Traditionally, recovery concepts: hope, control and opportunity, have been considered through the lens of younger adults. ‘Continuing to be me’ – Recovering a life with a Diagnosis of Dementia is a practical and useful guide that re frames the perception of how people with dementia can continue to live meaningful and fulfilling lives. Recovery is relevant to people with dementia.
Receiving a diagnosis of dementia can have an overwhelming impact. The paper sets out a framework for understanding the personal journey of recovery with a diagnosis of dementia; from identity, impact of diagnosis, making sense of their experience to coping strategies and ways to live well.
Person-centred care and recovery-orientated practice offer possibilities for cross fertilisation of ideas and learnings. Values underpinning the principles are complementary not contradictory. Principles hold similarities through relationships and collaborative partnerships, opportunities for meaningful roles and personal growth, and viewing diversity and uniqueness as an asset and a strength.
‘Continuing to be me’ – Recovering a life with a Diagnosis of Dementia was launched at ImROC training events facilitated by Dr Rachel Perkins on Central and North West London NHS Foundation Trust Older People’s wards on 30 September 2016. ImROC works with services, systems and communities to translate the guidance from its briefing papers into local practice and experience. Through facilitation, local planning and implementation the concepts and ambitions of the briefing papers can be put in to practice.
Co-authors of the briefing paper say:
“If you are in any doubt that it’s possible to live well with dementia, read this. Research into causes and potential cures is great, but the effect of changing our attitudes to dementia, could be greater still.”
Mike Chappell, Compass Worker Lead, Mental Health Services for Older People, Nottinghamshire Healthcare NHS Foundation Trust
“One of the hardest parts of my job is telling people they have dementia. I long for the day when the fear following diagnosis can be replaced with hope. It’s not easy living with dementia but it is possible to live well and achieve goals. I hope this paper will be the first step on a journey to rethinking what it means to have dementia. It is a stimulating and inspiring read for people with dementia, their family and friends and health care professionals.”
Laura Hill, Consultant Psychiatrist, Older People’s Mental Health, Devon Partnership NHS Trust
“A practical, informative and radical paper that challenges prevailing assumptions and narratives of dementia. From ‘living death’ to ‘living well’, from ‘victims’ to be pitied to ‘citizens’ with rights who can and should speak for themselves.”
Rachel E. Perkins BA, MPhil (Clinical Psychology), PhD, OBE, Senior Consultant, ImROC, Co-editor of ‘Mental Health and Social Inclusion’ Journal, Deputy Chair, Equality and Human Rights Commission Disability Committee
“Recovering & discovering a life with dementia – for the individual, those around them & those supporting them – is so much more than making sense of facts and information that is readily available.
This briefing draws on the invaluable personal experiences of those who can inform, guide and inspire all concerned; to ensure those who receive a diagnosis of some form of dementia can ‘continue to be me’ and remain valued, participatory citizens; & who will continue to help shape services.”
Jane Rennison, Trust Head of OT & Recovery Lead, Central & North West London NHS Foundation Trust
“We know that from talking to people with dementia and their carers that the principles which underpin the concept of recovery do have meaning and resonance with them. People with dementia want to remain in the driving seat of their own life, and to continue to do things which give life purpose and re-enforce a sense of who they are. Recovery-oriented practice is equally important for dementia services, even if the language is problematic, this briefing is intended to help services to think about how they can apply these principles in practice.”
Dr Stephanie Daley, Clinical Research Fellow, Centre for Dementia Studies, Brighton and Sussex Medical School
Download 12. ‘Continuing To Be Me’ – Recovering a Life with a Diagnosis of Dementia
12. ‘Continuing To Be Me’ – Recovering a Life with a Diagnosis of Dementia
Rachel Perkins, Laura Hill, Stephanie Daley, Mike Chappell and Jane Rennison
INTRODUCTION
The purpose of this briefing paper is to explore what ‘recovery’ might mean for those with a diagnosis of dementia.
Ideas about recovery have typically focused on younger adults, and have not considered people living with progressive conditions for which there is no known ‘cure’. However, recovery is essentially the process of rebuilding your life following events that ‘knock the bottom out of your world’. A diagnosis of dementia is certainly, for most people and those who are close to them, a devastating and life changing event. Images of a decent life with dementia are few and far between. In this briefing paper, our aim is to contribute to changing the narrative from ‘living death’ to ‘living well’: to show how many people have found ways of living a meaningful and fulfilling life with a diagnosis of dementia. Recognising some of the parallels between ‘recovery focused practice’ and ideas about ‘person centred care’, we explore what enables people to regain hope and live positively, maintain personal control and have the opportunity to do the things they value, remain a valued part of their community and participate not as victims, but as citizens.
The Impact of Diagnosis
For most people, a diagnosis of dementia is a devastating and life-changing experience for both the individual and the family and friends who are close to them.
“I felt totally alone, with the world receding from me in every direction and you could have used my anger to weld steel.” (Pratchett, 2008)
“Not only is it painful to realise that someone you love has dementia, but it can also be hard to accept that your life may need to change quite considerably.” (in Pratt and Wilkinson, 2001)2
The symptoms themselves can be difficult and frightening
“It’s as though I can’t think. It’s a mild panic.”
“One of the difficulties is that I can’t remember that I am going to forget things.”
(in Pratt and Wilkinson, 2001)
“What worries me is the fact . . . have I said something, and I’ve forgotten I’ve said it, and what worries me . . . am I saying the same thing, you know, which I think I have said before . . . that’s what worries me.” (in Caddell and Clare, 2011)
But equally difficult to deal with is the loss of the things you value…
“ The hardest thing about the whole lot is the things they took off me. All my enjoyment they took it away from me. They took my car off me, took my license off me for the car, they took my gun off me, they took my fishing off me…Everything I try to do I get shot down at, everything, everything I try or want to do, I can’t even take my granddaughter out for a walk.” (in Pratt and Wilkinson, 2001)
“I couldn’t – I can’t – I don’t cook, no. I have changed a lot in the way that I don’t cook.”
“The fact about my life is that it’s very, very shallow now . . . I wasn’t a shy person or a reclusive person at all, erm, but now . . . my lifestyle is so limited and narrow.”
(in Caddell and Clare, 2011)
…and fear of what will happen in the future as the condition worsens.
“I worry a lot really, I’m afraid and I don’t know whether will get worse. Do you know? Yeah, I worry about it.” (in Manthorpe et al, 2011)
“[I was] totally devastated. I had watched my mum when she took it … she didn’t even know who we were or anything … she hadn’t a clue … when I first heard that I was in the stages of starting it I got really terrified.”
(in Pratt and Wilkinson, 2001)
“If it gets any worse and I can’t recognise my wife or something like that.”
“… at the day centre I see people who are really bad, and they’re quite, you know, one or two are quite childish, and I would hate to get like that “
(in Caddell and Clare, 2011)
Given the overwhelming impact of the diagnosis, it is all too easy for the person, and those close to them, to feel completely hopeless about themselves and their possibilities. Everyone with a diagnosis of dementia faces the challenge of finding a way of living a meaningful and fulfilling life after the initial impact of the diagnosis. This challenge is often compounded by age discrimination: ideas that the person has ‘had a good innings’ and prevailing societal beliefs that older people have little to contribute and constitute a burden on their kinfolk in particular and on society in general. Too often, older people experience loss of valued roles following retirement, deteriorating physical health and physical impairment, reduced social networks and the death of friends and partners3. According to Age UK (Davidson and Rossall (2014) more than a million older people say they only, or always feel lonely. 49% of people over 65 say that their television or their pets are their main forms of company; 17% have less than weekly contact with family friends and neighbours and 11% have less than monthly contact. Over half go for over a month without speaking to a friend, neighbour or family member. Loneliness matters: not only does it reduce a person’s quality of life, it is as harmful to health as smoking 15 cigarettes per day (Holt-Lunstad et al, 2010) and people with a high degree of loneliness are twice as likely to develop Alzheimer’s ( Wilson et al, 2007; Holwerda et al, 2014). Among those with dementia, a survey of over 500 adults by Alzheimer’s Society (2013) reports that 38% say they are lonely and 70% have stopped doing things they used to do after diagnosis.
For those with a diagnosis of dementia the challenge is amplified by popular characterisations of dementia. Peel (2014) describes a ‘panic-blame’ framework demonstrated in media consideration of dementia. This is encapsulated in the headlines of two British newspapers: the Daily Mail (Revoir, 2011) talked of “The living death of Alzheimers’, while the Express proclaimed “Take a walk to keep dementia at bay” (Fletcher, 2010). On the one hand there is the view of dementia as something that “sneaks up on unsuspecting victims and is therefore an indiscriminate invader of older people’s lives” (Peel, 2014): ‘a living death’ with panic laden talk of an ‘epidemic’ or ‘tsunami’ of dementia. On the other hand there is a discourse around personal responsibility – “a blame discourse [that] coheres around constructing dementia onset as a function of individual behaviour” (Peel, 2014). Adopt a healthy life-style (intellectual stimulation, drinking, eating, weight, physical activity) and keep dementia at bay. These are summarised in Carper’s 2011 book 100 Simple Things You Can Do to Prevent Alzheimer’s and AgeRelated Memory Loss’.
Rebuilding a life with a diagnosis of dementia is not easy, and it is made more difficult by such negative and blaming constructions of dementia. Seldom heard are the voices of people living with a diagnosis of dementia which could serve to challenge these popular representations.
“Understanding the impacts this discourse does and will increasingly have on different individuals and groups, and how it may be challenged or reclaimed will be important in generating positive social change for people living with dementia and their carers.” (Peel, 2014)
Caddell and Clare (2011) show how, in the early stages of dementia, people appeared to be in a state of flux, experiencing both continuity and change in their sense of identity “…participants felt that little had changed with respect to their identities as a whole, but most identified features of themselves that were different than they had been prior to the onset of dementia.”
There may be no way back to how things were before, but many people with a diagnosis of dementia and their families have shown that a decent life with dementia is possible4.
“I can reassure you that, however it may feel at the beginning, it is still possible to live a life of quality with dementia. Not the life you had before, perhaps, but a life full of promise…” (James McKillop 2005 in Still Going Strong)
“With willing and dedicated support from her extended family, she enjoyed an excellent quality of life at the centre and head of her family, right up until her death at home from vascular dementia.” (Mike Chappell, Compass Worker Lead)
Recovering a life with a diagnosis of dementia
Ideas about recovery have typically focused on younger adults. With some notable exceptions (for example, Woods, 2007; Hill et al, 2010; Adams, 2010; McKay et al, 2012; Daley et al, 2013), there has been little attention paid to older people, especially those who are living with dementia. As Woods (2007) has argued, the applicability of concepts of recovery to older people with functional mental health problems is clear, but at first sight, ideas about ‘recovery’ may seem incompatible with a progressive and ultimately fatal health condition such as dementia. However, this discordance applies only if recovery is viewed in clinical terms of ‘getting better’ and ‘cure’. The process of recovery is not about ‘recovering from an illness’ but ‘recovering a life’ (Deegan, 1988; Anthony, 1993; Repper and Perkins, 2012): the lived, or real life experience as the person accepts and overcomes the challenge of what has happened and recovers a new sense of self and purpose within and beyond the limits of disability (Deegan, 1988). Recovery is “a way of living a satisfying, hopeful and contributing life even within the limitations caused by illness … a deeply personal, unique process … recovery involves the development of new meaning and purpose in one’s life as one grows beyond the catastrophic effects of illness.” Anthony (1993) makes it clear that recovery is not the same as cure and is not restricted to mental health problems. It is a common human challenge faced by anyone who is affected by any form of illness or other traumatic and life changing events.
