, some would argue, have been undermined by the increasing ‘marketisation’ of healthcare with its emphasis on impersonal service transactions, rather than the relationships within which these transactions take place. Positive relationships are at the heart of basic, good care highlighted in the Francis Report (2013) and they also show considerable overlap with the NICE quality standards (NICE, 2011; 2013, see Technical Appendix). High quality, recovery-oriented services should also be consistent with the key recovery principles identified by Repper & Perkins (2003) – hope, control, and access to ‘opportunities to build a life beyond illness’.
Pro-recovery working practices
In terms of recovery-oriented practices, the starting point must be to encourage the person to tell their story. Narrative accounts are the oldest – and probably the most powerful – ways in which we make sense of the world and build relationships. Everyone has a story to tell and the process of storytelling is almost always experienced as positive and validating. Narratives are inherently meaningful and are expressed in a form and language that is accessible to everyone (Greenhalgh & Hurwitz, 1999). They also provide a source of information and explanation which is complementary to a conventional ‘evidence-based medicine’ approach (Roberts, 2000). We should therefore give the use of narrative accounts the central place in the practice of recovery that it deserves, both in helping people formulate goals and in monitoring outcomes (see below).
A second important practice is the consistent use of a ‘strengths’ approach (Rapp & Goscha, 2006). This seeks to identify the person’s competencies and their environmental resources (friends, neighbours, local opportunities) which might be used to further their personal life goals. The strengths assessment is often based on simply encouraging the person to tell their story as this can provide important clues to activities and interests that were pursued in the past which could be used again in the future. The ‘strengths approach’ therefore offers an important contrast to the ‘deficits model’ which has tended to dominate mental health practice up to now.
Another recovery-supporting practice, which has been developed in the last few years, is the ‘coaching’ model (Bora et al., 2010). This uses many of the same techniques as the strengths approach, e.g. an emphasis on the service user taking the lead, the importance of identifying personally-relevant goals, a focus on strengths and natural supports. However, there is greater emphasis on the importance of staff behaviour as a ‘coach’, or learning partner (‘on tap, not on top’) and on the service user’s responsibilities to make a commitment to action. Although there is good evidence for the effectiveness of coaching in relation to the management of long-term health conditions (O’Connor, Stacey & Legere, 2008) there is little evidence as yet regarding its specific effectiveness in relation to supporting recovery in mental health.
The use of narratives, building on strengths and a coaching approach can then form the starting point for the development of Personal Recovery Plans. These may be based on formal tools such as the ‘Wellness Recovery Action Plan’ (WRAP) (Copeland, 1997) or the Recovery STAR (McKeith & Burns, 2010) or simply developed from the person’s narratives or an analysis of their strengths. Whatever their derivation, Personal Recovery Plans should contain an identification of the person’s internal and external resources and a plan for how they can use these to take control of their life and achieve their chosen goals (Perkins & Rinaldi, 2007). The person should not necessarily have to share their recovery plan with staff: they belong to them. They are therefore not the same as ‘care plans’, although it is clearly desirable if there is as much overlap as possible between the two (Rinaldi & Watkeys, in press).
WRAP is a framework for developing a personal plan to cope with distressing symptoms, prevent relapse, manage crises and stay ‘well’. It was designed by a service user for service users. WRAP has been widely used in England and there are some good practical examples of the difficulties and benefits of implementation (Hill, Roberts & Igbrude, 2010). The Recovery STAR is also currently very popular. It contains ten ‘domains’ of recovery and the service user and staff member work together to rate each domain area on a ten point scale. The results are then presented visually on a Star diagram. This is an attractive, easy-to-understand, format and most service users seem to find the ten domains helpful for identifying personal goals, although some report that it needs to be more personalised. Both WRAP and the STAR are therefore useful methods for engaging people and assisting with personal recovery planning and monitoring individual progress. They are less useful as outcome measures (see below).
As indicated earlier, an important theme in most people’s recovery is the struggle to achieve a greater sense of control over their symptoms and their life in general. Thus, improving the person’s capacity for self-management is critically important. Self-management can refer to a wide variety of methods from simply handing out leaflets, to personal support through telephone monitoring, goal-setting, coaching and structured education. There is strong evidence, mainly from studies in the physical healthcare field, that supporting self-management can be extremely helpful in terms of ameliorating symptoms, improving quality of life, and reducing dependency on formal health care interventions (Foster et al., 2007; De Silva, 2011). Approaches which include full and active involvement of the person, rather than the passive provision of information, are also likely to be most effective. Thus, De Silva recommends, “a fundamental transformation of the patient-caregiver relationship into a collaborative partnership” (p.vi).
Mueser and his colleagues in the U.S. have developed a comprehensive educational and self-management package designed to provide people with severe mental illness with the information and skills necessary to manage their symptoms more effectively and work towards achieving personal recovery (Mueser et al., 2002). This has become popular in the U.S. and has attracted some interest in Europe. The ‘Illness Management and Recovery Programme’ (IMR) consists of five components:
- ‘psycho-education’ regarding severe mental illness
- the provision of information on medication and side effects, using a ‘motivational interviewing’ approach
- a relapse prevention programme
- training in coping skills and problem-solving
- a cognitive-behavioural approach to symptom management.
Preliminary findings have been published regarding its implementation in small samples in the U.S. and Australia (Mueser, et al., 2006; Salyers, 2006) and a randomized controlled trial found that service users appeared to have increased their knowledge of illness, coping skills, personal goal identification and attainment (Hasson-Ohayon et al., 2007). There was weaker evidence of improvements regarding hope and no significant gains regarding social support or help from others. Salyers et al. (2009) also evaluated a statewide implementation of IMR and found evidence of increased hope, but not satisfaction. Systematised programmes like IMR provide a good summary of basic information and give general tips on self-management but, viewed in the context of the De Silva (2011) review, IMR cannot be said to be an example of ‘co-production’. In our view, this is a vital missing ingredient.
Alongside self-management approaches, there has also been increasing interest in ‘shared-decision making’. This brings together two sources of expertise – the knowledge, skills and experience of health and social care professionals and the individual’s own knowledge and expertise of their own condition. Both forms of expertise are key to making good decisions. Used together they enable the person to make choices regarding treatment and management options that are most consistent with research evidence and with their own preferences and priorities. ‘Shared decision-making’ is therefore the basis of truly informed consent. There are a number of examples of the value of this approach in the physical healthcare field (e.g. Simon et al., 2009) and they are now beginning to be applied in mental health, particularly in relation to medication management (Deegan & Drake, 2008; Torrey & Drake, 2009; SAMSHA, 2011). A helpful article recently appeared ‘coproduced’ by service users, carers and professionals which sets these approaches clearly within the framework of recovery-oriented practice (Baker et al., 2014).
As a result of negative coverage in the media and perceived external pressures, the assessment and management of risk has become a prominent issue in mental health services. Many staff have become highly ‘risk averse’ and are reluctant to engage in what might have been seen in the past as ‘positive’ risk taking, i.e. working with service users to help them identify risk management strategies which are necessary in order to take pursue reasonable and realistic life goals. This has happened despite clear government guidance to the contrary (Department of Health, 2007). However, in the past few years recovery-oriented professionals have developed new approaches to managing risk which are based on working with the person to examine what risks may prevent them from pursuing their chosen life goals and then involving them fully in the development of a plan to support the pursuit of these goals in ways that are safe for them and those around them. This is known as person-centred ‘safety planning’ and will be the subject of a forthcoming Briefing paper (Boardman & Roberts, in press).
Approaches which support recovery not developed from a recovery perspective
In addition to these general ‘pro-recovery’ working practices, staff should also be trying to offer a number of specific approaches to help people in their recovery which have not been developed from a recovery perspective.
For most people their Personal Recovery Plan will involve them avoiding unnecessary admissions to hospital, particularly if these are compulsory under the Mental Health Act. The Joint Crisis Plan (JCP) is a relatively new invention which has been specifically developed to achieve these aims and is based on a process of co-production (Henderson et al., 2004). The JCP is formulated by the service user, together with peer support if available and the key mental health staff involved in their care, including the treating psychiatrist. It is therefore similar to an ‘advance statement ’, or the kind of crisis plan contained in WRAP, but with the crucial inclusion of the clinical staff and the treating psychiatrist in the formulation of the plan. In an initial randomised controlled trial, people who were discharged with a Joint Crisis Plan were shown subsequently to have significantly fewer compulsory admissions compared with controls (Henderson et al., 2004). Qualitative data also suggested that the JCP group felt more ‘in control’ of their mental health problems (Henderson et al., 2008). A second study produced less impressive results, but the authors acknowledge that this was mainly due to practical difficulties in ensuring that the joint planning meetings always occurred and were effectively facilitated (Thornicroft et al., 2013). The addition of peer support workers to inpatient teams may be one way of ensuring that JCPs are routinely offered.
Housing, employment and money are then the key building blocks in most people’s recovery and it is therefore important to ensure that effective methods for achieving these goals are available for everyone attending mental health services.
The ‘Housing First’ initiative was developed in the U.S. to meet the needs of homeless people with complex mental health and substance misuse problems. It prioritises the identification of suitable housing, based on personal preference, and then delivers other supportive services to the person once they are housed, without a pre-requisite that their substance misuse must cease first. The use of permanent housing options and the commitment to floating support means that the resident does not have to make continual moves between different types of accommodation as their support needs change. A four-year longitudinal study compared the ‘Housing First’ model with traditional ‘treatment first’ approach and found a significantly higher rate of retention for residents in the Housing First model (88% v. 47%, Padgett, Gulcur & Tsemberis, 2006). Despite there being no requirement for the Housing First group to abstain from substance misuse there was actually no significant difference between the two groups regarding their levels of drug and alcohol use. However, the annual per capita costs of the Housing First programme were around half those of ‘treatment first’ programmes. This approach is now being tried in England (Shelter, 2008) but is not widespread, often because of the lack of available housing alternatives.
The ‘Individual Placement and Support’ (IPS) approach has been designed to help people with severe mental health problems gain and retain paid employment. It has a number of similarities with the Housing First method. Thus, it is also based on placing the person in a work position of their choice as quickly as possible and then providing them and with an integrated package of vocational and clinical support in situ (Becker, Drake & Concord, 1994). There is now very strong evidence, both nationally and internationally, that IPS consistently achieves employment rates two to three times better than traditional alternatives such as pre-vocational training and sheltered workshops (Burns et al., 2007; Bond, Becker & Drake, 2008; Sainsbury Centre for Mental Health, 2009a). The one study where IPS failed to produce such impressive results was where it was not implemented with good fidelity to the research model (Howard et al., 2010; Latimer, 2010). Longer term follow-up studies of people placed through IPS suggest that the higher rates of employment are maintained and have positive impact on non-vocational outcomes – e.g. improved confidence and wellbeing, reduced sense of stigma. In addition, they are associated with reduced use of mental health services, leading to reduced costs (Sainsbury Centre for Mental Health, 2009b).
Finally, we should note the importance of money in the lives of people with mental heath problems (Parsonage, 2013). Personal budgets may be a source of supplementary income to help with specific social and vocational goals. There are still practical problems around the implementation of these personal budgets, mainly regarding their availability, bureaucracy involved and ensuring that resources are effectively targeted on those in greatest need, but the principle of providing someone with resources that they can choose to spend on what they think will help them must be correct. The use of personal budgets to support recovery is discussed in detail in Alakeson & Perkins (2012).
Quality indicators at an organisational level
The quality of support for individuals to pursue their recovery goals ultimately depends on the quality of care provided by individual staff in their everyday interactions. However, in order for these recovery-supporting relationships to be maintained, the organisation also needs to demonstrate its commitment to recovery principles and to creating a ‘recovery-supportive’ culture. How might this be measured?
Burgess et al. (2011) reported a systematic review of 11 instruments aimed at assessing the ‘recovery-orientation’ of organisations. They examined each measure in terms of its ease of use, whether or not it satisfactorily reflected a ‘consumer’ perspective and its psychometric properties. They ended by recommending just four:
- Recovery-Oriented Systems Indicators (ROSI)
- Recovery Self Assessment (RSA) tool
- Recovery-Oriented Practices Index (ROPI) (adapted for use in a British context as the ‘Scottish Recovery Indicator’)
- Recovery Promotion Fidelity Scale (RPFS).
(For details of these measures see the Technical Appendix).
All these instruments have advantages and disadvantages. All were developed in the U.S. or Australia and hence there are problems with cross-cultural application of specific items (Slade & Hayward, 2007). Most are also rather long and laborious to use. Some have reasonable inter-rater reliability and concurrent validity, but the test-retest reliability has generally not been thoroughly investigated. This is a key limitation in tools designed to measure change as it makes it impossible to assess what constitutes ‘real’ change and what is simply measurement error. In addition, most of the measures give no information about sensitivity to change.
A similar review of organisational measures by Williams et al. (2012) also included the ‘Recovery Enhancing Environments Measure’ which is well known in its English version DREEM (Dinniss et al., 2007). Like Burgess et al. they concluded that, ‘none of the measures identified can be recommended for use outside their country of origin without further testing. Further psychometric testing, particularly in terms of reliability and sensitivity to change, would provide further evidence of the accuracy and utility of the measures’ (p.1834, op cit).
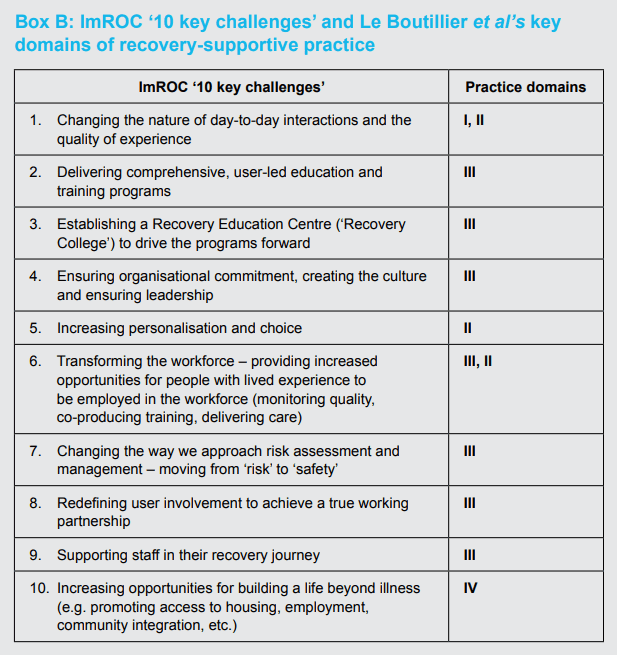
The ImROC ‘10 key challenges’
Given all these problems, it seems safest at this stage to concentrate on attempts to assess organisational recovery-orientation which are primarily designed to support service development, rather than trying to provide a formal measure of quality. This is what the ImROC ’10 key challenges’ framework was designed to do.
It was developed specifically to help organisations work together to review their current state of development regarding the provision of recovery-oriented services. The framework then assists the groups to set specific targets for service change (Shepherd, Boardman & Burns, 2010). It was not designed as a psychometric instrument and its test-retest or inter-rater reliability have never been explored. However, it does appear to have good content validity if one compares it with the areas identified by Le Boutillier et al. (2011) in their international review of recovery-oriented practice. It has also now been used widely to support the development of more recovery-oriented services by a range of different groups – staff, service users and carers, clinicians, managers – from both statutory and independent sector agencies (NHS Confederation/Centre for Mental Health, 2011; Shepherd, 2013) and has proved a useful heuristic.
As we have gained more experience in using the ’10 key challenges’ four specific elements have emerged as being particularly important in terms of high-quality, recovery-oriented services. These are: (a) the establishment of Recovery Colleges; (b) selecting, training and supporting Peer Support workers; (c) the move from professionally determined risk assessment and management to personcentred ‘safety planning’; and (d) the application of recovery principles to improve the quality of care and safety on inpatient units. All these elements are underpinned by a process of development which depends on ‘co-production’ between people using these services and professionals.
The concept of the ‘Recovery Colleges’ was described in an earlier briefing paper (Perkins et al., 2012). It is based on an ‘educational’ model and uses co-production to develop and deliver courses to students who are a mixture of service users and staff (co-learning). The emphasis is on providing an environment where people can develop their own understanding of mental health issues and how best to manage them. Recovery Colleges are very popular with service users and can often engage people who find traditional services unacceptable. Preliminary (uncontrolled) evidence suggests that two-thirds of those attending at least 70% of the sessions felt more hopeful about the future and were more likely to have developed their own recovery plans. They also showed more engagement in volunteering, education and paid employment (Rinaldi, Wybourn & Clenehan, 2012).
Support from peers in mental health services has been present for a long time, but formally employed Peer Support workers are relatively new. They have been shown to produce a range of improved outcomes including greater optimism about the future, increased selfesteem, a greater sense of empowerment and reduced self-stigmatisation (Repper & Carter, 2010; Repper, 2013a). They also give benefits to those providing the service and help change the organisational culture to one where the contribution of service users is more highly valued and where expectations are raised. A selective review of the effects of adding peer support workers to acute inpatient and crisis teams further suggests that they can also be highly cost effective (Trachtenberg et al., 2013). If Peer Support workers are to have the greatest possible impact then their integrity must be maintained. This means that the whole organisation needs to be prepared to support their introduction and ensure that their key working principles are upheld through careful attention to the processes of recruitment, training, monitoring and supervision (Repper, 2013b).
The move from professionally determined risk assessment and management to person-centered ‘safety planning’ was mentioned earlier in the context of recovery-supporting practices. Minimisation of harm and preservation of safety remain clear aims of mental health services, but risk must be understood as inherent in everyday living and ‘positive risk-taking’ is a valuable route to the development of skills, confidence and resilience which may underpin the recovery process.