“Successful recovery from a catastrophe does not change the fact that the experience has occurred, that the effects are still present, and that one’s life has changed forever. Successful recovery does mean that the person has changed, and that the meaning of these facts to the person has therefore changed. They are no longer the primary focus of one’s life. The person moves on to other interests and activities.” (Anthony, 1993)
A diagnosis of dementia is certainly a catastrophic and life-changing event for the individual and those who are close to them, and everyone affected faces the challenge of recovery.
“Even for conditions where there is as yet no cure, as with dementia, improvements in care and treatment are achievable ….’Recovery’ and well-being approaches … are equally applicable to older people. ‘Recovery’ does not imply ‘cure’, but builds on the personal strengths and resilience of an individual … Recovery is about the development of coping skills, and about social inclusion, making it possible for people to have quality of life and a degree of independence and choice, even those with the most enduring and disabling conditions.” (Social Care Institute for Excellence, 2006).
Recovery does not mean that all problems have disappeared: “Life isn’t about waiting for the storm to pass…It’s about learning to dance in the rain.” (Anonymous, more recently attributed to Vivian Greene5). Neither is it a professional treatment or intervention. It is a deeply personal and individual journey of growing within and beyond what has happened to you. There is no set formula for recovery – everyone must find their own way. Recovery is an ongoing process of accommodating and moving beyond what has happened, and there will be ups and downs.
“Living with a memory problem is sometimes like living in the fog and sometimes like living in the sunshine. We have good days and bad days.” (Alzheimer’s Society online community Talking Point, 2004)6
Recovery is a journey for families and friends as well as the individual with the diagnosis. They face the challenge of helping the person they love in their own journey: their own lives are profoundly affected by the diagnosis of dementia in someone they love.
“I was shocked. Then I thought about all the plans I’d made for my retirement with my wife. I realised it would no longer be possible.” http://www. alzheimer-europe.org/Living-withdementia/After-diagnosis-What-next/ Diagnosis-of-dementia/Facing-thediagnosis
Their lives may be profoundly affected and they too must find new sources and meaning and value.
“A diagnosis of dementia has a profound impact not only on the individual, but also on those who are close to them. Essentially, the challenge of ‘Recovery’ from a diagnosis of dementia involves families discovering new sources of value and meaning for themselves, in their loved one and in their relationship with them.” (Recovery is for All. Hope, Agency and Opportunity in Psychiatry. A Position Statement by Consultant Psychiatrists, 2010)
A small survey of clinicians attending an old age psychiatry conference (Hill et al, 2010) showed that the majority thought that a recovery approach was wholly or partially applicable to people with dementia, arguing that helping them to achieve their maximum potential, focusing on abilities and enabling them to sustain valued roles are central to the provision of effective support. However, serious concerns about the term ‘recovery’ also exist. Some feel that it may foster unrealistic expectations in carers, relatives and the person with dementia; that those caring for loved ones with more advanced dementia might recoil at the language; that attempting to promote the concept of recovery could be taken to negate or undermine the devastating consequences of the global deterioration seen in dementia. Some services have preferred to use other terms such as ‘living well’ or ‘positive lives’ however, “preferred terms are less important that the values they support” (Hill et al, 2010) and there is an increasing consensus that the values underpinning a recovery approach are applicable to dementia.
“I never use the word ‘recovery’ with carers but always emphasise that there are many ways they can help the person with dementia have as good a quality of life as possible; that living with dementia doesn’t have to be awful. I also emphasise that caring with this approach is a wonderful act in itself.” (Mike Chappell, Lead Compass Worker)
It is also important to avoid adopting wholesale concepts and approaches deriving from the world of younger adults or people with other conditions. In order to understand what recovery means in the context of dementia, it is critical that we tap the wisdom and experience of people living with dementia, those who are close to them, and the individuals and services who support them to gain an insight into:
- the process of recovering a life with a diagnosis of dementia,
- what helps people in this journey,
- the different possibilities and challenges facing individuals and those who are close to them, and
- ways in which services and supports assist people in their journey.
A framework for understanding the personal journey of recovery with a diagnosis of dementia
Daley et al (2013) interviewed people with dementia (and functional mental health problems) and their relatives/carers in a South London mental health service. They performed a ‘grounded theory analysis’ which used the interview data to build a bottom-up framework for understanding the process of recovering a life with a diagnosis of dementia. This includes the following elements (adapted from Daley, 2013).
1. Identity: the person in their life.
Most people who develop dementia have a long established and enduring sense of identity: a strong sense of who they are and what matters in life, a resilience born of many years experiences of the vicissitudes of life and a wealth of coping strategies. Daley et al (2013) concluded that “recovery appeared primarily to be connected to the extent to which the preexisting sense of identity could be maintained.” (Daley et al, 2013).
“I’m still me. My memory may not be as good as it was but it doesn’t stop me from being me.”
“Support is the key to me leading as normal a life as possible. People knowing and treating me as the person I still am. Giving me room to live.”
(in Care Services Improvement Partnership, 2005)
2. Impact of diagnosis.
As already discussed, many people have described the devastating impact of a diagnosis of dementia both for themselves and for their family and friends. These extend beyond the impact of the symptoms to the loss of hopes and dreams for the future and a knowledge that your condition will become progressively worse.
“We were diagnosed over two years ago but can still remember those first shattering feelings – shock, disbelief, fear, shame, feeling cut off…and feeling very alone…” (Pat, James and Ian http://www.alzheimer-europe.org/Living-with-dementia/Afterdiagnosis-What-next/Diagnosis-of-dementia/Facing-the-diagnosis)
3. Making sense of the experience.
A diagnosis of dementia is a form of bereavement and associated with all the normal responses to loss: anger, despair, hopelessness, denial. Too often professionals focus on giving factual information about diagnosis and prognosis and practical assistance available rather than offering time and support through the emotional processing that must go on in order for people to find a way forward (Rachman, 1980).
“ … Your brain feels numb and you can’t take it all in… . But take heart, these first terrible feelings really do pass. We know – we’ve been there.” (Pat, James and Ian http://www. alzheimer-europe.org/Living-with-dementia/After-diagnosis-What-next/Diagnosis-ofdementia/Facing-the-diagnosis
Individuals and their relatives face the daunting task of making sense of, and finding meaning in, what has happened in order to move forward in their lives: Why? Why me? Who am I? What is my life about? The answers to such questions lie not in the realm of psychiatry or psychology, but in spirituality and, in the words of the Kensington and Chelsea Memory Group, ‘being philosophical’ (see Box 1). There is no way back to how things were before, but many people have found the strength to accept what has happened and keep going:
“I thought that was the end of my life, I really did. …I thought that was it, I just couldn’t see anything beyond it … but as the time goes on a bit and then you realise that it is worthwhile persevering.”
“You’ve got it, it’s gonna kill you, but not today, so let’s get on with it today and let’s get today’s enjoyment or whatever you like, and don’t think about what’s going to happen tomorrow or the next day. Live today. As I say although you’ve got it, it hasn’t killed you so get on and enjoy.”
(in Pratt and Wilkinson, 2001)
‘ I thought ‘thank god’ I like knowing, the Alzheimer’s – I know now what is me, and what is the Alzheimer’s.’ (in Daley et al, 2013)
“Memory loss makes each day a challenge but I have realised that if I don’t give up I will always conquer, I will always be able to fight.” (Smith, 2003)
The way in which a diagnosis is given and the support that people have in making sense of it and finding a way forward, are of the essence. At present there is an emphasis on providing early diagnosis and intervention (Department of Health, 2009) in order to ensure that people receive all the support and treatment that is available. Early diagnosis may be positive if accompanied by assistance to accommodate what has happened, emotionally and practically, and work out a way forward to ‘living well with dementia’. However, at present there is a widespread lack of effective post-diagnostic support. Although there are differences from place to place, too often, the reality is that, over a couple of appointments, people are given a diagnosis, a prescription and some signposting to voluntary sector organisations with a distinct lack of true ‘intervention’ or stable, long term support.
“When I was diagnosed I was frightened. I had no-one to talk to, so I became very negative … I was left on my own and I became very depressed. Very, very deep depression. As I went through this I thought to myself “depression is worse than dementia”. (Patricia, 2013 https://www.mentalhealth.org.uk/stories/patricias-story-if-youthink-old-you-will-be-old-if-you-think-young-youll-stay-young)
“Well I would have thought it would have been courtesy actually (to have a follow up appointment), but eh, because eh, the amount of questions that can come up, and if you’re looking for answers then you want to have somebody that can give you answers.” (in Pratt and Wilkinson, 2001)
In 2010, the Dementia Action Alliance, a broad based coalition in England comprising a broad range of public and voluntary sector organisations, including the Department of Health, produced a National Dementia Declaration (Dementia Action Alliance, 2010). This comprised a vision of how people living with dementia and their families should be supported, based around seven core ‘I’ statements:
- I have personal choice and control or influence over decisions about me.
- I know that services are designed around me and my needs.
- I have support that helps me live my life.
- I have the knowledge and know-how to get what I need.
- I live in an enabling and supportive environment where I feel valued and understood.
- I have a sense of belonging and of being a valued part of family, community and civic life.
- I know there is research going on which delivers a better life for me now and hope for the future.
The continuing shortcomings in postdiagnostic support mean that these ambitions – all of which are central to living well with dementia – are unlikely to be realised.
4. Continuing to be me: moving on and living well with dementia
This involves individual strategies for coping with symptoms and support from family to manage the impact of illness. However, most importantly, it also involves reinforcing identity, doing the things you value, retaining choice and control, and having people around who believe in you.
“Dementia has affected my whole family, but we have decided we are in this together now and we have to work it out. Now they understand I am really the same person.”
(in Mental Health Foundation, 2005)
“My dad’s identity was incredibly important and positive for him up until the time some of those around him started denying it. After that he deteriorated quickly. When the keys to the local church were taken off him, he went from being an active and important part of his community with a sense of purpose and a meaningful life, to a person beset by bitterness and distress. His sharp deterioration and subsequent loss of freedom followed an accident he had scaling a high wall trying to get into church. Removing the possibility of “dying with his boots on” had a profound effect on his quality of life.”