The application of recovery principles to improve the quality of inpatient care and reduce the use of physical restraints has been pioneered in the U.S. by Recovery Innovations (Ashcraft, Bloss & Anthony, 2012). ImROC sites in England (e.g. Merseycare) have developed a package, based on the ‘No Force First’ model, consisting of:
- an emphasis on the importance of basic, staff relationship skills (listening, respect, compassion)
- development of co-produced, individual ‘safety plans’ to replace traditional risk assessment and management methods
- avoidance of rigid interpretation of rules, encouraging flexibility
- using peer support workers to provide training and routine ‘de-briefing’ for staff following incidents
- introducing ‘advance directives’ or ‘Joint Crisis Plans’ to ensure that strategies for managing people in crisis accord with their wishes
- clear definitions for incidents, combined with systematic recording and feedback on frequency
- regular ‘Learning the Lessons’ events for staff and service users.
Because they are very new, these combined approaches do not have an extensive evidence base, however the preliminary results are very encouraging (King et al., 2013).
To summarise, a framework of quality indicators for supporting recovery at an organisational level is shown in Box 2.
Box 2: Quality indicators for supporting recovery at an organisational level
Outcomes
Good quality services should produce good outcomes. How to measure these? When considering outcome measures for recovery, we must first agree what constitute the key areas for measurement (‘domains’). In this we were considerably assisted by a series of meetings with a specially convened expert group who were asked to determine if there was a consensus regarding these key domains1,2. The results of these discussions are summarised in Box 3. For the first four domains there was a strong consensus regarding their importance as outcome measures; for the remaining two, the consensus was less strong.
Box 3: Summary recommendations for recovery outcomes measures
Definite
RECOVERY OUTCOME DOMAIN 1 – Quality of recovery-supporting care
To what extent do service users feel that staff in services are trying to help them in their recovery?
Recommended measure: INSPIRE
RECOVERY OUTCOME DOMAIN 2 – Achievement of individual recovery goals
To what extent have goals, as defined by the individual, been attained over time?
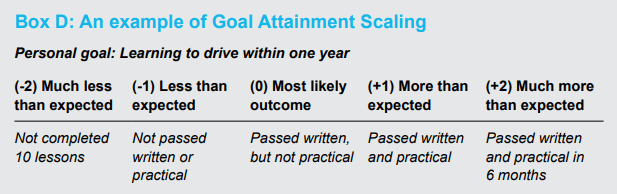
Recommended measures: Goal Attainment Scaling (GAS), narrative accounts
RECOVERY OUTCOME DOMAIN 3 – Subjective measures of personal recovery
To what extent do individuals feel that their hopes, sense of control and opportunities for building a life beyond illness have improved as a result of their contact with services?
Recommended measure: Questionnaire on the Process of Recovery (QPR)
RECOVERY OUTCOME DOMAIN 4 – Achievement of socially valued goals
Has the person’s status on indicators of social roles improved as a result of their contact with services?
Recommended measures: Relevant items from Adult Social Care Outcomes Framework (2013b), Social inclusion web.
Possible
RECOVERY OUTCOME DOMAIN 5 – Quality of life and well-being
Has the person’s quality of life and well-being improved?
Recommended measures: MANSA, WEMWBS
RECOVERY OUTCOME DOMAIN 6 – Service use
As a result of their recovery being supported, has the person made an appropriate reduction in their use of formal mental health services?
Recommended measures: Relevant items from the NHS Outcomes framework, and the Mental Health Minimum Data Set (but beware!).
RECOVERY OUTCOME DOMAIN 1 – Quality of recovery-supporting care
The first domain is not actually a measure of individual outcomes: it is really a measure of process. However, it is clear that if services are to be successful in supporting recovery outcomes, then they should be providing a different experience for the people using them. Improving patients’ experience of care figures prominently in both the NHS and Adult social care outcome frameworks (Department of Health 2013a; 2013b). The expert group agreed that quality of experience constituted an important recovery outcome in its own right.
Many services already use a range of survey methods – often ‘home-grown’ – to assess experience of care as part of local quality initiatives3. These are useful, but sometimes the methods used are not very sophisticated and the way in which samples have been constructed means that the results are not reliable. A more formal survey, using a standardised, self-report, postal questionnaire and a consistent random sampling method is provided by the ‘National Patient Survey’ (NPS) (www.nhssurveys.org/). The questionnaire was designed with considerable input from service users and several of the items are directly relevant to recovery issues. Despite the limitations of a postal questionnaire in terms of the relatively low response rate (approximately 30%) the data from the NPS do provide useful information which could be used as a ‘snapshot’ of outcomes regarding perceived quality of care, especially in terms of charting progress within a single service over time. The NPS could be improved if the sampling was targeted on specific clinical areas (including inpatient care) and the questionnaire data were supplemented by individual interviewing or focus groups4.
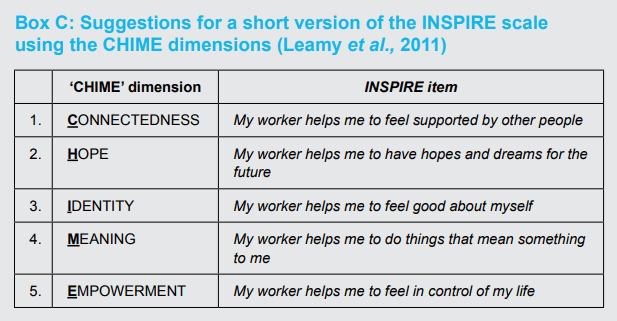
In our view, probably the best method for assessing perceived quality of care in relation to support for recovery is a new tool developed by the REFOCUS group at the Institute of Psychiatry in London known as INSPIRE (Williams et al., 2011). This tries to assess whether particular types of recovery support are important to the service user (hope, understanding, building on strengths, etc.) and whether she/he feels these are provided by their current mental health worker. It also asks questions about the general quality of the helping relationship. INSPIRE is relatively quick and easy to use (10 minutes to complete) and appears to have good face validity. There is some evidence that key areas may be missing – notably physical fitness, work and medication (Rinaldi, 2013) but, in general, the content validity is good. It is being used successfully by several sites in the ImROC programme (e.g. Newman-Taylor et al., in press). There is also a short, five item, version of INSPIRE5 now available (Slade, personal communication, 2013). This could form the basis of a quick and easy method for routine evaluation of service quality.
RECOVERY OUTCOME DOMAIN 2 – Achievement of individual recovery goals
Recovery is, of course, a unique and individual process. This poses particular challenges for attempts to measure outcomes since most measurement tools prescribe a particular set of outcomes and are designed to summarise effects between groups (e.g. in controlled trials). Thus, instruments like the STAR suggest a set of outcome domains in advance which may – or may not – be relevant to every individual. The STAR is also psychometrically weak with little evidence regarding its internal validity (Dickens et al., 2012) and even less regarding its test-retest reliability or external validity (Burgess et al., 2011; Hampson et al., 2011).
Probably the best known, truly individually-based, measure is the ‘Goal Attainment Scale’ (GAS), (Kirusek & Sherman, 1968). In this a specific outcome is agreed between the person and their care worker, together with different ‘levels’ of this outcome which might be achieved within a specific time period (e.g. ‘Most likely’, ‘More than expected’, ‘Much more than expected’, ‘Less than expected’ and ‘Much Less than expected’). Each level can be assigned a numerical score and different scores can also be weighted. The GAS has been widely used in mental health services and there is relatively good evidence for its inter-rater reliability and construct validity. It also shows good sensitivity to change (Hurn et al., 2006) and is almost completely flexible: it can reflect more-or-less any aspiration in terms of personal life goals. In many respects, it is therefore an ideal measure for individual recovery goals. However, the data are difficult to aggregate across individuals and it is therefore difficult to compare effects across groups.
If one is not interested in aggregating results across individuals, then it is worth considering narrative accounts (recovery stories) as outcome measures. These are highly personal and individualised and can capture outcomes in a very vivid, easy-to-understand form. These stories can be very powerful indicators of the effects of recovery-supporting services and, despite their simplicity, can provide compelling evidence for the effectiveness of particular kinds of support.
RECOVERY OUTCOME DOMAIN 3 – Subjective measures of personal recovery
The INSPIRE measure tries to measure the extent to which the person feels that the service is trying to support them along key recovery dimensions, but this is not the same as the person actually feeling more hopeful, more in control, more supported to build a life beyond illness, as a result. There are a number of examples in the literature of attempts to measure these kinds of outcomes with simple, Likert scales, e.g. ‘I feel more hopeful for the future as a result of the course’, Strongly agree > Agree > Neither agree nor disagree > Disagree > Strongly disagree’. These kinds of scales are quick and easy to use, with good face validity, but they are psychometrically weak, with unknown test-retest reliability, sensitivity to change, or social desirability bias.