(Mike Chappell, Compass Worker Lead talking about his father)
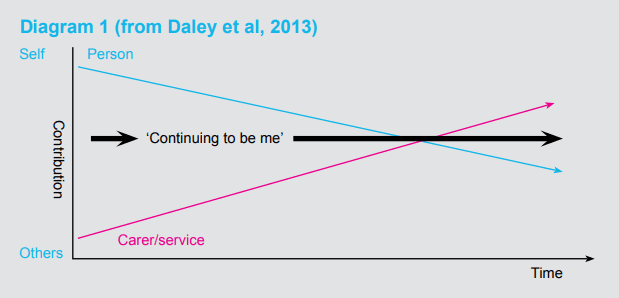
Daley et al (2013) discuss the importance of personal responsibility, connectedness and continuity in recovering a life with a diagnosis of dementia. They also emphasise the central role that relatives, friends and carers have in enabling a person to ‘continue to be me’ and the way in which this role changes over time. In the early stages people are able to take personal responsibility for managing the impact of illness and working out coping strategies that support continuity. However, as dementia progresses, the role of relatives, friends, informal carers and services increases in supporting coping strategies and enabling people to retain a sense of identity. For people with more advanced dementia, personal responsibility decreased, but where carers were able to reinforce a sense of personal identity through continuity, recovery continued to take place; the person was able to ‘continue to be me’ (see Diagram 1)
Diagram 1 (from Daley et al, 2013)
Continuing to be me: living well with dementia
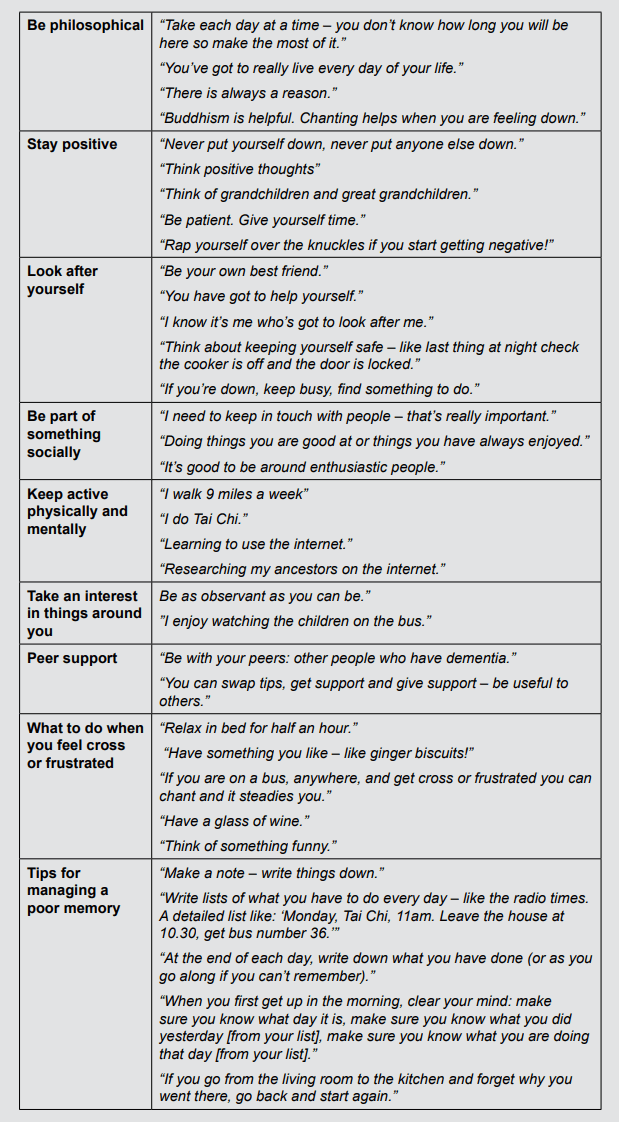
In 2014, we asked the ‘Memory Group’ in Kensington and Chelsea to think about the things that were important to them in living well with dementia. Their responses can be seen in Box 1. They talked about the need to be philosophical, stay positive, look after yourself, be part of something socially and keep physically and mentally active. They also talked about the importance of peer support and ‘self-management’: working out ways of dealing with frustration and poor memory. However, they were clear that the most important thing is to feel useful, use your skills, help other people. Feeling valued and valuable is critical.
These suggestions (see Box 1) are not dissimilar to those things identified as important by younger people facing mental health challenges: (Repper and Perkins, 2003, 2012; Shepherd et al, 2008): hope (stay positive, be philosophical, meet others facing similar challenges), personal control (look after yourself, develop strategies for dealing with frustration and poor memory) and opportunity/participation (be part of something socially, take an interest in things around you, remain active physically and mentally).
“ You need to focus on the ability and the contribution that we can make rather than what we can no longer do.”
“Being encouraged to do as much as possible keeps me going. It stops me feeling unwanted and builds my confidence” (in Care Services Improvement Partnership, 2005)
Box 1: Suggestions on living well with dementia from six people with mild to moderate dementia in the Kensington and Chelsea ‘Memory Group’ (2013)
THE MOST IMPORTANT THING: To feel useful, to be able to help others, be useful to others
“Dementia does not stop you being useful.” “Use your skills.” “Working can be good.”
“Everyone is different and everyone is an individual with worth and value.”
Person-centred care and recovery-oriented practice: a convergence of ideas and approaches
Services cannot make people recover a fulfilling and satisfying life with dementia, but they can support individuals and those who are close to them in their journeys: help people to grow beyond their diagnosis and ‘continue to be me’. Creating recoveryfocused services is not just about adding another intervention to our repertoire – it requires fundamental changes in culture and practice. This was recognised in the development of ‘person-centred care’ (Kitwood, 1997) and parallels exist between ‘person-centred care’ in dementia and ‘recovery-oriented practice’ in working age adult services.
Ideas about recovery among younger adults emerged from the expertise of lived experience (see, for example, Chamberlin, 1977; Deegan, 1988) while ideas about person-centred care arose from the work of professionals and academics. However, the ‘recovery-oriented practice’ that these ideas about recovery have spawned (Repper and Perkins 2003; 2012; Care Services Improvement Partnership 2007; Shepherd et al, 2008; O’Hagan, 2014) share a value base with ‘person-centred care’ (see Box 2). Both approaches unite in “an emphasis on ‘repersonalising’ or ‘recovery of the person’.” (Hill et al, 2010).
Deegan (1996) described the dehumanising impact of diagnosis and treatment
“We found ourselves undergoing that dehumanizing transformation from being a person to being an illness: “a schizophrenic”, “a multiple”, “a bi-polar”. Our personhood and sense of self continued to atrophy as we were coached by professionals to learn to say, “I am a schizophrenic”; “I am a bi-polar”; “I am a multiple”. And each time we repeated this dehumanizing litany our sense of being a person was diminished as “the disease” loomed as an all powerful “It”… we learned to equate our very selves with our illness. So much of what we were suffering from was overlooked.
The context of our lives were largely ignored … no one asked for our stories. Instead they thought our biographies as schizophrenics had been already been written nearly a century before by Kraeplin and Blueler.” (Deegan, 1996)
Kitwood (1997) described being appalled by the image of dementia as ‘death that leaves the body behind’ and the negative discourse used to describe people with dementia such as ‘victims’, ‘dements’ or ‘elderly mentally infirm’. He argued that the time had come to recognise men and women with dementia in their full humanity. He argued the frame of reference should be the ‘PERSON-with-dementia’ rather than ‘person-with-DEMENTIA’.
These similarities allow the possibility of cross-fertilisation: there may be much that recoveryoriented services for working age adults with mental health conditions can learn from personcentred services for people with dementia and vice versa.
Box 2: Principles underpinning in recovery-oriented practice and person-centred care
Adapted from Hill et al (2010)
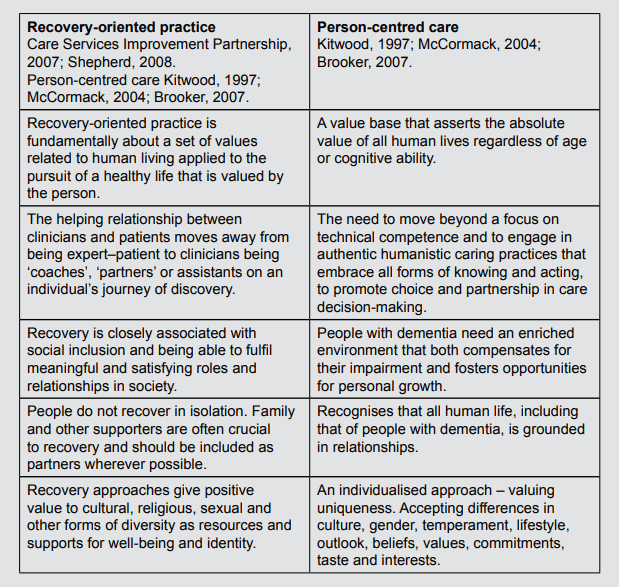
Like person-centred care, recovery-focused practice shifts the focus from itemising deficits and dysfunctions to recognising a person’s strengths and possibilities. It involves creative and collaborative ‘positive risk taking’ to enable people to do the things they value and is based on collaboration, partnership and self-directed care. There are however differences between recovery and person-centred care, most notably, that unlike recovery, person-centred care has evolved as, and remains a professional-led approach to working with people with dementia.
Finding hope, living positively
One of the biggest challenges for services is helping people to believe that a decent life is possible with a diagnosis of dementia.
“Hope is about believing in yourself and being willing to ‘hang on in there’: persevere and pick yourself up again when you are knocked down. Hope does not arrive like a bolt of lightning – it begins as a small fragile flame that can be fanned or snuffed out.” (Repper and Perkins, 2012).
The importance of hope in services for people with a diagnosis of dementia has long been recognised. A sense of hope is one of Kitwood’s (1997) four ‘global sentiment states’ that are central to the wellbeing of people living with dementia. Lintern et al (2000) showed that hopefulness and respect for personhood are critical factors in dementia care while Zimmerman (2005) and Spector and Orrell (2006) showed that, from residents’ perspective, quality of life was higher in facilities where care providers felt more hope. Hope on the part of care givers is critical in fostering a belief that a fulfilling life is possible with a diagnosis of dementia. Woods (2007) discusses what hope might mean in working with people with dementia:
You need people who believe that there is a way to get through … even if it takes time … people who can encourage and support and help others realise they can make a difference to the person with dementia, not just ‘baby sitters’!!”
(Woman with a diagnosis of dementia, Kensington and Chelsea Memory Group)
“We encourage carers to look out for and appreciate the good times they share with the person they care for. At the time these can seem rare and insignificant, but with some distance they can make the overall experience positive. Seeing my dad play a keyboard badly for a couple of minutes, long after he’d apparently lost the ability to comprehend anything, is a far more important memory for me than the hours it took to organise.”
(Mike Chappell, Compass Worker Lead)
Fostering hope in relatives and friends who provide care and support can be an effective way of maximising the chance of people who have the diagnosis living well. Relatives are themselves products of a society where negative images about dementia prevail. It is, therefore, not surprising that they often start from a position of hopelessness. However, as their relationships with the person who has the diagnosis are far more deep-rooted, intense and consistent than any professional support could hope to be, it makes sense to support them to view the possibilities of life with dementia in a more positive light, so that they can sustain their belief in the person they care about and can better adapt to their changing needs.
“It’s not about believing a cure is just around the corner. Rather, it’s the ability to see that small things can make a difference, and a real difference at that. It’s about recognising the look of pleasure when the person is offered their favourite food, or hears their favourite music …” (Woods, 2007)
If professionals are to foster hope in individuals with dementia and those who are close to them, then they must themselves “believe that there is a way to get through”. Health workers are not immune from the negative images of dementia that prevail so training can be important. An education programme in Surrey and Sussex – Time for Dementia – has been working with 400 people with dementia and their families and 800 medical, nursing and paramedic students from the Brighton and Sussex Medical School and University of Surrey7. In the programme, students visit a person with dementia and their relatives at home over a two year period and spend two to four hours with them on each visit. The idea is to improve understanding, knowledge, attitudes and empathy towards people living with dementia and help students understand how people do live well with dementia. The people with dementia involved have seized this opportunity to use their lived experience meaningfully to contribute towards the training of future professionals, and preliminary findings suggest a positive shift in student attitudes.
Fostering hope: creating a hope-inspiring environment
The environment has a major role to play in fostering hope and enabling people to live positively: both the environment in which people live (whether this be their own home or a residential or nursing home) and the environment within services. What messages do services convey about the people who use them? Do they offer images of possibility or images of doom and gloom? Does it demonstrate that those who use the service are respected and valued? How much does it enable people to be part of local communities?
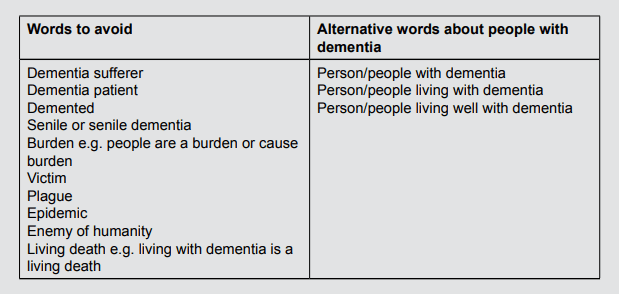
It is important that the environment actively challenges prevailing negative images of dementia, and this requires attention not only to the physical environment but to language that is used. Language matters.