In terms of standardised measures for subjective recovery, these were also covered in the Burgess et al. (2011) review cited earlier. Using the same criteria they employed to evaluate organisational recovery-orientation they examined 22 instruments and ended up (again) with just four possible candidates.
- Recovery Assessment Scale (RAS)
- Illness Management and Recovery Scales (IMR)
- Stages of Recovery Instrument (STORI)
- Recovery Process Inventory (RPI).
(Details of these instruments are given in the Technical Appendix).
As with the organisational tools, all these instruments have their strengths and weaknesses,and the problems of cross-cultural applicability still apply. They would therefore require further development and testing for routine use in an English context (or other countries). A useful measure which was not considered by Burgess et al., but which was developed specifically for use in a Britain with people with a diagnosis of psychosis, is the Questionnaire about Process of Recovery (QPR), (Neil et al, 2009). This has good coverage of the key recovery dimensions – hope, control, opportunity – and excellent psychometric properties (Shanks et al. 2013). It also closely maps onto the CHIME framework – Connectedness, Hope, Identity, Meaning and Empowerment – developed by Leamy et al. (2011) and has been used as the primary outcome measure in the REFOCUS study. We would therefore recommend it as the best standardised measure of personal recovery currently available for use in a British context.
RECOVERY OUTCOME DOMAIN 4 – Achievement of socially valued goals
Most people’s recovery story contains reference to the importance of quite objective, valued, social goals – ‘somewhere to live, something to do and someone to love’ (Perkins, 2012). These ‘objective’ indicators are relatively simple to define and, in principle, should be relatively straightforward to measure. For example, they are reflected in items from the NHS Outcomes Framework (Department of Health, 2013a) and the Adult Social Care Outcome Framework (Department of Health, 2013b). A list of possible indicators is suggested below:
- Engaged in whole or part-time paid employment of their choice
- Accessing volunteering
- Accessing education or training
- Participating in local community activities
- Reporting increased social network
- Living in settled accommodation of their choice where they feel safe and secure.
The problem with these ‘objective’ outcomes lies in ensuring that they are defined unambiguously and then in setting up systems for routine data collection. Given the enormous problems with large scale information systems, this is probably best achieved by small scale, local initiatives.
Regarding these kinds of social goals, the ‘Social Inclusion Web’ (Hacking & Bates, 2008) provides a practical resource to help individuals (or groups) chart and then monitor their progress regarding increasing community inclusion. It covers eight domains of social contact – employment, education, volunteering, arts & culture, faith and meaning, family and neighbourhood, physical activity and services – and assesses the number of people in the person’s social network and the number of places that matter to them. The information is intended to be produced by a joint discussion between the person and their key worker and the results are presented in an easy-to-understand, ‘clock’ diagram. Data from 150 service users in Liverpool demonstrated good sensitivity to change and good content validity.
The final two domains are important, but received less consensus support from our stakeholder group.
RECOVERY OUTCOME DOMAIN 5 – Quality of life and well-being
Intuitively, supporting people to pursue their recovery should result in an increased ‘quality of life’. There are a number of quality of life measures available, but probably the best – and most practical – for routine use is the ‘Manchester Short Assessment of Quality of Life’ (MANSA) (Priebe et al., 1999). This has been specifically developed for use in a British context. It has good psychometric properties and has been used extensively to evaluate changes following the introduction of various service developments. It measures both objective aspects of quality of life (work, finances, social support, accommodation, safety, leisure, family, physical and mental health) and subjective satisfaction with these aspects of social adjustment. It is a very good instrument, but it does take time to administer and is probably best viewed as a research tool, rather than as a routine outcome measure. Notwithstanding, with the right kind of electronic support, it could be introduced as part of routine reviews.
The other measure which is related to ‘quality of life’ and is becoming increasingly popular is the ‘Warwick and Edinburgh Mental WellBeing Scale’ (WEMWBS) (Tennant et al., 2007). This was designed as a measure of positive mental health primarily for use in population surveys. It consists of 14 items, each rated on a 5 point scale, referring to the person’s experience over the last two weeks. It has good test-retest reliability and shows sensitivity to change. It also has high internal consistency and low social desirability bias. The WEMWBS is a good measure, but it was not developed as a measure of ‘recovery’ and the items are therefore not phrased using recovery language. They are also very similar to items contained in general measures of psychological distress and the WEMWBS correlates quite highly with these kinds of instruments (e.g. +0.53 with the GHQ-12).
‘Well-being’ should also not be assumed to be the same as ‘quality of life’. Connell et al. (2012) in an important paper based on a synthesis of qualitative research on quality of life for people with mental health problems concluded that it includes ‘well-being’, but this was only one element in the construct. A number of other dimensions were also important including: subjective sense of control (particularly regarding distressing symptoms), feelings of autonomy and choice, a positive self-image, a sense of belonging, engagement in meaningful and enjoyable activities and feelings of hope. There are obvious similarities between these dimensions and basic recovery principles (hope, control, opportunity).
RECOVERY OUTCOME DOMAIN 6 – Service use
Finally, we come to the controversial question of whether reduced use of mental health services can be used as an indicator of ‘recovery’. The focus of recovery is on building a meaningful and satisfactory life and it can be argued that this is going to be difficult if the person is heavily dependent on mental health services (e.g. in hospital for long periods). However, simply reducing use of services cannot be justified as an indicator of facilitating recovery. Of course, use of ineffective or unnecessary services should be reduced, but it depends on the individual just how important formal services are to their recovery. Reduced use of services may therefore be an indicator of recovery for some people, but it must be a consequence, not a cause. It also cannot be used on its own and should only be interpreted in the context of the other kinds of measures we have been discussing here.
In terms of measuring these service-related indicators, most are covered in the NHS Outcomes Framework (Department of Health, 2010), and the Mental Health Minimum Data Set (Health & Social Care Information Centre, 2013). Relevant items might be:
- number of inpatient admissions
- average length of stay
- time detained under MHA in hospital
- subject to Supervised Community Treatment Order (CTO)
- number of face-to-face community contacts with psychiatrists
- number of face-to-face community contacts with CPN or care coordinator
- number of face-to-face community contacts with other health professionals.
Outcomes for staff
There is another set of outcomes which may result from adopting more recovery-oriented approaches to mental health services. These concern the potential health benefits for staff. It is estimated that mental health problems among staff account for more than a third of sickness absence in the NHS (Health Service Journal, 2013a) and, given the overall cost of sickness and absence in 2012/13 was £1.55 billion (NHS Employers, 2013), this amounts to approximately half a billion pounds (£500,000,000) lost to the NHS as a whole through mental health issues in the workforce. If progress towards more recovery-oriented services could reduce these figures then there are clearly huge potential benefits in terms of improved health for staff and reduced costs. Is this feasible?
At the moment we simply don’t know. There is little formal research specifically relating to the impact of more recovery-oriented services. However, anecdotal evidence suggests that staff frequently report how much they like working in ways to support recovery – it allows them to do the things they came into the job to do: ‘it just feels right.’ Our impression is therefore that working in recovery-focused ways can reduce sickness and absence and improve job satisfaction for staff (e.g. see Health Service Journal, 2013b).
Recovery-oriented organisations should also apply the same principles to support those employed to deliver the services as they do to those using them. We are currently building a repertoire of Human Resources, Occupational Health and workforce approaches based on recovery principles and aimed at increasing job satisfaction and reducing work-stress related sickness. These approaches will be the subject of a forthcoming briefing paper. In the meantime, the potential benefits for staff – and for organisations – from adopting recovery-oriented principles need further systematic investigation.
Conclusions
Recovery is a complex construct and measuring quality and outcomes is therefore bound to be a complex process. This has to be acknowledged. It cannot be reduced to a single measure or practice just because this is convenient. At the heart of recovery outcomes must be the experience of the person themselves and their unique hopes and dreams for the future. In terms of measurement, this is probably still the most difficult area.
Having said this, considerable progress has been made. We are now in a position to describe in reasonable detail what constitutes an effective, ‘recovery-oriented’ service, at both an individual and an organisational level and we can support many of our conclusions with good quality evidence. The notion that, ‘Recovery sounds alright, but it’s too difficult to define and it’s not evidence-based’ is therefore not sustainable. How services may more effectively support recovery is definable. Our problem – as in many other areas of mental health services – therefore lies in implementing what we know to be important, rather than not knowing what this is.
Similarly, despite all the methodological problems, we can agree on a simple framework for recovery outcomes. This includes an improved experience of care, support for individual and socially-valued goals and enhanced feelings of hope and control. What we now need to do is to agree on the details of these broad domains and develop practical systems for routinely collecting the necessary information to monitor these outcomes.
There are also arguments for considering attempts to measure ‘quality of life’ and ‘well-being’, but these are less strong. We must also be clear that they are not the same thing. Comprehensive measures of quality of life are likely to have a strong relationship with subjective measures of recovery, but narrow measures of well-being will not. Measures of recovery outcomes based on service use also have some value, but only taken in the context of other measures. We should surely be aiming for people to be less dependent on services, but we should be aiming to do this by supporting their choices, not by forcing ‘choices’ upon them.