“Words are very powerful – they can build you up or put you down. When you are speaking about dementia, remember this.” Agnes Houston http://www.dementiadiaries.org/about-the-project
“The language we use to talk about dementia influences how people with dementia are viewed and also how they feel about themselves.” http://dementiavoices.org.uk/wp-content/uploads/2015/03/DEEP-Guide-Language.pdf).
The Dementia Engagement and Empowerment Network (DEEP) have produced guidelines on language about dementia created by 20 people living with dementia8. They identify a series of ‘curl up and die’ words that should never be used – words that create negative stereotypes and send out a message that life with dementia is not worth living – as well as offering acceptable alternatives (see Box 3).
Box 3: Dementia words matter
From Dementia Engagement and Empowerment Network
http://dementiavoices.org.uk/wp-content/uploads/2015/03/DEEP-Guide-Language.pdf
Fostering hope: helping people to make sense of what has happened
Given the devastating nature of a diagnosis of dementia, individuals and their families need to grieve, and, as with any bereavement, people respond in different ways. Facing and accepting a diagnosis can be a lengthy process and may be accompanied by a range of emotions: fear, terror, shame, guilt, denial, anger, sadness, bitterness and despair. People often feel isolated and helpless. It is important to understand that these are normal reactions and that there is no right or wrong way of coping with the devastating news
“Some people divide emotions into those that are acceptable and those that are not. Some are afraid of strong emotions as they fear they may lose control or receive criticism from others. Mixed feelings can also be problematic. Emotions may be experienced at any time and people may jump from one to another. Sometimes you may have conflicting emotions such as feeling optimistic about the possible effects of medication whilst at the same time feeling utter despair about the changes that are occurring in your life.
Denial is sometimes used as a way to cope e.g. putting everything down to “normal aging” or “an incorrect diagnosis” or simply choosing to ignore the diagnosis. This kind of denial, which is sometimes used by carers as well as people with dementia, can serve as protection against a reality which is too hard to deal with at the time. In such cases, it is best to respect the person’s needs and be ready to support them should they eventually decide to address the issue.” (http://www.alzheimereurope.org/Living-with-dementia/Afterdiagnosis-What-next/Diagnosis-of-dementia/ Facing-the-diagnosis)
Having someone to talk to is important for most people.
“ Talking to someone who really understands makes me realise I am not alone.” (in Mental Health Foundation, 2005)
“I and my Compass colleagues often have a feeling that the support we provide is inadequate; how can a few quid from a carers assessment or information about other services make up for the challenges they are facing? I think it is natural for most of us to measure our effectiveness in terms of results from practical interventions. However, time and again carers express enormous gratitude for us “just being there”: emotional support has a very positive effect on them.” (Mike Chappell, Compass Worker Lead)
In helping people to make sense of what has happened it is important to both appreciate the devastating impact of the diagnosis and foster a positive vision of the future. This can take time and involves:
- Understanding and empathising with what has happened and what it means in the context of their life
- Recognising the enormity of the challenge
- Understanding what is important to the person
- Believing that a decent life is possible for the person
- Helping people to make sense of what has happened within their own philosophical/ spiritual framework: ‘Why?’, ‘Why me?’ ‘What’s the point?’ ‘Who am I now?’
In making sense of what has happened, three things may be particularly important: spirituality (‘being philosophical’), story-telling and peer support.
1. Spirituality – ‘being philosophical’
The quest for meaning lies not in psychiatry, but in spirituality or philosophy.
“My friends say that I have developed a very philosophical attitude towards life. I think that it was necessary for me in order to cope.” (Janice – http:// www.alzheimer-europe.org/Living-withdementia/After-diagnosis-What-next/ Diagnosis-of-dementia/Facing-thediagnosis)
Spirituality and philosophy are not necessarily the same as formal faith or religion. White (2006) outlines three areas that might usefully be explored in talking about spirituality in healthcare:
Meaning and purpose
- What gives you a sense of purpose?
- Do you have a specific aim that is important to you at the moment?
- Do you believe in any kind of existence after life?
- Has your illness affected your attitude to the future?
- What bothers you most about being ill?
Security and hope
- What are your sources of strength and hope?
- Who do you turn to when you need help? In what ways do they help?
- What inner resources do you draw upon?
- Where do you go for comfort and support?
- Who or what do you depend on when things go wrong?
Religion and spirituality
- Do you consider yourself religious or spiritual?
- How does this affect you? Has being ill changed this?
- Is prayer helpful to you? Can you talk about how?
- Is there anything we can do to support your spiritual or religious practice?
“My dad was both deeply religious and deeply spiritual; it was by far the most important aspect of his identity. As an atheist, helping him maintain this identity was very challenging but ultimately something I’m very proud of. I’ve since supported carers for whom a connection to god, and or a church, has been a great source of comfort and pleasure to them and the people they care for.”
(Mike Chappell, Compass Worker Lead talking about his father)
2. Story-telling
Story-telling is also important in providing a sense of identity and possibility. Human beings are story telling creatures. We know ourselves through the stories we tell of our lives. When traumatic events befall us we have to retell the stories of our lives. We connect with other people by sharing our stories. We understand our possibilities by seeing what others who have been in a similar position have achieved (Repper and Perkins, 2012). ‘Life Story Work’ has long been used with older people on medical wards and in residential care homes as well as people with dementia (see McKeown et al, 2006). It helps people to retain a sense of themselves (‘continue to be me’) and enables the person and others to see themselves as more than ‘an illness’. It enables people to celebrate their lives and, in an era where discovering one’s roots and ancestry is becoming increasingly popular, it offers the gift of history to future generations (thus enabling people to do something for others).
“Listening to someone with dementia tell a story about their past in the company of their carer can sometimes be an interesting experience. The speaker becomes animated and joyful whilst the carer rolls their eyes upwards, shakes their head and becomes irritable – they have heard the story many times. A great reason for a fresh pair of ears occasionally.” (Mike Chappell, Compass Worker Lead)
Helping people to pull together their life stories can also be an important way to:
- challenge ageist assumptions and attitudes,
- improve staff understanding of people’s behaviour,
- bridge generational gaps between people providing support and those they are supporting
- provide a basis for individualised personal care that reinforces identity and personhood,
- identify valued roles that the person has had…and could still have,
- assist in the transition from one care environment to another (e.g. moving into residential care), and
- improve relationships between care staff and family carers.
By sharing stories in families people can celebrate stories and lives they have shared, and sharing stories with others makes links and enables people to feel less alone, gain images of possibility. Reading or hearing the stories of others can help people who are facing similar challenges and is thus a way of using our experience to help other people and provide peer support.
‘Real life stories … are nutritious and sustaining. They feed the mind with information and the heart with hope and strength.’ (Pullman 2006)
3. Peer support
Many people have found that others who have experienced similar challenges have been particularly useful in helping them in their own journey. Peer support for both individuals with a diagnosis of dementia and their relatives/friends can:
- help people feel less alone,
- foster images of hope and possibility,
- allow people to share experiences and different ways of understanding what has happened,
- help people to work out ways of dealing with problems and challenges, and
- offer support from someone who really understands what you are going through.
“I needed to know that I was not the only one.”
“I no longer feel isolated and alone. I have made many new friends, including many who support me, and of course, others with dementia. We are a great bunch of people.”
(in Mental Health Foundation, 2005)
For family carers, acknowledgement that they are in a difficult situation, that they have frailties like anyone else and, most importantly, that they are doing a good thing well, can be vital. Maintaining a belief in the person they support and care about can be extremely difficult. Love and a sense of duty may keep the person going, but when the person you know has apparently ‘gone’ – they don’t recognise you, you can’t have any meaningful conversation and you might be subjected to verbal abuse or violence – then belief is hard to summon.
“When belief is missing, grief and guilt can take its place: this is a time when talking to a peer can be helpful. Someone who can agree that it’s really difficult, that we’re only human and that inevitably things don’t go the way you’d like. Someone who can remind a carer that they’re doing a wonderful thing for the person they love and help them find ways of making life better for them both. A good example of this is helping a carer understand how different reality can be for someone with dementia and encouraging them to go with the alternative reality (even if this means denying their own existence!). As well as reducing the potential for conflict, this can lead to opportunities to enjoy new experiences together.” (Mike Chappell, Compass Worker Lead)
Providing peer support to others is also a way of using your experience and being useful to others.
“I volunteer as a peer-support worker at the Memory Service. I was very, very pleased, it lifted me up tremendously, knowing that I was some value and that I was going to be useful.” (https://www.mentalhealth.org.uk/stories/ patricias-story-if-you-think-old-you-willbe-old-if-you-think-young-youll-stayyoung#sthash.JHcqA7CL.dpuf)
“I cannot believe my good luck that I’ve been able to use such a difficult experience in such a positive way.”
(Mike Chappell, Compass Worker Lead talking about his father)
The National Dementia Strategy for England (Department of Health, 2009) recommended that Peer Support Networks and Dementia Advisors be established in 40 demonstration sites. These aimed to provide people with dementia and carers with information, guidance and advice, and enable access to a wide range of support including social groups that enabled peer learning.
“Peer support by and for people with dementia and carers was rooted in identification with others in a similar position, enabling greater confidence and more independence.” (Clarke et al, 2013).
The evaluation of these peer support networks concluded that:
“Peer Support Network services had a significant role in enabling people with dementia and carers to re-narrate their lives, finding a new life which, though different from life prior to dementia, had meaning, value and purpose and in signposting people with dementia and carers to appropriate other services and support.” (Clarke et al, 2013)
Peer support may take many forms including:
- sharing stories (for example, http://www. dementiadiaries.org)
- e-based peer support, for example, Alzheimers’ Society Talking Point (http:// forum.alzheimers.org.uk/ ),
- peer support workers with early dementia working in services for people with dementia (see, for example, https://www.youtube. com/watch?v=ol7-l5YrWc0
- a range of peer support groups and networks.
Some of these networks have a broader role in raising awareness and influencing the design of services as well as providing peer support. For example, EDUCATE (www.educatestockport.org.uk):
“We are a Stockport based group of people living with dementia, who raise awareness about dementia. We meet regularly to share our experience of managing the difficulties dementia can cause. Our aim is to inspire others to live well with dementia, and to involve people with dementia in the life of their communities.”
(www.educatestockport.org.uk)
Personal Control: Looking after yourself
Enabling people to make decisions, choices and do things for themselves, and respecting those decisions, is critical in services for people with a diagnosis of dementia.
“You must listen to us much more – please!”
“We are the real experts”
“We need support and care just as all others do and our carers are of enormous importance and we value them greatly. But we also need empowerment and independence”
(in Care Services Improvement Partnership, 2007)
There is not one set of experts but three: those with a diagnosis of dementia, the people who are close to them and professionals. All too often the expertise of lived experience, and preferences, interests and skills, are overlooked.
“… it’s about realising the person may be able to be independent in dressing if we laid the clothes out in the right order; it’s about recognising that the person is able to take in new information and can speak for him/herself … Perhaps above all, it’s recognising that what makes life meaningful for one person may not be of interest to the next and that abilities change and fluctuate from day to day, so we need to be flexible in our response.” (Woods, 2007)
‘Continuing to be me’ involves continuing to do things for yourself and look after yourself as far as you can, making choices about what you want and doing the things you value. For professionals, this involves practices which help to maintain identity or build resilience. For example, sometimes people will need help to make decisions (it is often easier to make a choice between a couple of things than respond to broad general questions ‘What do you want?) and to do things for themselves. Assisting people to make decisions and do things for themselves may take longer than telling people what to do and doing things for them, but it is critical in enabling people to retain some control, agency and sense of self.