So, much remains to be done. In the current climate we will undoubtedly continue to suffer the familiar round of changes to the structure and functions of different parts of health and social care – ‘stirring the pot’ in a different direction – combined with severe overall restrictions on funding which now look likely to persist into the foreseeable future. We therefore need to think of how we are going to pursue the goals of establishing more ‘recovery-supporting’ services using methods which go beyond simply ‘salami slicing’ existing services. We may need to start to consider reforms, including in relation to the workforce and the balance between ‘peer support’ staff and traditional mental health professionals. Questions about outcomes and cost-effectiveness will be central to these debates.
Recommendations
- For health and social care providers
- Acknowledge that defining ‘quality’ in services to support recovery for people with mental health problems is not simple or one-dimensional.
- Recognise that recovery is based on simple, human needs: to have hope for the future, to feel somewhat in control of your life and to be able to have access to the ordinary things that make life meaningful – somewhere to live, something to do, someone to care about you, and a feeling that you are a part of society, not excluded from it.
- Ensure that all staff are managed not just in terms of their technical competence in delivering ‘evidence-based’ interventions which will support these goals, but also their ability to form honest and respectful relationships with the people using services.
- Give consistent messages to staff that support for recovery is a priority and that this can be achieved without significant additional costs.
- Encourage staff to think beyond the traditional roles of ‘expert professionals’ and ‘passive patients’ and work together with the people who use services to ‘co-produce’ services which support recovery outcomes.
- Encourage boards to ensure that recovery-focused outcomes are given priority throughout their organisations.
- Using the outcome framework described in this paper, agree specific measures with service users and carers to be used locally which adequately reflect recoveryoriented outcomes and establish practical systems for routinely collecting this information.
- For health and social care commissioners
- Recognise that supporting recovery is complex and cannot be reduced to a single quality or outcome measure, no matter how superficially attractive this might appear.
- Look for evidence that providers place emphasis on improving the process of care (quality of experience) in addition to the delivery of evidence-based interventions aimed at securing specific outcomes.
- Notwithstanding 2.2 above, look for evidence that local providers are offering a number of key service developments – peer support workers, recovery colleges, shared decision-making, supported self-management, Individual Placement and Support (IPS), ‘No Force First’ – which are likely to lead to desirable, recovery-focused outcomes.
- Recognise that the application of key recovery principles – ‘expert patient’, personalisation, choice, importance of self-management and shared decisionmaking – are common to the effective management of long-term conditions in both mental and physical health services.
- Recognise that these ‘long-term condition management’ models require an emphasis on supporting people to achieve social (life) goals in addition to symptom management.
- Using the outcome framework described in this paper, agree specific measures to be used locally with providers, service users and carers which adequately reflect recovery-oriented outcomes and establish practical systems for routinely collecting this information.
- For government and NHS England
- Ensure that ‘transactional models’ of health care delivery (e.g. PBR) support the central importance of the provision of effective relationships in healthcare.
- Ensure that central, regulatory bodies such as the Care Quality Commission embed a framework for delivering highquality, recovery-oriented services and recovery-focused outcomes into their mental health inspection methodology.
- Within an agreed framework for quality and outcomes for mental health services which will support recovery, encourage local commissioners and providers – and user and carer groups – to work together to agree on systems for routinely collecting and feeding back relevant information to monitor performance.
PART II. TECHNICAL APPENDIX
In this section we will present detailed technical support for a number of the conclusions and recommendations cited above. The structure replicates Part I.
Quality indicators at an individual level – Recovery-promoting relationships
Box A: NICE Quality Standards for service user experience in adult mental health (QS14 Issued December 2011)
http://publications.nice.org.uk/quality-standard-for-service-userexperience-in-adult-mental-health-qs14
Statement 1. People using mental health services, and their families or carers, feel optimistic that care will be effective.
Statement 2. People using mental health services, and their families or carers, feel they are treated with empathy, dignity and respect.
Statement 3. People using mental health services are actively involved in shared decision-making and supported in self-management.
Statement 4. People using community mental health services are normally supported by staff from a single, multidisciplinary community team, familiar to them and with whom they have a continuous relationship.
Statement 5. People using mental health services feel confident that the views of service users are used to monitor and improve the performance of services.
Statement 6. People can access mental health services when they need them.
Statement 7. People using mental health services understand the assessment process, their diagnosis and treatment options, and receive emotional support for any sensitive issues.
Statement 8. People using mental health services jointly develop a care plan with mental health and social care professionals, and are given a copy with an agreed date to review it.
Statement 9. People using mental health services who may be at risk of crisis are offered a crisis plan.
Statement 10. People accessing crisis support have a comprehensive assessment, undertaken by a professional competent in crisis working.
Statement 11. People in hospital for mental health care, including service users formally detained under the Mental Health Act, are routinely involved in shared decision-making.
Statement 12. People in hospital for mental health care have daily one-to-one contact with mental healthcare professionals known to the service user and regularly see other members of the multidisciplinary mental healthcare team.
Statement 13. People in hospital for mental health care can access meaningful and culturally appropriate activities seven days a week, not restricted to 9am to 5pm.
Statement 14. People in hospital for mental health care are confident that control and restraint, and compulsory treatment including rapid tranquillisation, will be used competently, safely and only as a last resort with minimum force.
Statement 15. People using mental health services feel less stigmatised in the community and NHS, including within mental health services.
Specific approaches
Housing First (Shelter, 2008)
Key features:
- Offers immediate (or relatively immediate) permanent accommodation for people is provided to service users directly from the streets, without the requirement of assessed housing ‘readiness’.
- There are no preconditions of treatment access or prior engagement with health services (‘housing first, not treatment first’).
- A harm-reduction approach is taken to dependency issues, abstinence is not required.
- There is a separation of access to housing from engagement with services to address health, social care and other support needs.
- Comprehensive support services are offered and brought to the service user. Typically, these include multi-disciplinary specialists, including physical and mental health workers; drug and alcohol treatment workers, employment support workers and peer workers. These are either employed within the housing agency, or brokered from communitybased services.
- Promotes consumer choice regarding engagement with services, including the right to refuse. The programme only demands that service users pay rent, abide by the tenancy conditions and agree to a visit by a support worker (usually) once a week.
- Support can ‘float away’ or return as needs arise and the housing is maintained even if the resident leaves the programme (for example through imprisonment or hospital admission).
Individual Placement with Support (IPS)
Key principles (after Becker, Drake & Concord, 1994):
- Competitive employment is the goal (whole or part-time).
- No selection criteria are used beyond expressed motivation to obtain employment, i.e. it is accessible to all those who want to work.
- There is a focus on consumer preference – ‘fitting the job to the person, not the person to the job’.
- It is based on rapid job search and placement. Thus, it minimises preemployment assessment and training (‘place-then-train’, not ‘train-then-place’).
- Relies on close working between employment specialists (ES) and clinical teams. The ES is embedded in the clinical team and takes a full-part in all its activities (attending assessment meetings, contributing to clinical reviews, recording in notes, etc.).
- Provides individualised, long-term support with continuity.
- Includes access to expert benefits (pensions) advice.
Quality indicators at an organisational level
Burgess et al. (2011) recommended measures to assess the quality of recovery-oriented organisations:
- Recovery-Oriented Systems Indicators (ROSI) – This is a 65 item questionnaire consisting of two sections: (a) the Adult Consumer Self-report Survey (n=42 items) and the Administrative Data Profile (n=23 items). It is psychometrically quite sound, but it is also long and laborious and not well suited for routine use.
- Recovery Self Assessment (RSA) – This was developed on the basis of an extensive review undertaken by service users and providers. It comprises five factors: (a) ‘Is the service focused on user-defined life goals’?; (b) ‘Does it involve service users in the development and provision of programmes?’; (c) ‘Does it offer a diversity of treatment options?’; (d) ‘Are service users’ choices respected by staff and is coercive treatment avoided?’; and (e) ‘Are services individually-tailored to different cultures and interests and are active attempts are made to connect with the local community?’ The instrument has good internal consistency and face validity, but there are some doubts regarding its cross-cultural applicability.
- Recovery-Oriented Practices Index (ROPI) – This was developed by Mancini & Finnerty (2005) in New York but has been adapted for use in a British context as the ‘Scottish Recovery Indicator’. It consists of eight dimensions, each containing a number of specific items which are rated on a five-point scale from ‘absence’ to ‘full adherence’. The ratings are made by mixed groups of staff and service users working together to arrive at a consensus. The SRI contains areas which are clearly linked to achieving a more recovery-oriented service, but also contains dimensions which simply reflect basic good practice. There is little evidence regarding its psychometric properties.