“Don’t just tell me what to do. Help me to make choices”.
“Being encouraged to do as much as possible keeps me going. It stops me feel unwanted and builds my confidence”
(In Care Services Improvement Partnership, 2007)
Supporting self-management: Information
There have been debates around whether it is best to tell people about their diagnosis or not (for example, because therapeutic options are limited and the level of anxiety a diagnosis may produce in the individual being told). Some people would prefer not to know their diagnosis.
“I am certain that lack of a formal diagnosis until late on enabled my father to have the full life he did, despite the obvious difficulties caused by his dementia. After retirement and the onset of dementia, freed from the burdens of being a parish priest, my dad was able to devote himself to his spiritual life and the promotion of harmony within and between faiths. He was very much in demand as a spiritual mentor and champion of ecumenicalism. We didn’t actively avoid a diagnosis for my dad, but we didn’t actively seek one either. On balance I think this worked for my dad but probably made crises more difficult for me when they occurred.” (Mike Chappell, Compass Worker Lead talking about his father)
However, most people with the diagnosis are clear about their right to know what is happening to them (see Pratt and Wilkinson, 2001).
“I would shoot the person that tried to keep it back from me, I really think it’s an absolute disgrace, you should be told at the earliest moment, even if people say to you it might be that, we’ll have to test it, even tell them then. Then if you want to ignore it, ignore it if you wish, but it’s your choice, it’s not the doctor’s choice, or the carer’s choice, it’s your choice, and you should be given that choice.” (in Pratt and Wilkinson, 2001)
Information is central to making choices and many people with dementia, and those who are close to them, have spoken about how important learning about dementia, and those who are close to them, has been in enabling them to take control over their lives. Indeed, the provision of high quality information is a central tenet of the English National Dementia Strategy (Department of Health, 2009).
‘ Learning about dementia has taught me how to live my life again. I am not going to let it control me.’ (In Mental Health Foundation, 2011)
However, information must include both the expertise of professionals and the expertise of those who live with the diagnosis. While some people prefer to access information at individual meetings with Peer Support Workers and professionals, bringing together professional and lived experience in co-produced and co-delivered courses, maybe within Recovery Colleges, has proved useful9. These enable individuals, their relatives and staff to learn together. Cheffey et al (2016) found practical and emotional challenges when their co-producer with dementia was repetitive or struggled with concentration and attention, but there was no space for people to feel uncomfortable about dementia and there were no insurmountable challenges which time and careful planning could not address. More importantly, the value of combining ‘experts by experience’ and ‘experts by training’, led to a powerful and enriched learning experience leading students to comment: “his [the co-producer with dementia] insights were invaluable” and “I will make a point of looking at the person and not the diagnosis”.
Supporting self-management: Self-management plans
An important part of taking control and doing the things you value is working out strategies for managing the memory difficulties and other cognitive challenges that you face.
Self-management is increasingly recognised as important in other long term and progressive conditions. Teaching self-management techniques, for example to people with Chronic Obstructive Pulmonary Disease improves health related quality of life compared with usual care (Jordan et al, 2015). There is evidence for the use of self-management techniques in people with mild cognitive impairment (The Health Foundation, 2015): THYMe (Think Health for your Memory) groups supported participants to identify and complete goals and develop confidence to manage their memory difficulties.
People living with dementia have compiled lists of things that they have found helpful (see Box 4 for an example).
Box 4: Some strategies people with dementia have found helpful
From Mental Health Foundation http://www.mentalhealth.org.uk/publications/stillgoing-strong
- Follow a daily routine. This can stimulate your memory and help you feel calm and balanced.
- If there are regular things you need to remember, like locking doors or taking medication, write them on a notice board and pin them up somewhere prominent.
- It’s also fine to ask someone to repeat themselves if you haven’t understood or have forgotten something they said.
- Carry a notebook with lists of people’s names, telephone numbers and daily tasks written inside – you can refer to it if you have trouble remembering things.
- Write telephone numbers of important people – your friends, family, GP, and care staff (such as your CPN) – on a pad near the phone.
- Keep important items, like keys, spectacles or your notebook, in the same place, so you get in the habit of knowing where to look for them.
- Ask your bank to set up direct debits to pay all your important bills, so that you don’t need to worry about them.
- Carry a card which tells people that you have dementia. This can be useful if you get into a difficult situation and need someone to help you. Include the telephone number of someone you trust who can be called if necessary.
- Go easy on yourself. It’s OK to take your time over essential tasks that you might have done more easily in the past.
- Stay in touch with friends and family. Maintaining a social life can help prevent you from becoming isolated.
- Focus on what you can do, rather than what you can’t. Keeping positive will help you enjoy life.
- Remember that dementia is a disability. It is not your fault if you have difficulty remembering things or doing things which used to seem easy. Don’t worry what other people think – it is their problem if they cannot deal with your disability.
- Get to know as much as you can about dementia. The more you know, the more you will feel able to cope.
It is not only the person with the diagnosis who is living with dementia, so are the friends and relatives and supporters. They too must find strategies for coping. For example, Alzheimer Europe provides suggestions of coping strategies for both the individual and those supporting them. These can be seen in Box 5.
Box 5 Developing coping strategies: things that carers have found helpful
From Alzheimer Europe http://www.alzheimer-europe.org/Living-with-dementia/ After-diagnosis-What-next/Taking-care-of-yourself/Developing-copingstrategies/%28language%29/eng-G
Devise a problem solving strategy:
- Define the problem, explore possible causes and think about ways to overcome/deal with it.
- Use your own knowledge/experience and ask other people for advice.
- Collect as much information as you can and then set realistic goals.
- Try different solutions in order to find the one that works best for you.
- Try to prevent the problem from occurring by planning ahead.
- Do a risk assessment on what the person with dementia can safely do (if necessary consult someone qualified).
Be supportive:
- Try to adapt to the changing needs of the person with dementia.
- Assist when needed and discuss things together if you can.
- Be calm and patient when handling problems.
- Stimulate and encourage the person with dementia to remain active.
- Take them out for a drive or encourage them to accompany you to different places e.g. a walk, a visit to the gym or the local library.
Develop a positive outlook:
- Avoid catastrophic thinking (e.g. I lost my wife in the supermarket for five minutes so I am totally useless or I should never take her out of the house again).
- Remember the good times you had together.
- Remember that the disease is the problem and not the person with dementia.
- Remind yourself of things you do well (particularly when something goes wrong!).
- Remember that nobody is perfect and don’t be too hard on yourself.
Lists such as those provided in Boxes 4 and 5 can offer some ideas for strategies that have been helpful based on the lived experience of people who have faced similar challenges. However, there is no set formula. Some prefer not to have a diagnosis – denial can be a coping strategy that allows some people to carry on – and, while written notes and reminders can be helpful, it is possible to have too much of a good thing:
“My dad had so many note-books and signs littering his house that they actually became confusing and unhelpful.” (Mike Chappell, Compass Worker Lead talking about his father)
Each individual, and those who are close to them, must work out what works for them, and again, little things can make a big difference.
“I always used to lay the table at mealtimes but I started to get mixed up with the cutlery. So now I clear the table after the meal instead. I think it helps a bit.” (Hector – http://www. alzheimer-europe.org/Living-with-dementia/After-diagnosis-What-next/Taking-care-ofyourself/Developing-coping-strategies/%28language%29/eng-GB
“At family mealtimes in our house, it was a rule that everyone had to be served before you started eating. As my father’s cognitive abilities deteriorated he would simply start eating as soon as the food was put in front of him – causing great upset to my mother, especially if we had guests.This problem was solved by adopting the strategy of serving him last.” (Rachel Perkins, ImROC Senior Consultant talking about her family)
Younger adults living with mental health challenges have often found ‘Personal Recovery Plans’ or ‘Wellness Recovery Action Plans’ helpful in taking back control over the challenges they face10. These involve the personal strategies that people have developed to keep on an even keel, and how to deal with both things that upset them and times when their problems are worse. Cheffey et al (2013) discuss how such personal self-management plans, based on the original Wellness Recovery Action Plan (Copeland, 1997), might be developed for people living with the early stages of dementia.
The wellbeing of family and friends who are supporting someone with dementia is important – family and friends who provide care need to be encouraged to look after themselves as well: a happy, healthy carer is in a better position to provide love and support to their relative. Carer Peer Support Workers can have an important role to play, but relatives and friends may also benefit from developing their own personal health and wellbeing plan (see Repper, Perkins and Meddings, 2013). This might address how relatives can look after their own health and wellbeing, plans for managing challenges they face and where they can get help when everything is getting too much for them.
When people are unable to tell others what they want
People with dementia often live happy, fulfilling lives for years after they have been diagnosed. However, as dementia progresses, relatives, friends, informal carers and services have to take on a greater and greater role in enabling the person to retain a sense of identity – to ‘continue to be me’ (Daley et al, 2013). Eventually people may become less and less able to communicate their preferences and wishes; therefore the provision of the personalised support that preserves a sense of identity becomes more of a challenge.
Advance decisions and advance statements can enable people to make choices and decisions about their future care if the time comes when they are unable to articulate these for themselves11. They enable people to specify what treatment they wish to receive and who they want to make decisions for them. However, it is also important to have more detailed information about the person’s key roles and preferences (daily routines, interests, favourite things – TV, music books/ magazines/newspapers, things that are important to you and how you like to spend your day, food and drink preferences etc.) that are central to maintaining a sense of identity – ‘continuing to be me’. Small things can make a big difference.
“As her dementia progressed, my mother-in-law continued to come to lunch with us every Sunday. Being a mother was very important to her so at lunch she continued to sit at the head of the table and always wore her ‘Super Mum’ apron.” (Jane Rennison, Recovery Lead and Head of Occupational Therapy talking about her mother-in-law)
‘This is me’, developed by the Alzheimer’s Society, is a simple, practical tool developed for people with dementia to tell staff about their needs, preferences, likes, dislikes and interests12. It was originally developed for people with dementia who were going into hospital but can be used by people with dementia who are receiving professional care in any setting – at home, in respite care or a care home. It enables health and social care professionals to see the person as an individual, encouraging person-centred care, tailored to the person’s needs. Such information about roles and preferences can be particularly important if the person moves into residential care enabling support staff to preserve the continuity and connectedness that are so important for a sense of identity and personhood: ‘continuing to be me’. Those close to the person can explain these roles and preferences if the person has not done so themselves.
As dementia progresses, communication becomes more of a challenge13. People may not be able to communicate their preferences and wants verbally and non-verbal communication can become increasingly important. When a person with dementia becomes distressed or behaves in ways that cause problems for those who are supporting them, they are trying to communicate something (Alzheimer’s Society, 2005). Communication can be aided by people providing care and support seeing the world from the perspective of the person with dementia (Brooker, 2004)
“Even if I forget my facts, I can remember the feelings” (in Care Services Improvement Partnership, 2007)
“ Feelings remain when facts are forgotten. Patterns from the past continue” (Woman with a diagnosis of dementia, Kensington and Chelsea Memory Group)
For people with dementia in residential care settings, ‘Dementia Care Mapping’14 offers an approach to enabling others to understand what a person is trying to communicate. The social world that surrounds a person has a significant effect (positive or negative) on the person’s well-being. Enhancing well-being requires a focus on the uniqueness of each person and things that enhance or detract from their well-being.
“Dementia care mapping is a process that helps a professional to observe life through the eyes of a person with dementia. It involves watching someone unobtrusively over an extended period of time to see how they respond positively or negatively to events that happen to – and around – them.” (Morley et al, 2010)
The information gained from dementia care mapping can then be used as the basis for person centred planning. It can be used in developing a ‘one page profile’ of the person and what is important to them, identifying personal enhancers and detractors in the form of a ‘What is working/ What is not working’ sheet and developing a ‘communication sheet’, identifying what the person does in which situations, what we think it means and what we need to do (see Morley et al, 2010).