- Recovery Promotion Fidelity Scale (RPFS) – This was developed specifically to assess the degree to which mental health agencies incorporate key recovery principles and practices into their services and operations. The development involved a series of focus groups consisting of service users, carers, managers and clinicians. The final analysis produced 12 items, organised into five domains, each corresponding to a different area of recovery practice. The instrument is intended to guide self-assessments of recovery practice in community agencies and the authors acknowledge that further research is now required to investigate the relationship between the items and recovery outcomes.
The ImROC ‘10 key challenges’ – content validity
Le Boutillier et al. (2011) reviewed 30 international documents offering guidance for recovery-oriented practice and found four key domains. These were:
- Working relationships – Practitioners demonstrate a genuine desire to support individuals and their families to fulfil their potential and to shape their own future. A therapeutic relationship is essential in supporting recovery where partnership working and hope is promoted.
- Supporting personally defined recovery – Practitioners focus on personally defined recovery and view recovery at the heart of practice and not as an additional task. Individuals are supported to define their own needs, goals, dreams and plans for the future to shape the content of care. Individuality, informed choice, peer support, strengths focus, and holistic approach are contained in this practice domain.
- Organisational commitment – Organisations that support recovery demonstrate a commitment to ensure that the work environment and service structure is conducive to promoting recovery-oriented practice. The organisational culture gives primacy to recovery, focuses on, and adapts to, the needs of people rather than those of services. Recovery vision, workplace support structures, quality improvement, care pathway and workforce planning sit within this practice domain.
- Promoting citizenship – The core aim of services is to support people who live with mental illness to reintegrate into society and to live as equal citizens. Citizenship is central to supporting recovery, where the right to a meaningful life for people living with sever and enduring mental illness is advocated. Seeing beyond service user rights, social inclusion and meaningful occupation are grouped in this practice domain.
These domains map onto the ‘10 key challenges’ as shown in Box B.
Box B: ImROC ‘10 key challenges’ and Le Boutillier et al’s key domains of recovery-supportive practice
Outcomes
DOMAIN 1 – Quality of recovery-supporting care – INSPIRE (Williams et al., 2011)
21 items with two sub-scales ‘Support’ and ‘Relationships’. The former tries to assess whether particular types of recovery support are important to the service user (hope, understanding, building on strengths, etc.) and whether she/he feels these are provided by their current mental health worker. The latter asks questions about the general quality of the helping relationship (feels listened to, respect, positive belief in recovery.
Although INSPIRE is already quite a short instrument, discussions with Professor Slade suggest that it could be amended to an even shorter form using the ‘CHIME’ conceptual framework for recovery – Connectedness, Hope, Identity, Meaning and Empowerment – derived by Leamy et al. (2011) based on a systematic literature review and narrative synthesis. This is shown in Box C below. Further information is available from: www.researchintorecovery.com/inspire
Box C: Suggestions for a short version of the INSPIRE scale using the CHIME dimensions (Leamy et al., 2011)
DOMAIN 2 – Achievement of individual recovery goals – ‘Goal Attainment Scaling’ (GAS) developed by Kirusek & Sherman (1968)
A worked example is given in Box D.
Box D: An example of Goal Attainment Scaling
DOMAIN 3 – Subjective measures of personal recovery
Burgess et al. (2011) recommended measures to assess the subjective recovery outcomes.
- Recovery Assessment Scale (RAS) – assesses hope, willingness to ask for help, illness management, goal-orientation and self-determination (24 items).
- Illness Management and Recovery Scales (IMR) – assesses knowledge about illness, medication and side-effects, coping strategies and relapse prevention, symptom management (15 items).
- Stages of Recovery Instrument (STORI) – based on characterising the person’s a ‘stage’ of recovery using a model comprising ‘moratorium’, ‘awareness’, ‘preparation’, ‘rebuilding’ and ‘growth’ (50 items).
- Recovery Process Inventory (RPI) – assesses anguish, connectedness to others, confidence/purpose, living situation, care/help from others, hopefulness/help for self (22 items).
We would add for consideration:
The Questionnaire about Process of Recovery (QPR) (Neil et al, 2009) consists of 22 items, each rated on a five-point scale, which break down into two factors ‘intrapersonal’ (n=17 items) covering such items as “I feel that my life has a purpose” and “I can take charge of my life”; and ‘interpersonal’ (n= 5 items) covering items such as: “Meeting people who have had similar experiences makes me feel better” and “My recovery has helped challenge other peoples’ views about getting better”.
REFERENCES
Alakeson, V. & Perkins, R. (2012) Personalisation and Personal Budgets. ImROC Briefing paper 2. London: Centre for Mental Health.
Ashcraft, L., Bloss, M. & Anthony, W.A. (2012). The Development and Implementation of “No Force First” as a Best Practice. Psychiatric Services, 63, 415 – 417.
Baker, E., Fee, J., Bovingdon, L., Campbell, T., Hewis, E., Lewis, D., Mahoney, L. & Roberts, G. (2013) From taking to using medication: recovery-focussed prescribing and medication management. Advances in Psychiatric Treatment, 19, 2-10.
Becker, D.R., Drake, R.E. & Concord, N.H. (1994) Individual placement and support: a community mental health center approach to vocational rehabilitation. Community Mental Health Journal, 30, 193-206.
Bird, V., Leamy, M., Le Boutillier, C., Williams, J., & Slade, M. (2011) REFOCUS: Promoting recovery in community mental health services. London: RETHINK.
Boardman, J. & Friedli, L. (2012) Recovery, Public Mental Health and Wellbeing. ImROC Briefing paper 3. London: Centre for Mental Health.
Boardman, J., Slade, M. & Shepherd, G. (2013) Assessing recovery – seeking agreement about key domains. Unpublished report for the Department of Health. London: Centre for Mental Health, 134-138 Borough High Street, SE1 1LB.
Boardman, J. & Roberts, G. (in press) Risk, Safety and Recovery. ImROC Briefing paper. London: Centre for Mental Health, NHS Confederation.
Bond, G.R., Drake, R.E. & Becker, D. (2008) An update on randomized controlled trials of evidence-based supported employment. Psychiatric Rehabilitation Journal, 31, 280-290.
Bora, R., Leaning, S., Moores, A. & Roberts, G. (2010) Life coaching for mental health recovery: the emerging practice of recovery coaching. Advances in Psychiatric Treatment, 16, 459-467.
Borg, M. & Kristiansen, K. (2004) Recoveryoriented professionals: Helping relationships in mental health services. Journal of Mental Health, 13, 493-505.
Burns, T., Catty, J., Becker, T., Drake, R., Fioritti, A., Knapp, M., Lauber, C., Tomov, T., Busschbach, J. v., White, S. & Wiersma, D. (2007) The effectiveness of supported employment for people with severe mental illness: a randomised controlled trial. The Lancet, 370, 1146-1152.
Burgess, P., Pirkis, J., Coombs, T. & Rosen, A. (2011) Assessing the value of existing recovery measures for routine use in Australian mental health services. Australian and New Zealand Journal of Psychiatry, 45, 267-280.
Connell, J., Brazier, J.E., O’Cathain, A., Lloyd-Jones, M. and Paisley S. (2012) Quality of life of people with mental health problems: a synthesis of qualitative research. Health and Quality of Life Outcomes, 10:138. DOI: 10.1186/1477-7525-10-138. URL: http://www.hqlo.com/content/10/1/138
Copeland, M.E. (2011) Wellness Recovery Action Plan (WRAP). http://mentalhealthrecovery.com/store/wrap.html
Davies, S., Wakely, E., Morgan, S. & Carson, J. (2012) Mental health recovery heroes past and present. A handbook for mental health care staff, service users and carers. Brighton: Pavilion Press.
Deegan, P.E. & Drake, R.E. (2006) Shared Decision Making and Medication Management in the Recovery Process. Psychiatric Services, 57, 1636-1639.
Department of Health (2007) Independence, choice and risk: a guide to best practice in supported decision-making. http://webarchive.nationalarchives.gov.uk/ 20130107105354/http://www.dh.gov.uk/en/ Publicationsandstatistics/Publications/ PublicationsPolicyAndGuidance/DH_074773
Department of Health/HMG (2011) No health without mental health: a cross-government mental health outcomes strategy for people of all ages. London: Department of Health. http://www.dh.gov.uk/mentalhealthstrategy
Department of Health (2013a) The NHS Outcomes Framework 2014-15. London: Department of Health. https://www.gov.uk/ government/publications/nhs-outcomes-framework-2014-to-2015
Department of Health (2013b) The 2014/2015 Adult Social Care Outcomes Framework. London: Department of Health. https://www. gov.uk/government/publications/adult-socialcare-outcomes-framework-2014-to-2015
De Silva, D. (2011) Helping people help themselves. London: The Health Foundation. http://www.health.org.uk/publications/ evidence-helping-people-help-themselves/
Dickens, G., Weleminsky, J., Onifade, Y. & Sugarman, P. (2012) Recovery Star: validating user recovery. The Psychiatrist, 36, 45-50.
Dinnis, S., Roberts, G., Hubbard, C., Hounsell, J. & Webb, R. (2007) User-led assessment of a recovery service using DREEM. Psychiatric Bulletin, 31, 124-127.