Personal budgets can also be an important tool in fostering choice and control and tailoring support to the wishes, preferences and needs of the individual and their family (Alakeson and Perkins, 2012). In England, since October 2014, adults receiving NHS continuing care have had a right to have a personal health budget15. Personal budgets have been used to good effect to enable people to stay at home, rather than enter residential care, and continue to do the things they value.
“Debbie was able to care for her father at home during his last months, using a personal health budget to arrange flexible nursing, which allowed her to care for her father while working and caring for her son.”
“Louise, 90, has Alzheimer’s disease. Her personal health budget, managed as a direct payment for healthcare by her daughter, pays for personal assistants to care for her at home. Louise’s daughter Mary says that Louise’s quality of life has “increased exponentially”.
(Department of Health (2012)
“Three years on, we employ four members of staff who have all worked for us for at least two years. My dad no longer attends the day centre and spends more time at home. He enjoys doing things that HE chooses, more often, like feeding the ducks, going for walks, listening to music and going to football matches … he can enjoy some peace and quiet watching the TV programmes of his choice with a single personal assistant who understands his needs and wishes…and much, much more!”
(Cited in Think Local Act Personal, 2013)
Opportunity and Participation: the chance to do the things you value and be a part of your community
A sense of purpose and self-worth and the opportunity to contribute to your community are central to everyone, and no less important for people living with a diagnosis of dementia.
“Having dementia may change what a person can manage over time, but it will still be possible to celebrate and support what they can do.’” (Mental Health Foundation, 2011a)
However, too often it remains the case that:
“For many people with dementia [and their relatives], the battle is not just about getting a diagnosis and support from the health and social care system, but about the everyday things we all take for granted – having control over daily life, spending time with friends and family and enjoying hobbies.” (Crampton et al, 2012)
“I don’t want to sit here all day and wait for the news to come on. I’d rather get a newspaper, I’m still part of the world.’
(Woman with dementia, Daley et al, 2013)
Participating in valued activities also provides the opportunity for social contact that is so central to the health and wellbeing of people living with dementia and relatives/ friends who support them (Holt-Lunstad et al, 2010). Social isolation and loneliness have a detrimental impact on quality of life and wellbeing, adversely affect health and increase use of health and social services. (Social Care Institute for Excellence, 2011). 38% of all people living with dementia, and 62% of those living alone, report feeling lonely16 yet this subject is rarely addressed in the clinical sphere (Bailey et al, 2015).
A number of initiatives have been developed to reduce loneliness and isolation (Social Care Institute for Excellence, 2011; Davidson and Rosall, 2014).
- Individual, one-to-one interventions such as befriending, mentoring and Community Navigators.
- Group services and networks, from traditional ‘day centres’ and ‘luncheon clubs’ through to ‘dementia cafes’ and self-help and self-support groups17.
- Wider community engagement including a range of initiatives to increase participation in existing activities such as sport, libraries and museums.
Peer support may be particularly important in this context: both reducing social isolation and enabling people to use their skills and experience to assist others facing similar challenges (Clarke et al, 2013). Many local groups of people living with dementia have now been formed18 that often have both a peer support and a campaigning role (see Williamson, 2012).
Via these and other initiatives, a new perspective for thinking about people living with dementia is emerging: a perspective that focuses not on individual deficits and dysfunctions, but on human rights within a social model of disability. At present, a ‘clinical model’ is generally used to understand the social exclusion of people with dementia. That is, the exclusion from family, social, economic and cultural life of people living with dementia is understood as a function of the cognitive deficits associated with their dementia: people are unable to participate because of their memory deficits etc. In former times this was the overarching framework for understanding all experiences of disability. However, over recent decades this has changed. The ‘social model of disability’ conceived by the disability rights movement argues that barriers to participation lie not within the individual but in our communities and in society.
“It is society that disables people. It is attitudes, actions, assumptions – social, cultural and physical structures which disable by erecting barriers and imposing restrictions and options. Disability is not inherent. …The social model of disability is about nothing more complicated than a clear focus on the economic, environmental and cultural barriers encountered by people who are viewed by others as having some form of impairment – whether physical, sensory or intellectual” (Oliver, 2004)
Within this framework, rather than trying to change people so they ‘fit in’ (and explaining their continuing exclusion in terms of their deficits, dysfunctions and problems) such an approach clearly places the responsibility on society to make the necessary adaptations and provide support to enable ALL citizens – including those living with a diagnosis of dementia – to participate as equal citizens. Such an approach within the broader disability rights arena has resulted in the right to participation in all facets of community life being enshrined nationally in the GB Equality Act (2010) and internationally in the United Nations Convention on the Rights of Persons with Disabilities (UNCRPD, 2006) that has been ratified by the UK and 227 other countries. These relate to people with the full range of long-term physical, cognitive, intellectual and sensory impairments … which clearly includes people with dementia. The UNCRPD marks a paradigm shift in attitudes and approaches to persons with disabilities from objects of charity to subjects with rights:
“The Convention takes to a new height the movement from the treatment of persons with disabilities as “objects” of charity, medical treatment and social protection towards viewing persons with disabilities as “subjects” with rights who are capable of claiming those rights and making decisions for their lives based on their free and informed consent as well as being active members of society. The Convention gives universal recognition to the dignity of persons with disabilities.”
(http://www.un.org/esa/socdev/enable/ convinfopara.htm )
This includes both the right to the same opportunities as other citizens (at home, at work and as members of the community) and the right to the support and adjustments (based on their own preferences and choices) that people need to participate as equal citizens.
In relation to people with dementia, the relevance of a human rights based social model of disability was first explicitly suggested by the Care Services Improvement Programme (CSIP) National Older People’s Mental Health Programme (2007), and although there has been some discussion of its importance since (e.g. Perkins, 2013, 2014) perhaps the most extensive consideration has been offered by McGettrick and Williamson (2015). They argue that the prevailing deficit based ‘clinical approach’, with its focus on what people cannot do, has resulted in low expectations of people with dementia among public, policy makers, professionals and people with dementia themselves. This too often means that people with the diagnosis are viewed as portrayed as ‘victims’ and ‘sufferers’ who are unable to speak for themselves, have little useful to contribute and are therefore denied a voice in decisions that affect them and the design of services.
A rights-based approach within a social model of disability starts from a different place. It starts from the perspective that people living with a diagnosis of dementia are citizens with rights who are deserving of respect. The focus is not on ‘care’ but on ‘opportunity’ and the support/adjustments necessary to enable people to use their skills, do the things they value and be a valued part of their communities. Such a perspective provides greater autonomy, dignity and influence to people with dementia and could have as major a role in driving institutional, systemic and societal changes as it has in the broader disability world. It shifts the focus from identifying deficits and dysfunctions that prevent participation to identifying barriers that prevent participation (attitudes, expectations, assumptions – social, cultural and physical structures) and adjustments and supports necessary to facilitate access and inclusion … and people’s rights to the adjustments and supports they require. As a human rights based approach it is based on the principles of participation, accountability, non-discrimination, equality, empowerment and legal rights. A rights-based approach and social model of disability can play a central role in the creation of Dementia Friendly Communities (Crampton et al, 2012; Joseph Rowntree Foundation, 2015; Local Government Association and Innovations in Dementia, 2012) and a recognition of the expertise of lived experience in the coproduction of policy and services.
Dementia Friendly Communities
If people living with dementia are to have the opportunities that are their right, then the creation of communities that can accommodate all of us – ‘Dementia Friendly Communities’ – is of the essence (Local Government Association and Innovations in Dementia, 2012). A dementia friendly community might be defined as a place:
- in which it is possible for the greatest number of people with dementia to live a good life.
- where people with dementia are enabled to live as independently as possible and to continue to be part of their community, and
- where they are met with understanding and given support where necessary.
Five domains need to be addressed as part of developing a dementia-friendly community:
- The place: the physical environment – how easy it is and finding your way around.
- The people: the attitude of the people with whom they come into contact.
- The resources: resources to support people – formal services and volunteer, buddy and befriending schemes.
- The networks: relatives, friends, neighbours, service providers, as well as community leaders and local businesses.
- The person with dementia: the importance of the message ‘it is possible to live well with dementia’.
When people living with dementia and their supporters were consulted, they said that a dementia friendly community is one that enables them to find their way around and be safe; access the local facilities that they are used to and where they are known (such as banks, shops, cafes, cinemas, post offices); and maintain their social networks so they feel they can continue to belong. They would like to be able to simply go out more, pursue hobbies and interests, make more use of local facilities and help others in their community (for example, by volunteering). They said that they feel able to continue to do things they have always enjoyed if they feel welcomed and encouraged … but stop doing things and being involved if they feel they are a nuisance, if the atmosphere is discouraging in any way, if they are worried about their ability to cope as their dementia progresses and where they are concerned that people don’t understand their dementia. In particular, “People told us that one-to-one informal support was the key to helping them do these things.” (Local Government Association and Innovations in Dementia, 2012). Initiatives developed within the English pilots included ‘help card schemes’, ‘memory aware’ high street schemes (a ‘Memory Aware Kite Mark’), dementia awareness raising for staff and a help-pack for customer-facing staff19.
Recognising the expertise of lived experience at a policy and service level
The voices of people with dementia have only recently begun to be heard. Too often it has been assumed that people with dementia cannot speak for themselves and therefore they have not been involved in the development of policy or services. Organisations that speak on behalf of those living with dementia have developed, but organisations OF people living with dementia have been few and far between. This is now beginning to change. Local groups of people living with dementia have begun to emerge across England, Scotland, Wales and Northern Ireland20. Many of these groups have come together in the Dementia Engagement and Empowerment Project (DEEP)21.
Initially DEEP brought together 12 local groups of people living with dementia to network and connect together, share ideas and sometimes work collectively on national dementia issues (Williamson, 2012). By 2012 this had increased to 50 groups involving some 1000 people living with a diagnosis of dementia (Litherland, 2015). More recently, international networks are emerging22.
“You can start to think that you are the only ones doing it – DEEP helps you to see you are not alone.”
“We need DEEP if people with dementia are to have any chance of having a voice that is heard nationally, and it we are going to make strides in changing attitudes and perceptions”
“It means we’re not re-inventing the wheel, we can draw on the experiences of other groups. It gives us heart that someone is trying to pull it all together.”
“Being part of a network gave our members the confidence that they have a right to have their voices heard.”
“When I arrived at EDUCATE – I thought ‘I could never do that’, seeing people talking openly to each other about dementia. I was still shocked about my diagnosis, crying and feeling very sorry for myself. But now, look at me! I’m giving talks, I’ve been on the telly and the radio, I’m having a good life – and all because of this group.”
(members of a DEEP groups cited in Litherland, 2015)
The groups of people living with dementia involved in DEEP have come together at two national conferences23 and been involved in lobbying Government ministers, talking to the media about dementia, being on the advisory groups for dementia projects, speaking at conferences including the 2016 ImROC national conference, (Educate gave a presentation at the conference but did not use a full set of slides. More information is on their website: www.educatestockport.org.uk/)and giving talks to those who work with people with dementia (Williamson, 2012). By connecting local groups and individual activists through a national network that engages and empowers, people living with the diagnoses are beginning to set priorities and shape political agendas (Litherland, 2015). Having an influencing role has benefits for the individuals involved (Litherland, 2015):
- Creating a sense of solidarity, building confidence, empowerment and increased self-esteem.
- Improving health and wellbeing.
- Enabling people to ‘give back’, to leave a legacy.
- Improving services, helping to spend money on the services that people need and want.