Foster, G., Taylor, S.J.C., Eldridge, S., Ransay, J. & Griffiths, C.J. (2007) Selfmanagement education programmes by lay leaders for people with chronic conditions. Cochrane database of Systematic Reviews Issue 4. Art. No.: CD005108.
Francis, R. (2013) The Mid Staffordshire NHS Foundation Trust Public Inquiry Final report. http://www.midstaffspublicinquiry.com/report
Goldberg, D. & Williams, P. (1988) A users guide to the General Health Questionnaire. Slough: NFER-Nelson.
Greenhalgh, T. & Hurwitz, M. (1999) Narrative based medicine: Why study narratives? British Medical Journal, 318, 48-50.
Hacking, S. & Bates, P. (2008). The Inclusion Web as a tool for person-centred planning and service evaluation. Mental Health Review Journal: Research, Policy and Practice, 13, 4-15.
Hampson, M., Killaspy, H., Mynors-Wallis, L. & Meier, R. (2011) Outcome measures recommended for use in adult psychiatry, Royal College of Psychiatry Op 78, June 2011.
Hasson-Ohayon, I., Roe, D. & Kravetz, S. (2007) A Randomized Controlled Trial of the Effectiveness of the Illness Management and Recovery Program. Psychiatric Services, 58, 1461-1466.
Health & Social Care Information Centre (2013) Mental Health Minimum Dataset (MHMDS) Specifications and Guidance v4.1. http://www.hscic.gov.uk/mhmds/spec
Health Services Journal (2013a) Why It’s Time to Help the Helpers. Mental Health Supplement, 6 December, 2-3.
Health Services Journal (2013b) Spelling It Out Loud And Clear. Mental Health Supplement, 6 December, 4-5.
Henderson, C., Flood, C., Leese, M., Thornicroft, G., Sutherby, K. & Szmukler, G. (2004) Effect of joint crisis plans on use of compulsory treatment in psychiatry: a single blind randomised controlled trial. British Medical Journal, 329, 136-138.
Henderson, C., Flood, C., Leese, M., Thornicroft, G., Sutherby, K. & Szmukler, G. (2008) Views of service users and providers on joint crisis plans. Social Psychiatry Psychiatric Epidemiology. Published online 4 October 2008. DOI 10.1007/s00127-008- 0442-x.
Howard, L.M., Heslin, M., Leese, M., McCrone, P., Rice, C., Jarrett, M. & Spokes, T. (2010) Supported employment: randomised controlled trial. British Journal of Psychiatry, 196, 404-411.
Hill, L., Roberts, G. & Igbrude, W. (2010) Experience of support time and recovery workers in promoting WRAP. The Psychiatrist, 34, 279-284.
Hurn, J., Kneebone, I. & Cropley, M. (2006) Goal setting as an outcome measure: a systematic review. Clinical Rehabilitation, 20, 756-772.
King, L., Robb, J., Riley, D., Benson, I. & Tyrer, K. (2013) NO FORCE FIRST – Changing the culture to create coercion-free environments. Presentation to ImROC Learning Set, 11/12/13, Manchester. London: www.ImROC.org
Kirusek, T.J. & Sherman, R.E. (1968) Goal Attainment Scaling: A General Method for Evaluating Comprehensive Community Mental Health Programs. Community Mental Health Journal, 4, 443-453.
Latimer, E. (2010) An effective intervention delivered at sub-therapeutic does becomes an ineffective intervention. British Journal of Psychiatry, 196, 341-342.
Leamy, M., Bird, V., Le Boutillier, C., Williams, J. & Slade, M. (2011) Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. British Journal of Psychiatry, 199, 445-462.
Le Boutillier, C., Leamy, M., Bird, V., Davidson, L., Williams, J. & Slade, M. (2011). What does recovery mean in practice? A qualitative analysis of international recovery-oriented practice. Psychiatric Services, 62, 1470-1476.
McColl, A., Roderick, P., Gabbay, J. et al. (1998) Performance Indicators for primary care groups: an evidence based approach. British Medical Journal, 317, 1354-1360.
McKeith, J. & Burns, S. (2010) The Recovery Star: User Guide (Second Edition). London: Mental Health Providers Forum. www.mhpf.org.uk
Mueser, K.T., Corrigan, P.W., Hilton, D.W., Tanzman, B., Schaub, A., Gingerich, S., Essock, S.M., Tarrier, N., Morey, B., VogelScibilia, S. & Herz, M.I. (2002) Illness, Management and Recovery: A Review of the Research. Psychiatric Services, 53, 1272-1284.
Mueser K.T., Meyer, P., S., Penn, D., L., Clancy, R., Clancy, D.M., & Salyers, M. (2006) The Illness, Management and Recovery Program: Rationale, Development, and Preliminary Findings. Schizophrenia Bulletin, 32 (suppl 1), S32 – S43.
Neil, S.T., Kilbride, M., Pitt, L., Nothard, S., Welford, W., Sellwood, W., Morrison, A.P. (2009) The questionnaire about the process of recovery (QPR): A measurement tool developed in collaboration with service users. Psychosis, 1, 145-155.
Newman-Taylor, K., Herbert, L. & Woodfine, C. (in press) Are we Delivering RecoveryBased Healthcare? Psychology Academic Unit, University of Southampton, SO17 1BJ. knt@soton.ac.uk
NHS Confederation/Centre for Mental Health (2012) Supporting Recovery in mental health, Briefing paper, Issue 244. London: NHS Confederation.
NHS Employers (2013) 2012-2013 NHS Sickness and absence figures. http://www.nhsemployers.org/ HealthyWorkplaces/LatestNews/Pages/ StaffSicknessFiguresReleased.aspx
NICE (2011) Quality standard for service user experience in adult mental health. Issued December 2011. http://publications.nice.org.uk/ quality-standard-for-service-user-experience-inadult-mental-health-qs14/list-of-statements
NICE (2013) Service user experience in adult mental health services overview. http://pathways.nice.org.uk/pathways/serviceuser-experience-in-adult-mental-healthservices
O’Connor, A.M., Stacey, D. & Legere, F. (2008) Coaching to support patients in making decisions. British Medical Journal, 336, 288.
Padgett, D., Gulcur, L., & Tsemberis, S. (2006) Housing first services for people who are homeless with co-concurring serious mental illness and substance abuse’. Research on Social Work Practice, 16, 74-83.
Parsonage, M. (2013) Welfare advice for people who use mental health services. London: Centre for Mental Health.
Perkins, R. (2012) UK mental health policy development: a counter-argument deriving from users’ experiences, in P. Phillips, T. Sandford & C. Johnston, C. (Eds), Working in Mental Health: Practice and Policy in a Changing Environment. Oxford: Routledge
Perkins, R. & Rinaldi, M. (2007) Taking back control: A guide to planning your recovery. London: Southwest London & St. George’s Mental Health NHS Trust, Trust Headquarters, Springfield University Hospital, 61 Glenburnie Road, London SW17 7DJ.
Perkins, R., Repper, J., Rinaldi, M. & Brown, H. (2012) Recovery Colleges, ImROC, Briefing 1. London: Centre for Mental Health.
Priebe, S., Huxley, P., Knight, S. & Evans, S. (1999) Application and results of the Manchester short assessment of quality of life (MANSA). International Journal of Social Psychiatry, 45, 7-12.
Rapp, C. & Goscha, R.J. (2006) The Strengths Model: Case Management With People With Psychiatric Disabilities, 2nd Edition. New York: Oxford University Press.
Repper, J. (2013a) Peer Support Workers: Theory and Practice, ImROC Briefing Paper 5. London: Centre for Mental Health and Mental Health Network, NHS Confederation.
Repper, J. (2013b) Peer Support Workers: A Practical Guide to Implementation, ImROC Briefing Paper 7. London: Centre for Mental Health and Mental Health Network, NHS Confederation.
Repper, J. & Carter, T. (2011) A review of the literature on peer support in mental health services. Journal of Mental Health, 20, 392- 411.
Repper, J. & Perkins, R. (2003) Social Inclusion and Recovery. London: Baillière Tindall.
Rinaldi, M., Wybourn, S. & Clenehan, M. (2012) The development, piloting and outcomes from a Recovery College in England. London: Southwest London & St. George’s Mental Health NHS Trust, Trust Headquarters, Springfield University Hospital, 61 Glenburnie Road, London SW17 7DJ.
Roberts, G. (2000) Narrative and severe mental illness: what place do stories have in an evidence-based world? Advances in Psychiatric Treatment, 6, 432-441.
Sainsbury Centre for Mental Health (2009a) Doing what Works: Individual placement and support. Briefing paper 37. London: Sainsbury Centre for Mental Health.
Sainsbury Centre for Mental Health (2009b) Commissioning what Works: The economic and financial case for supported employment. Briefing paper 41. London: Sainsbury Centre for Mental Health.