- Using people’s skills and their unique expertise of ‘lived experience’.
- Seeing and hearing ‘real people’ can challenge stereotypes.
- People have a role, are occupied and maintain a sense of value and purpose.
Collectively, DEEP members have produced a number of DEEP guides24 (including one offering guidance on setting up a new group25) designed to support the involvement of people with dementia. Some of these were created for groups and individuals with dementia (for example, travelling with dementia, enhancing communication and using sound and film to hear the voices of people with dementia) and some for organisations wanting to work well with people who live with dementia (for example, guidelines on language about dementia, writing dementia-friendly information and involving people with dementia in various settings including advisory groups, the development of Dementia Friendly Communities, staff recruitment and research).
In summarising the learning from the Dementia Engagement and Empowerment Project, Litherland (2015) concludes that:
- Involvement is not just about consulting people with dementia, but about providing and responding to opportunities for them to shape their own agendas.
- Local groups are where most people with dementia get support to find their voices.
- Health, social and political bodies should involve people with dementia in setting priorities.
- Appropriate funding of local groups is essential to broker the relationship between people with dementia and decision-makers.
- Local organisations, commissioners and decision-makers are key allies for groups.
- People with dementia often feel they have a ‘window of opportunity’ to be involved, and therefore need to see results from the energies they put into being involved.
- There is a need for mechanisms that support people with dementia to carry on contributing as their needs change, and to ensure that a range of people with dementia, including those with more advanced dementia, can have their voices heard.
Conclusions: Changing the narrative
“I’m living with Dementia, not dying from Dementia.” (Ashley 2002)
If people who receive a diagnosis of some form of dementia are to ‘continue to be me’ – recover a valued, meaningful and satisfying life – then many things are important, but most of all we need to change the narrative.
From ‘victims’ to be pitied and cared about, to ‘citizens’ with rights who can and should speak for themselves. Like other citizens, people may need support to do this. Like other disabled people, those living with dementia have a right to a voice and a right to the adjustments and support they need to participate: rights enshrined in the Equality Act and United Nations Convention on the Rights of Persons with Disabilities.
From a ‘living death’ to a ‘life’. Life changes, but life goes on and that life can be a good life. Images of possibility are central to living well with dementia26. As James McKillop of the Scottish Dementia Working Group says, (in O’Hara, 2008) the typical image of someone with dementia is of someone who can do nothing for themselves and is completely unable to communicate their wishes and preferences.
“If you take a positive outlook and are determined to get on with life as best you can, I think you will be pleasantly surprised at what you can achieve …you will still be able to do many things you did before by yourself, and others you will be able to manage with a little assistance. You may even find time to return to old hobbies or to learn to do things you always wished you’d had time for. It is a time for opportunity which you should grab with both hands.” (James McKillop in Mental Health Foundation, 2011)
Relatives and friends must also face the challenge of dementia, and while supporting someone with dementia can be exhausting and painful at times, many people have also said that it can be rewarding.
“They have dementia, but most things are possible with a little planning. Continue to socialise, go shopping or for a drink – my wife still goes to weddings and parties with me, and she has a smashing time. After I had a heart attack some years ago, my wife nursed me for two years and now I’m nursing her in return. Often she takes my hand and tells me she loves me and I get a lot of satisfaction out of seeing her happy. It’s not always easy being a carer, but it is rewarding.” (Joe McCall in Mental Health Foundation, 2011a)
“One family we support are mostly confined to one room and have little life beyond the dinner
plate and the commode. However, between periods of harsh words, they (the person with
dementia and her family) shower each other with love and affection. I think this keeps them
all going and will be the defining memory of this experience.” (Mike Chappell, Compass
Worker Lead)
Living with dementia is not easy, but both people living with the diagnosis and the family and friends who support them have identified positive things that can be drawn from the experience (see Mental Health Foundation 2011, 2011a)
- The satisfaction of surviving and succeeding in the face of adversity.
- Becoming emotionally closer through sharing the experience of dementia with them.
- Meeting new people who are going through similar experiences.
- The realisation that every day is precious, and that even though things may have changed you can still enjoy happy times.
“My caring experience gave me confidence in my abilities (if I can do that, I can do other difficult stuff), and having the opportunity to use these experiences to help other carers, and by extension people with dementia, has been one of the greatest gifts from my dad.”
(Mike Chappell, Compass Worker Lead talking about his father)
References
Adams, T. (2010) ‘The applicability of a recovery approach to nursing people with dementia’, International Journal of Nursing Studies, 47(5), 626-634
Alakeson, V. and Perkins, R. (2012) Recovery, Personalisation and Personal Budgets, ImROC Briefing Paper, London: Centre for Mental Health/NHS Confederation
Alzheimer’s Society (2013) Dementia 2013:The hidden voice of loneliness, London: Alzheimers Society https://www. alzheimers.org.uk/site/scripts/download_info. php?fileID=1677
Alzheimer’s Society. (2005) Caring for someone with dementia: Communicating, London: Alzheimer’s Society http://www. alzheimers.org.uk/Caring_for_someone_ with_dementia/Maintaining_quality_of_life/ advice_communication.htm
Anthony, W. A. (1993). Recovery from mental illness: The guiding vision of the mental health service system in the 1990’s. Psychosocial Rehabilitation Journal, 16(4), 11-23
Ashley.P. (2002) Now you see it now you don’t. London: Alzheimer’s Society, London.
Bailey, S.J., Partridge, J., Hill, L. & Dhesi, J. Loneliness in older age: a risk factor for ill health, Geriatric Medicine, June 2015, 47-51
Bowers, H., Bailey, G., Sanderson, H., Easterbrook, L. &Macadam, A. (2007) Person Centred Thinking and Older People – Practicalities and Possibilities, Helen Sanderson Associates
Brooker, D. (2004) ‘What is person-centred care in dementia?’, Reviews in Clinical Gerontology, 13(03), 215-222
Brooker, D. and Surr, C. eds (2005) Dementia Care Mapping: Principles and Practice. Bradford Dementia Group: University of Bradford.
Caddell, L. S. and Clare, L. (2011) ‘I’m still the same person: The impact of early-stage dementia on identity’, Dementia, 10(3), 379- 398
Care Services Improvement Partnership (2005) Everybody’s Business Integrated mental health services for older adults: a service development guide, London: Department of Health
Care Services Improvement Partnership (2007) Strengthening the Involvement of People with Dementia, London: CSIP Oder People’s Mental Health Programme
Carper, J. (2011b) 100 Simple Things You Can Do To Prevent Alzheimer’s and AgeRelated Memory Loss. London: Ebury Press
Chamberlin, J. (1977) On Our Own, edition published by MIND in 1988, London: MIND
Cheffey, J., Hill, L., Roberts, G. & Marlow, R. (2013) Supporting self-management in early dementia: a contribution towards ‘living well’? Advances in Psychiatric Treatment ,19, 344–350 doi: 10.1192/apt.bp.112.011023
Cheffey, J., Hill, L., McCullough, C., & McCullough C. (2016 – in press) Can I facilitate a project when my memory lets me down? The Challenges and rewards of co-producing and ‘Living Well with Dementia’ course. FPOP Faculty for the Psychology of Older People
Clarke, C.L., Keyes, S.E., Wilkinson, H., Alexjuk, J., Wilcockson, J., Robinson, L., Reynolds, J., McClelland, S., Hodgson, P., Corner, L. and Cattan, M. (2013) HEALTHBRIDGE: The National Evaluation of Peer Support Networks and Dementia Advisers in implementation of the National Dementia Strategy for England [Ref: 025/0058], Department of Health Policy Research Programme Project
Copeland, M.E. (1997) Wellness Recovery Action Plan, www.mentalhealthrecovery.com
Crampton, J., Dean, J., & Ely, R. (2012) Creating a Dementia Friendly York, York: Joseph Rowntree Foundation
Daley, S., Newton, D., Slade, M., Murray, J. & Banerjee, S. (2013) Development of a framework for recovery in older people with mental disorder, International Journal of Geriatric Psychiatry, 28, 522–529
Davidson, S. & Rosall, P. (2014) Evidence Review: Loneliness in Later Life, London: Age UK
Deegan, P. (1988) Recovery: The lived experience of rehabilitation, Psychosocial Rehabilitation Journal, 11: 11-19
Deegan, P.E. (1996). Recovery as a Journey of the Heart. Psychiatric Rehabilitation Journal 19, 3, 91–97
Dementia Action Alliance (2010) National Dementia Declaration. London: Dementia Action Alliance http://www.dementiaaction. org.uk/nationaldementiadeclaration
Department of Health (2009) Living well with dementia: A National Dementia Strategy. London: Department of Health
Department of Health (2012) Personal health budgets and NHS Continuing Healthcare. London Department of Health
Fletcher, V. (2010) Take a walk to keep dementia at bay. Express, 14 October
Hill, L., Cheffey, J. McCullough & McCullough 2016 – in press
Hill, L., Roberts, G., Wildgoose, J., Perkins, R. & Hahn, S. (2010) Recovery and personcentred care in dementia: common purpose, common practice? Advances in Psychiatric Treatment, 10, 288-298
Holt-Lunstad J, Smith TB, Layton JB (2010) Social Relationships and Mortality Risk: A Meta-analytic Review. PLoS Med 7(7): e1000316. doi:10.1371/journal. pmed.1000316
Holt-Lunstad, J., Smith, T. and Layton, J.B. (2010) ‘Social relationships and mortality risk: a meta-analytic review’, PLoS Medicine, vol 7, no 7, doi:10.1371/journal.pmed.1000316
Holwerda, T.J., Deeg, D.J., Beekman, A.T., van Tilburg, T.G., Stek, M.L., Jonker, C., & Shoevers, R.A. (2014) Feelings of loneliness, but not social isolation, predict dementia onset: Results from the Amsterdam Study of the Elderly (AMSTEL), Journal of Neurological and Neurosurgical Psyychiatry, 85(2): 135-142
Janet Crampton, J., Dean, J., & Eley, R. (2012) Creating a dementia friendly York, York, Joseph Rowntree Foundation
Jordan. R.E., Majothi, S., Heneghan, N.R., Blissett, D.B., Riley, R.D., Sitch, A.J., Price, M.J., Bates, E.J., Turner, A.M., Bayliss, S., Moore, D., Singh, S., Adabm P., Fitzmauricem D.A., Jowett, S., and Jolly, K. (2015) Supported self-management for patients with moderate to severe chronic obstructive pulmonary disease (COPD): an evidence synthesis and economic analysis. Health Technology Assessment, 19(36)
Joseph Rowntree Foundation (2015) Dementia without walls https://www.jrf.org.uk/ dementia-without-walls
Kitwood TM (1997) Dementia Reconsidered. The Person Comes First. Open University Press.
Lintern, T., Woods, B.., & Phair, L. (2000). Before and after training: a case study of intervention. Journal of Dementia Care, 8(1), 1 -17
Litherland, R. (2015) Developing a national user movement of people with dementia. Learning from the Dementia Engagement and Empowerment Project (DEEP), York: Joseph Rowntree Foundation
Local Government Association and Innovations in Dementia (2012) Developing dementia friendly communities. Learning and guidance for local authorities, London: Local Government Association
Manthorpe J, Samsi K, Campbell S, Abley C, Keady J, Bond J, Watts S, Robinson L, Gemski, Warner J, Goodman C, Dreenan V, Iliffe, 2011, The Transition from cognitive impairment to dementia: older people’s experiences, NIHR Service Delivery & Organisation Programme
McGettrick, G. and Williamson, T. (2015) Dementia, rights and the social model of disability, London: Mental Health Foundation
McKay, R., McDonald, R., Lie, D. and McGowan, H. (2012) ‘Reclaiming the best of the biopsychosocial model of mental health care and ‘recovery’ for older people through a ‘person-centred’ approach’, Australasian Psychiatry, 20(6), 492-5
McKeown, J., Clarke, A. and Repper, J. (2006) The Use of Life Story Work within Health and Social Care Practice: A Systematic Literature Review. Journal of Advanced Nursing 55 (2):237-247
Mental Health Foundation (2005) Still Going Strong. London: Mental Health Foundation.
Mental Health Foundation (2011) Still Going Strong. A guide to living with dementia, London: Mental Health Foundation https:// www.mentalhealth.org.uk/sites/default/files/ Download_StillGoingStrong.pdf
Mental Health Foundation (2011a) Becoming a Carer. A booklet about looking after someone with Dementia. London: Mental Health Foundation https://www.mentalhealth. org.uk/publications/becoming-carer
Morley, A., Redburn, D., Jennison, W., Mascall, J., Fryer, J., Sanderson, H. & Bailey G. (2010) Using Person-centred Thinking to implement Dementia Care Mapping, Helen Sanderson Associates http:// www.helensandersonassociates.co.uk/wpcontent/uploads/2015/03/DCM.pdf
Morley, A., Redburn, D., Jennison, W., Mascall, J., Fryer, J., Sanderson, H., Bailey, G. (2010)
O’Hagan, M. Madness Made Me. Wellington, New Zealand: Open Books.
O’Hara, M. (2008) Brigding the gap, The Guardian, 6th February 2008 http://www. theguardian.com/society/2008/feb/06/ longtermcare.socialcare
Oliver, M (2004). If I had a hammer: the social model in action. In: J. Swain, S. French, C. Barnes and C. Thomas, (eds). Disabling Barriers – Enabling Environments. SAGE, London
Peel, E. (2014) ‘The living death of Alzheimer’s’ versus ‘Take a walk to keep dementia at bay’: representations of dementia in print media and carer discourse. Sociology of Health & Illness. 36(6), 885–901
Perkins, R. (2013) Recovery in Later Life. Recovery and Recovery-focused Practice in Services for Older People with Complex Needs and Dementia, presentation at Norfolk and Suffolk Mental Health Trust, 9th December 2013
Perkins, R. (2014) Living well with dementia. Recovery focused practice in services for people with dementia, presentation at Richmond Fellowship Western Australia, Perth 15th May 2014.
Pratchett, T. (2008) ‘I’m slipping away a bit at a time… and all I can do is watch it happen’, The Daily Mail, 7th October 2008
Pratt, R. & Wilkinson, H (2001) ‘Tell Me The Truth’ The effect of being told the diagnosis of dementia from the perspective of the person with dementia. London: Mental Health Foundation/Stirling: Centre for Social Research on Dementia, University of Stirling
Pullman, P. (2006) quoted in R. Little ‘True stories to feed the heart with hope’, The Oxford Times, 6th April 2006
Rachman, S. (1980) Emotional processing, Behaviour Research and Therapy, 18(1), 51-60
Rachman, S. (1980). Emotional processing. Behaviour Research & Therpay, 18, 51-60
Repper, J. and Perkins, R. (2012) Recovery: A journey of Discovery for Individuals and Services. In: Phillips, P., Sandford, T. and Johnston, C. (eds.) Working in Mental Health: Practice and Policy in a Challenging Environment. Oxford: Routledge.
Repper, J., Perkins, R. & Meddings,S. (2013) A personal health and wellbeing plan for family, friends and carers, London: ImROC
Repper, J.M. & Perkins, R.E. (2003) Social Inclusion and Recovery: A Model for Mental Health Practice. London: Balliere Tindall .
Revoir, P. (2011) The living death of Alzheimer’s. Daily Mail, 26 April
Shepherd, G., Boardman, J., & Slade, M. (2008) Making Recovery a Reality. London: Sainsbury Centre for Mental Health.
Smith, E. speaking at the Changing Melody Forum, a Canadian event for and by people with dementia (2003) http://www.google.co.uk/url?sa=t&rct=- j&q=&esrc=s&source=web&cd=1&ved=0CCEQFjAA&url=http%3A%2F%2Fwww. dasninternational.org%2F2006%2FCanadians%2520with%2520Dementia%2520Fight%2520to%2520WinFinal. doc&ei=mnX8U5WiLdDb7Aac0IGwCA&usg=AFQjCNGLj3YbE3lBnsvnKQ6EdjOvh6alJw&bvm=bv.73612305,d.ZGU
Social Care Institute for Excellence (2011) Preventing loneliness and social isolation: interventions and outcomes, Research briefing 39, London: Social Care Institute of Excellence
Social Care Institute of Excellence (2003) Assessing the mental health needs of older people. Adults’ Services: SCIE
Guide 03, London: SCIE South London and Maudsley NHS Foundation Trust and South West London and St George’s Mental Health NHS Trust (2010) Recovery is for All. Hope, Agency and Opportunity in Psychiatry. A Position Statement by Consultant Psychiatrists. London: SLAM/SWLSTG.
South London and Maudsley NHS Foundation Trust and South West London and St George’s Mental Health NHS Trust (2010) Recovery is for All. Hope, Agency and Opportunity in Psychiatry. A Position Statement by Consultant Psychiatrists. London: SLAM/SWLSTG
Spector, A., & Orreii, M. (2006). Quality of Life (QoL) in Dementia: A Comparison of the perceptions of people with Dementia and care staff in Residential Hom s. Alzheimer Disease and Associated Disorders, 20, 160-165
The Health Foundation (2015) Shine 2014 final report: A Study of the Use of SelfManagement Techniques in Patients with Mild Cognitive Impairment, Devon Partnership Trust, Sept 2015
Think Local Act Personal (2013) MAKING IT REAL for people with dementia, London: TLAP
Williamson, T. (2012) A stronger collective voice for people with dementia, York: Joseph Rowntree Foundation
Wilson, R.S., Krueger, K.R., Arnold. S.E., Schneider, J.A., Kelly, J.F, Barnes LL, et al. (2007) Loneliness and risk of Alzheimer disease. Archives of General Psychiatry, 64(2):234-240
Woods, R. (2007) Recovery—is it relevant to older people? Signposts.12 (1), 2-3
Zimmermann, S., Sloane, P D., Williams, C. S., Reed, P. S., Preisser, J. S-, Eckert, J. K., Boustani, M., & Dobbs, D. (2005). Dementia care and quality of life in assisted living and nursing homes. Gerontologisf, 45 (Special lssue 1), 133-146
Rachel Perkins, ImROC Senior Consultant, Co-editor of Mental Health and Social Inclusion, Deputy Chair of the Equality and Human Rights Commission Disability Committee
Laura Hill, Consultant Psychiatrist, Older People’s Mental Health, Devon Partnership NHS Trust
Stephanie Daley, Clinical Research Fellow, Centre for Dementia Studies, Sussex Partnership Foundation Trust
Mike Chappell, Compass Worker27 Lead, Nottinghamshire Healthcare NHS Foundation Trust
Jane Rennison, Recovery Lead and Head of Occupational Therapy, Central and North West London Foundation NHS Trust
With the assistance of Patricia Witherden, Dementia Peer Support Worker, and the Kensington and Chelsea Memory Group who shared with us the expertise of their experience on living well with dementia and assisted in the development of Recovery Workshops within Central and North West London NHS Trust older adults service that contributed to the development of this briefing paper.
1 From Daley et al (2013)
2 All boxed quotes in this briefing paper are the words of people living with dementia – individuals with the diagnosis and their relatives – describing their experiences.
3 http://www.which.co.uk/elderly-care/your-relatives-needs/tackling-loneliness/386429-causes-of-loneliness-in-older-people
4 See, for example, Social Care Institute for Excellence ‘Getting to know the person with dementia: the impact of diagnosis’ http://www.scie.org.uk/publications/dementia/resources/video-player.asp?v=gettingtoknowthepersonwithdementia
5 http://philosiblog.com/2013/07/31/life-isnt-about-waiting-for-the-storm-to-pass-its-about-learning-to-dance-in-the-rain/ accessed 14.3.2016
6 All boxed quotes in the text are the words of people who are living with a diagnosis of dementia.
7 https://hee.nhs.uk/sites/default/files/documents/Time%20For%20Dementia%20programme.pdf
http://www.sussexpartnership.nhs.uk/whats-new/time-dementia-2
8 http://dementiavoices.org.uk/wp-content/uploads/2015/03/DEEP-Guide-Language.pdf
9 See, for example, Sussex Recovery College https://www.sussexrecoverycollege.org.uk/courses/12-west-sussex/199-livingwith-dementia; Barnsley Recovery College http://www.southwestyorkshire.nhs.uk/wp-content/uploads/2014/05/BarnsleyRecovery-College-prospectus-Sept-2014-July-2015.pdf Devon Recovery Learning Community http://www.devonpartnership. nhs.uk/fileadmin/user_upload/images/enews/DAISY_Online_News/DRLC_Summer_2015_prospectus.pdf ; South London and Maudsley Recovery College http://www.slamrecoverycollege.co.uk/courses.html
10 See, for example, Mary Ellen Copeland who developed the original ‘wellness recovery action plans’ (WRAP) (www.mentalhealthrecovery.com) and Perkins, R. & Rinaldi, M. (2007) Taking Back Control. A guide to planning your own recovery, London: South West London and St George’s Mental Health NHS Trust.
11 See for example https://www.alzheimers.org.uk/site/scripts/documents_info.php?documentID=143
12 https://www.alzheimers.org.uk/site/scripts/download_info.php?downloadID=399
13 See Alzheimer’s Society 2005 and Care Services Improvement Partnership 2007 for tips to improve communication.
14 Developed by Professor Tom Kitwood http://www.bradford.ac.uk/health/dementia/dementia-care-mapping/ . See Brooker and Surr, 2005)
15 http://www.nhs.uk/choiceintheNHS/Yourchoices/personal-health-budgets/Pages/about-personal-health-budgets.aspx and https://www.alzheimers.org.uk/site/scripts/download_info.php?fileID=2640
16 Alzheimer’s UK ‘Dementia – the hidden voice of loneliness’ https://www.alzheimers.org.uk/site/scripts/documents_info.php?documentID=2164
17 See for example, https://www.mentalhealth.org.uk/projects/dementia-self-help-project
18 see http://dementiavoices.org.uk/deep-groups-alphabetical-order/ )
19 Recommendations and resources from the English Dementia Friendly Communities pilots can be found in http://www.local. gov.uk/ageing-well/what-makes/-/journal_content/56/10180/3489659/ARTICLE
20 see http://dementiavoices.org.uk/deep-groups-alphabetical-order/
21 An initiative managed by the Mental Health Foundation, Innovations in Dementia and Alzheimer’s Society and funded by the Jospeph Rowntree Foundation http://dementiavoices.org.uk )
22 http://dementiawithoutwalls.org.uk/2016/03/peer-support-crosses-all-borders/
23 A video from the DEEP conferences – People With Dementia Speak Out! – illustrating their work can be found at https://www. youtube.com/watch?v=mdqucRPRQTo
24 http://dementiavoices.org.uk/resources/deep-guides/
25 http://dementiavoices.org.uk/2016/01/setting-up-a-new-guide-deep-guide/
26 See, for example, http://www.scie.org.uk/dementia/resources/video-player.asp?v=gettingtoknowthepersonwithdementia
27 Compass Workers are Carer Peer Support Workers: people who have their own experiences of providing care and support for a relative/friend living with a diagnosis of dementia who are paid to provide peer support to other carers of people with moderate to severe dementia living at home. They provide emotional support and mentoring, and can often act as a bridge between carers and services by helping people to navigate the maze of services and supports available. They also provide support after a move into care and support after bereavement.