Salyers, M.P., Godfrey, J.L., McGuire, A.B., Gearhart, T., Rollins, A.L. & Boyle, C. (2009) Implementing the Illness Management and Recovery Program for Consumers with Severe Mental Illness. Psychiatric Services, 60, 483-491.
SAMSHA (2010) Shared Decision-Making in Mental Health Care: Practice. Research and Future Directions. HHS Publication No. SMA-09-4371, Rockville, MD: Centre for Mental Health Services , Substance Abuse and Mental Health Services Administration. http://store.samhsa.gov/product/SharedDecision-Making-in-Mental-Health-Care/ SMA09-4371
Shanks, V., Williams, J., Leamy, M., Bird, V.J., Le Boutillier, C., & Slade, M. (2013) Measures of personal recovery: a systematic review. Psychiatric Services, 64, 974-980.
Shepherd, G., Boardman, J. & Slade, M. (2008) Making Recovery a Reality. London: Sainsbury Centre for Mental Health.
Shepherd, G., Boardman, J., & Burns, M. (2010). Implementing recovery: A methodology for organisational change. London: Centre for Mental Health.
Shelter (2008) Housing First. www.shelter.org.uk/goodpracticebriefings
Simon, D., Willis, C.E. & Harter, M. (2009) Shared decision-making in mental health. In A. Edwards & G. Elwyn (Eds.) Shared decision-making in health care: Achieving evidence-based patient choice (2nd edition pp.269-276). Oxford: Oxford University Press.
Slade, M. (2009) Personal Recovery and Mental Illness. Cambridge: Cambridge University Press.
Slade, M. & Hayward, M. (2007) Recovery, psychosis and psychiatry: research is better than rhetoric. Acta Psychiatrica Scandinavica, 116, 81-83.
Tennant, R., Hiller, L., Fishwick, R., Platt, P., Joseph, S., Weich, S., Parkinson, J., Secker, J., Stewart-Brown, S. (2007) The WarwickEdinburgh Mental Well-being Scale (WEMWBS): development and UK validation, Health and Quality of Life Outcomes, 5:63 doi:101186/1477-7252-5-63.
Thornicroft, G., Farrelly, S., Szmukler, G., Birchwood, M., Waheed, W. et al. (2013) Clinical outcomes of Joint Crisis Plans to reduce compulsory treatment for people with psychosis: a randomised controlled trial. British Journal of Psychiatry, 381, published online March 26, 2013. http://dx.doi.org/10.1016/S0140-6736(13)60105-1
Torrey, W., C. & Drake, R. (2009) Practicing Shared Decision Making in the Outpatient Psychiatric Care of Adults with Severe Mental Illnesses: Redesigning Care in the Future. Community Mental Health Journal. Published online: 08 November 2009. DOI 10.1007/ s10597-009-9265-9.
Trachtenberg, M., Parsonage, M., Shepherd, G. & Boardman, J. (2013) Peer support in mental health care: is it good value for money? London: Centre for Mental Health.
Williams, J., Leamy, M., Bird, V., Harding, C., Larsen, J., Le Boutillier, C., Oades, L. & Slade, M. (2012) Measures of the recovery orientation of mental health services: a systematic review. Social Psychiatry Psychiatric Epidemiology, 47, 1827-1835. DOI 10.1007?s00127-012-0484-y.
1 Boardman, J., Slade, M., & Shepherd, G. (2013) Assessing recovery: seeking agreement about the key domains. Report prepared for the Department of Health, Centre for Mental Health: London.
2 For a full list of members see Appendix 1.
3 Patient (and carer) experience measures are already part of the NHS contract and as from April 2014 Trusts will be required to apply the ‘Family and Friends’ test.
4 We understand that the NPS survey is currently being revised.
5 www.researchintorecovery.com/INSPIRE#s3
APPENDIX 1: MEMBERS OF THE EXPERT GROUP CONVENED TO EXPLORE THE CONSENSUS REGARDING DOMAINS OF RECOVERY OUTCOMES (DEPARTMENT OF HEALTH, 2013)
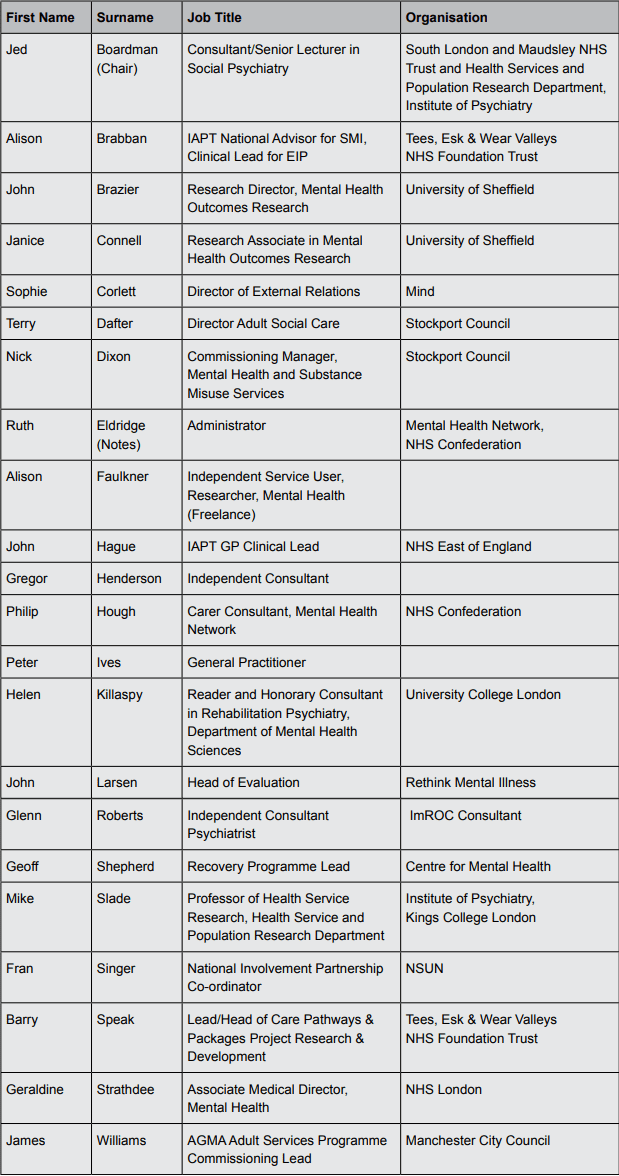
ABOUT THE AUTHORS
Geoff Shepherd
Geoff Shepherd trained originally as a clinical psychologist. He has worked most of his career in the NHS as a practitioner, manager and researcher and is currently leading the ImROC programme (Implementing Recovery through Organisational Change) based at the Centre for Mental Health and the NHS Confederation. Geoff also has a particular interest in employment issues for people with mental health problems. He holds a visiting chair at the Institute of Psychiatry and continues to be active in mental health services research.
Jed Boardman
Jed Boardman is Consultant and Senior Lecturer in Social Psychiatry at the South London and Maudsley NHS Foundation Trust and the Institute of Psychiatry. He is Senior Policy Advisor to the Centre for Mental Health and Lead for Social Inclusion at the Royal College of Psychiatrists. He has worked in community-based mental health services for most of his career. He has published widely in social and community psychiatry and helped to establish the Recovery projects at the Centre for Mental Health. Jed has been a member of the ImROC project team since its inception.
Miles Rinaldi
Miles Rinaldi is the Head of Recovery and Social Inclusion at South West London & St George’s Mental Health NHS Trust. He has been working to implement recovery-focused practice across the organisation, including setting up evidence-based employment services and opening the first Recovery College in England. Miles has worked in the voluntary sector, local authorities, and also within government on mental health policy. He has also conducted service evaluations and research with over 20 peer reviewed journal publications and book chapters. Miles has been a member of the ImROC project team since its inception.
Glenn Roberts
Glenn Roberts has worked for over 30 years as an NHS psychiatrist. He is a past academic secretary of the RCPsych Faculty of Rehabilitation and Social Psychiatry and Lead on Recovery. He has published extensively on aspects of working with people who experience psychosis and the value of narrative and stories. Glenn has a particular interest in working out how to apply recovery principles in psychiatric practice and has been a member of the ImROC project team since its inception. He continues to work for ImROC as a senior consultant.
Supporting recovery in mental health services: Quality and Outcomes
This briefing paper has been produced for the Implementing Recovery through Organisational Change programme, a joint initiative from the Centre for Mental Health and the NHS Confederation’s Mental Health Network.
The pilot phase of ImROC ran from 2011-12 and was supported by the Department of Health, together with contributions from the participating services. The continuing work of ImROC is endorsed by the Department of Health and managed and supported by the Centre for Mental Health and Mental Health Network.
For more information on the current work of ImROC, please visit imroc.org.
ImROC, c/o Mental Health Network, NHS Confederation, 50 Broadway, London, SW1H 0DB
Tel: 020 7799 6666
imroc@nhsconfed.org
imroc.org
